-
PDF
- Split View
-
Views
-
Cite
Cite
Esha Vaid, Amy Hughes Lansing, Catherine Stanger, Problems With Self-Regulation, Family Conflict, and Glycemic Control in Adolescents Experiencing Challenges With Managing Type 1 Diabetes, Journal of Pediatric Psychology, Volume 43, Issue 5, June 2018, Pages 525–533, https://doi.org/10.1093/jpepsy/jsx134
Close - Share Icon Share
Abstract
This study explored the associations between problems with self-regulation and glycemic control (HbA1c) in teens experiencing challenges with managing type 1 diabetes by examining greater diabetes-related family conflict and poorer adherence as serial mediators of the link between greater problems with self-regulation and higher HbA1c.
Teens experiencing challenges with managing type 1 diabetes (n = 93, HbA1c ≥8%, 96% White, 57% male) completed an HbA1c test, and their parents completed assessments including measures of adherence and family conflict related to diabetes management during an intake for a larger Web-based intervention study or fMRI study. Teen problems with self-regulation were indexed the Child Behavior Checklist using the dysregulation profile.
Bivariate correlations found significant associations between greater problems with self-regulation, greater family conflict about diabetes management, poorer adherence, and higher HbA1c. However, only greater family conflict, and not adherence, significantly explained the association between greater self-regulation problems and higher HbA1c.
These findings suggest that among teens experiencing challenges with managing type 1 diabetes, interventions that decrease family conflict may be critical to promoting optimal glycemic control in those teens with greater problems with self-regulation.
Among adolescents with type 1 diabetes, nearly 75% evidence glycemic control that does not meet clinical guidelines (Wood et al., 2013) and this above-target glycemic control contributes to multiple negative health outcomes including premature mortality (Kakleas, Kandyla, Karayianni, & Karavanaki, 2009). Management of type 1 diabetes in adolescence is a challenging daily task requiring repeated blood glucose monitoring, multiple daily insulin dosing, and careful carbohydrate counting. Optimal diabetes management in adolescence requires not only good self-regulation skills, but also benefits from the involvement of family caregivers (Berg et al., 2013; Berg, Hughes, et al., 2014; Berg, Queen, et al., 2016; Lansing, Berg, Butner, & Wiebe, 2016). Research examining self-regulation and diabetes management in youths has emphasized the contributions of self-regulation to individual processes such as goal setting, problem-solving, and affect regulation (Hughes, Berg, & Wiebe, 2012; Lansing, Berg, et al., 2016; McNally, Rohan, Pendley, Delamater, & Drotar, 2010). Yet, despite developmental theory frequently linking self-regulation and family processes (Repetti, Taylor, & Seeman, 2002; Rothbart, Posner, & Kieras, 2006), there has been limited research examining the intersection of self-regulation and family functioning in adolescent diabetes management (Berg, Queen, et al., 2016). Further, although family conflict about diabetes management has been repeatedly associated with above-target glycemic control (Hilliard, Wu, Rausch, Dolan, & Hood, 2013; Ingerski, Anderson, Dolan, & Hood, 2010), it has not been examined as a mechanism linking problems with self-regulation to poor adherence and glycemic control. Exploring additional mechanisms that might link problems in self-regulation with poorer adherence and glycemic control, especially in youth with challenges managing type 1 diabetes, is needed to inform the tailoring of interventions to promote more optimal diabetes outcomes.
Problems with self-regulation are key contributors to nonadherence and challenges in maintaining optimal glycemic control in adolescents with type 1 diabetes. Self-regulation is defined as the ability to modulate behavior, emotion, and cognition toward a goal (Finkenauer, Engels, & Baumeister, 2005) and is a broad construct that encompasses numerous constructs, for example, self-control, cognitive control, executive function, and effortful control, many of which have been examined in adolescents with type 1 diabetes. For example, research has found that problems with self-regulation predicted poorer adherence and worse daily blood glucose control (Berg, Wiebe, et al., 2014; Lansing, Berg, et al., 2016). Also, multiple studies have found repeated associations between stronger executive function skills and better adherence and glycemic control in youth with type 1 diabetes (Bagner, Williams, Geffken, Silverstein, & Storch, 2007; Duke & Harris, 2014; McNally et al., 2010; Miller et al., 2013). Across this research, the link between problems in self-regulation and poorer adherence is theorized to occur owing to impairments in behavioral self-regulation required for adolescents to independently complete complex daily adherence behaviors. However, this research has yet to examine how family functioning might also contribute to explaining the link between adolescent problems with self-regulation and disease self-management and outcomes.
Individual differences in problems with self-regulation in adolescence may also be associated with impairments in family functioning and greater risk for poor outcomes. Problems with self-regulation in children emerge from a complex and transactional biopsychosocial developmental process that intricately links self-regulation and family functioning (Blair & Raver, 2015; Bradford, Vaughn, & Barber, 2008; Frankel et al., 2012; Kim et al., 2012; Pardini, Fite, & Burke, 2008; Zeman, Cassano, & Perry-Parrish, 2006). However, individual differences in problems with self-regulation that emerge earlier in childhood remain relatively stable in predicting outcomes later in life (Hay & Forrest, 2006; Raffaelli, Crockett, & Shen, 2005). For example, self-control at age 5 predicts health, wealth, and criminality in adulthood (Moffitt et al., 2011). So, although self-regulatory capacity continues to mature across adolescence and into emerging adulthood, including via transactional associations with family and social processes, the stability of problems with self-regulation allows for consideration of how problems with self-regulation in adolescence contribute to other family and developmental outcomes. For example, increased teen problems with self-regulation may be associated with impaired family functioning, including high levels of family conflict, and greater negative developmental outcomes (Zeman et al., 2006).
Among adolescents with type 1 diabetes, increased family conflict as a mediator of the link between problems with self-regulation and diabetes outcomes (e.g., adherence and glycemic control) has yet to be examined. Supporting the importance of considering family conflict as a mediator of the link between problems with self-regulation and diabetes outcomes in youths with type 1 diabetes, there is ample evidence linking family conflict about diabetes with adherence and glycemic control. Research has repeatedly found that higher levels of family conflict are associated with poorer adherence and glycemic control (Anderson et al., 2002; Duke et al., 2008; Hilliard et al., 2013; Ingerski, Anderson et al., 2010; Smith, Dishion, Moore, Shaw, & Wilson, 2013). Longitudinal studies have found that greater family conflict about diabetes management is prospectively associated with later decreases in adherence behaviors and in turn above-target glycemic control. Further, greater adolescent externalizing behaviors, often an indicator of problems with self-regulation, have been associated with increased family conflict about diabetes (Duke et al., 2008). Consistent with both developmental and type 1 diabetes research, it was hypothesized that greater problems in self-regulation would be associated with greater family conflict about diabetes management and that would, in turn, be associated with poorer adherence and worse glycemic control.
In addition, although longitudinal research supports that increased family conflict leads to above-range glycemic control by decreasing adolescence adherence to the medical regimen, there is also emerging evidence that family conflict may be associated with glycemic control through additional processes beyond impairing youths’ adherence. For example, Herzer, Vesco, Ingerski, Dolan, and Hood (2011) found that the link between family conflict and glycemic control was not mediated by level of adherence, but by increased youth anxiety. The mechanism for this link has not yet been identified in youth with diabetes; however, stressful family environments, including those with high family conflict, have been associated with impairments in youths’ biological stress regulatory systems (Repetti et al., 2002). Changes in the stress regulatory system have far-reaching influences on health and may serve as a physiological mechanism that links family conflict to glycemic control outside of adherence behaviors. Thus, it was also hypothesized that problems with self-regulation might be linked with glycemic control through family conflict alone as well as through both family conflict and adherence.
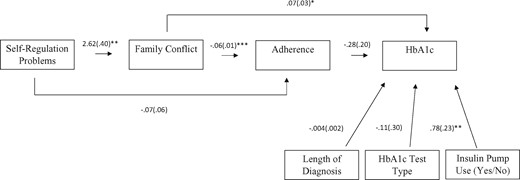
In this study, we examined problems with self-regulation, family conflict, adherence, and glycemic control in a sample of youths experiencing challenges with managing type 1 diabetes. It was hypothesized that the link between problems with self-regulation and glycemic control (HbA1c) would be explained by three indirect effects (Figure 1). First, it was hypothesized that problems in self-regulation would be associated with higher HbA1c, in part, serially through increased family conflict and poorer adherence. Second, it was hypothesized that problems in self-regulation would also be associated with poorer adherence and in turn higher HbA1c, outside of associations with family conflict. Third, it was also hypothesized that problems in self-regulation may be associated with increased family conflict and in turn higher HbA1c, outside of associations with adherence.
Greater problems with self-regulation are associated with glycemic control (HbA1c) through greater family conflict about diabetes management.
Methods
Participants
Participants for this study included 93 teenagers (43% female, 96% White, 62% pump, M age = 15.12 years, SD = 1.40, average length of diagnosis = 6.15 years, SD = 3.46) recruited from two clinical sites affiliated with an academic medical center children’s hospital. Inclusion criteria were the following: teens aged 13–17, type 1 diabetes diagnosis >15 months prior, average glycated hemoglobin percentage (HbA1c) ≥ 8% for the past 6 months and most recent HbA1c ≥ 8%, as well as broadband Internet and a computer at home (to allow participation in web-delivered treatment). Exclusion criteria included pregnancy and severe medical or psychiatric illness. Participants were recruited from the same clinics for studies on adolescent diabetes management that all followed the same intake procedures. The first study examined a Web-delivered intervention targeting adherence in adolescents with above-target glycemic control (n = 76 in current study; 201 families were screened, 94 did not enroll, and 31 were not eligible). The second study was an functional Magnetic Resonance Imaging (fMRI) study with an option to complete a similar Web-based intervention (n = 17 in current study; 111 families were screened, 54 did not enroll, 40 were not eligible, mostly owing to HbA1c < 8% or braces/metal in body which prevented fMRI). Overall, our sample consists of 93 adolescents, and this study used data collected before any intervention participation. On average, families were middle class based on the Hollingshead nine-step scale for parental occupation (M = 6.20, SD = 1.86). This study was conducted in compliance with the college’s institutional review board. There is no missing data to report.
Procedure
Intake assessments were conducted in the pediatric endocrinology department or a study office centrally located in the region. The study was explained to parents or guardians and adolescents, and parental or guardian consent and adolescent assent were obtained for all participants. At this intake, parents completed the study’s questionnaires using a Web-based system on a computer in the laboratory and teens completed a glycated hemoglobin test.
Measures
Problems in Self-Regulation
Youth problems with self-regulation was measured using parent report on the Child Behavior Checklist form (CBCL; Achenbach & Rescorla, 2001), a widely used and normed tool to assess behavioral and emotional problems in youths. The CBCL has demonstrated strong psychometric properties (Achenbach & Rescorla, 2001) and has been successfully used in youth with type 1 diabetes (Duke et al., 2008; Holmes, Respess, Greer, & Frentz, 1998; Strudwick et al., 2005). An index of problems with self-regulation of cognitions, emotions, and behaviors that draws on parent-reported data from the CBCL has been previously developed and validated (Althoff, Ayer, Rettew, & Hudziak, 2010; De Caluwé, Decuyper, & De Clercq, 2013; Jucksch et al., 2011; Masi, Pisano, Milone, & Muratori, 2015; Peyre, Speranza, Cortese, Wohl, & Purper-Ouakil, 2015). The problems with self-regulation index is calculated from item scores on three problem scales: (1) anxious/depressed, (2) attention problems, and (3) aggressive behavior. Specifically, the average item score (ranges from 0 to 2) on each of the scales were summed together, resulting in scores from 0 to 6, with higher scores indicating greater problems with self-regulation. This method weights problems on each syndrome scale equally, regardless of the number of items on the scale and captures broad deficits in self-regulation rather than emphasizing one particular syndrome scale. In further examination of this scale in our sample, all three syndrome scales loaded onto a single factor in a post hoc factor analysis (factor eigenvalue = 2.1, 71% of variance explained). Also, the Cronbach’s alpha for this scale indicated sufficient reliability (α= .73). In addition, further supporting the validity of this scale, in a subsample of the participants’ (n = 16) parents also reported on the Self-Control Scale (Tangney, Baumeister, & Boone, 2004), which was highly correlated with the CBCL problems with self-regulation scale (r = −.95, p < .01). Finally, while the measure was slightly positively skewed, the distribution was sufficiently normal for the analytic approach without transformations required (skew = .96; kurtosis = .25).
Diabetes-Related Family Conflict
Diabetes-related family conflict was assessed using parent report on the revised Diabetes Family Conflict Scale (DFCS) (Hood, Butler, Anderson, & Laffel, 2007). This measure includes two subscales, conflict on direct management tasks and conflict on indirect management tasks, and has been validated in samples of youths with type 1 diabetes (Hilliard, Guilfoyle, Dolan, & Hood, 2011; Müller-Godeffroy, Treichel, & Wagner, 2009; Wysocki et al., 2007). This study used the direct management tasks subscale (e.g., “During the past month, I have argued with my child about remembering to check blood sugars”), which has been most closely linked with diabetes self-management and glycemic control (Hood et al., 2007). The level of diabetes-related family conflict is rated on a 3-point scale (1 = never argue, 2 = sometimes argue, 3 = always argue) across nine direct diabetes management tasks. A total score, ranging from 9 to 27, is calculated, with higher scores indicating more conflict. Reliability for the DFCS Direct Management scale in this study sample was high (α = .87).
Self-Care Inventory
Adherence was measured via parent report on the Self-Care Inventory (SCI; Lewin et al., 2009). The SCI contains 14 items about adherence to important diabetes behaviors, such as blood glucose checking and administering the correct amount of insulin. Scores on the SCI were calculated by taking the average of scores across all 14 items. The validity of the SCI in adolescents with type 1 diabetes has been independently supported (Lewin et al., 2009), used validly in many studies (Berg et al., 2008; Berg, Butner, et al., 2016; Helgeson, Reynolds, Siminerio, Escobar, & Becker, 2008), and showed good reliability (α’s > .78). In this sample, reliability for parent report on the SCI was also good (α = .78).
Glycemic Control
HbA1c from a blood sample was used to measure glycemic control and was collected using two separate methods because one sample completed their baseline assessment away from the hospital in a laboratory research setting that limited the use of venous blood draws. For 76 youths, a venous blood draw was used and all samples were analyzed in the same central laboratory. For 17 youths, a point of care finger stick blood test was conducted. There was no significant difference in HbA1c based on the type of test conducted (t(20) = −0.49, p = .63). The distribution of HbA1c in this sample was such that 50% of participants had an HbA1c between 8 and 9, 31% between 9 and 10, and 19% >10. HbA1c serves as an indicator of glycemic control over the previous 3 months.
Analyses
Initial descriptive and Pearson correlation analyses for key study variables were conducted in SPSS v23. The hypothesized model (Figure 1) was tested through structural equation modeling and estimated using maximum likelihood with bias-corrected bootstrap confidence intervals for indirect effects in Mplus v.7.3. Fit indices for the overall model included Chi Square, comparative fit index (CFI), and root mean square error of approximation (RMSEA). Chi square p > .05, CFI > 0.9, and RMSEA < 0.05 indicated good model fit. This model was tested with multiple covariates included for glycemic control: insulin pump use, duration of diabetes diagnosis, and type of HbA1c test. In addition, the three hypothesized indirect effects were specified and tested in the model: (1) problems in self-regulation > family conflict > adherence > glycemic control; (2) problems in self-regulation > adherence > glycemic control; (3) problems in self-regulation > family conflict > glycemic control. A fourth indirect effect inherent within the first pathway of the model was also probed: problems in self-regulation > family conflict > adherence. Indirect effects were evaluated after considering the overall model fit. Finally, there was no missing data at intake, so no missing data procedures were required.
Results
Descriptive statistics and bivariate correlations are provided in Table 1. All key study variables were significantly correlated (r’s > .24) with greater problems with self-regulation, greater family conflict, poorer adherence, and higher HbA1c all associated. SES and age were not significantly associated with any of the key study variables. Further, t-tests examining teen gender differences for key study variables found no significant differences (problems with self-regulation: t(91) = −1.14, p = .26; family conflict: t(91) = −1.10, p = .27; adherence: t(89.20) = −0.14, p = .89; HbA1c: t(87.93) = −0.05, p = .96).
| Variables . | 1 . | 2 . | 3 . | 4 . | 5 . | M (SD) . | Range . |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | – | – | – | – | – | 9.24 (1.11) | 8.00–12.70 |
| 2. Family conflict | .36** | – | – | – | – | 15.90 (4.31) | 9.00–27.00 |
| 3. Self-care inventory | −.30** | −.51** | – | – | – | 3.25 (.54) | 2.14–4.43 |
| 4. Problems with self-regulation | .24* | .56** | −.36** | – | – | 1.07 (.91) | .00–3.71 |
| 5. SES (Hollingshead 9-step) | −.16 | −.20 | −.19 | −.01 | – | 6.20 (1.86) | 1.00–9.00 |
| 6. Age at intake | .07 | −.08 | −.20 | .02 | −.02 | 15.12 (1.40) | 13.02–17.68 |
| Variables . | 1 . | 2 . | 3 . | 4 . | 5 . | M (SD) . | Range . |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | – | – | – | – | – | 9.24 (1.11) | 8.00–12.70 |
| 2. Family conflict | .36** | – | – | – | – | 15.90 (4.31) | 9.00–27.00 |
| 3. Self-care inventory | −.30** | −.51** | – | – | – | 3.25 (.54) | 2.14–4.43 |
| 4. Problems with self-regulation | .24* | .56** | −.36** | – | – | 1.07 (.91) | .00–3.71 |
| 5. SES (Hollingshead 9-step) | −.16 | −.20 | −.19 | −.01 | – | 6.20 (1.86) | 1.00–9.00 |
| 6. Age at intake | .07 | −.08 | −.20 | .02 | −.02 | 15.12 (1.40) | 13.02–17.68 |
p < .05; **p < .01.
| Variables . | 1 . | 2 . | 3 . | 4 . | 5 . | M (SD) . | Range . |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | – | – | – | – | – | 9.24 (1.11) | 8.00–12.70 |
| 2. Family conflict | .36** | – | – | – | – | 15.90 (4.31) | 9.00–27.00 |
| 3. Self-care inventory | −.30** | −.51** | – | – | – | 3.25 (.54) | 2.14–4.43 |
| 4. Problems with self-regulation | .24* | .56** | −.36** | – | – | 1.07 (.91) | .00–3.71 |
| 5. SES (Hollingshead 9-step) | −.16 | −.20 | −.19 | −.01 | – | 6.20 (1.86) | 1.00–9.00 |
| 6. Age at intake | .07 | −.08 | −.20 | .02 | −.02 | 15.12 (1.40) | 13.02–17.68 |
| Variables . | 1 . | 2 . | 3 . | 4 . | 5 . | M (SD) . | Range . |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | – | – | – | – | – | 9.24 (1.11) | 8.00–12.70 |
| 2. Family conflict | .36** | – | – | – | – | 15.90 (4.31) | 9.00–27.00 |
| 3. Self-care inventory | −.30** | −.51** | – | – | – | 3.25 (.54) | 2.14–4.43 |
| 4. Problems with self-regulation | .24* | .56** | −.36** | – | – | 1.07 (.91) | .00–3.71 |
| 5. SES (Hollingshead 9-step) | −.16 | −.20 | −.19 | −.01 | – | 6.20 (1.86) | 1.00–9.00 |
| 6. Age at intake | .07 | −.08 | −.20 | .02 | −.02 | 15.12 (1.40) | 13.02–17.68 |
p < .05; **p < .01.
The full model examining the association of problems in self-regulation with glycemic control via indirect associations with family conflict and adherence (Figure 1) had good fit, with a nonsignificant Chi-square test, X2 (7) = 4.30, p = .74, CFI > 0.99, and RMSEA < 0.001, 90% CI [0, 0.09], and predicted 31% of variance in family conflict, 27% of variance in adherence, and 30% of variance in HbA1c. Problems with self-regulation had significant direct associations with family conflict (b = .56, p < .001, 95% CI [1.90, 3.45]) but not with adherence (b = −.07, p = .25, 95% CI [−0.19, 0.05]). Family conflict (b = .07, p = .02, 95% CI [0.01, 0.13]), but not adherence (b = −.28, p = .16, 95% CI [−0.65, 0.10]), had significant direct associations with HbA1c. Pump status was a significant predictor of HbA1c (b = −.78, p = .001, 95% CI [−1.23, −0.35]), while duration of diabetes (b = −.004, p = .11, 95% CI [−0.01, 0.000]) and type of HbA1c test (b = −.11, p = .70, 95% CI [−0.68, 0.48]) were not significantly associated with HbA1c.
Three primary indirect association pathways were examined to explore the mechanisms that might link problems with self-regulation and HbA1c. Only one path was supported, such that there was a significant indirect association of problems in self-regulation with higher HbA1c through greater family conflict (indirect association = 0.18, p = .03, 95% CI [0.03, 0.36]). There was not a significant indirection association of serially through family conflict and adherence (indirect association = 0.04, p = .17, 95% CI [−0.01, 0.10]).1 This was despite a significant indirect association of problems with self-regulation with adherence through family conflict (indirect association = −0.24, p < .001, 95% CI [−0.24, −0.08]). In addition, there was not a significant indirect association of problems with self-regulation and HbA1c through only adherence (indirect association = 0.02, p = .47, 95% CI [0.03, 0.36]). The link between adherence and HbA1c was not significant after accounting for all the predictors, such that only variance in family conflict significantly explained the association between problems with self-regulation and HbA1c.
Discussion
This study examined the association of adolescent problems in self-regulation with glycemic control through family conflict about diabetes and adherence. Out of the three pathways hypothesized, the only significant indirect pathway was through greater family conflict. Neither adherence alone nor adherence as a serial link between family conflict and out-of-range glycemic control explained the associations between self-regulation and glycemic control, despite bivariate associations among all of these variables. These findings suggest that in teens with challenges managing type 1 diabetes, family conflict about diabetes management explained the link between greater problems with self-regulation and above-target glycemic control. This highlights the likely importance of addressing family conflict about diabetes management to promote more optimal glycemic control in teens with type 1 diabetes who are experiencing problems with self-regulation.
Consistent with prior literature, this study’s findings supported bivariate associations among greater problems with self-regulation, poorer adherence, greater family conflict, and above-target glycemic control. For example, problems with self-regulation have been associated with adolescent adherence (Berg et al., 2014; Lansing, Berg, et al., 2016) and above-target glycemic control (Bagner et al., 2007; Duke & Harris, 2014; McNally et al., 2010; Miller et al., 2013). Greater family conflict has also been linked to poorer adherence and out-of-range glycemic control (Anderson et al., 2002; Duke et al., 2008; Hilliard et al., 2013; Ingerski, Anderson, et al., 2010; Smith et al., 2013), while among youths without diabetes, problems with self-regulation and family conflict have been linked (Blair & Raver, 2015; Frankel et al., 2012; Kim et al., 2012).
However, despite longitudinal research showing that greater family conflict predicted poorer adherence, which in turn predicted worsening glycemic control (Anderson et al. 2002; Duke et al., 2008; Ingerski, Anderson, et al., 2010; Hilliard et al., 2013; Moore et al., 2013), the current cross-sectional study did not support adherence as a mediator of the links between problems with self-regulation, family conflict, and glycemic control. A similar finding occurred in Herzer & Hood, (2010), another cross-sectional study, where increased anxiety, but not adherence, mediated the link between greater family conflict about diabetes and above-target glycemic control. This lack of an indirect effect via adherence may be occurring for multiple reasons: (1) the cross-sectional design; (2) owing to issues with the measurement of adherence and family conflict about diabetes management; and (3) owing to a separate pathway or intervening variable linking family conflict and glycemic control. First, the cross-section design may account for some of the unexpected nonsignificant findings, such that important transactional relations between family conflict, adherence, and HbA1c may be obscured by the stronger association of family conflict, compared with adherence, with HbA1c in this cross-sectional measurement approach. Second, measures of adherence and family conflict about diabetes management may explain similar variance in glycemic control, as much of family conflict may occur around instances or patterns of nonadherence. If measures of family conflict encompass both levels of nonadherence and family distress/functioning related to that nonadherence, they may predict variance in glycemic control uniquely from adherence. Further, the medium effect size (r = .3) between adherence and HbA1c in this study is similar to effect sizes between HbA1c and other measures of adherence examined in a meta-analysis (Hood, Peterson, Rohan, & Drotar, 2009). These small to medium effect sizes (0.20–0.30 in meta-analysis and 0.30 in this study) suggest that (1) improved measurement of adherence might be required to better understand adherence as a mediator of the links between problems with self-regulation, family conflict about diabetes management, and glycemic control, and (2) it is highly possible for another variable to explain variance in glycemic control above and beyond adherence, as family conflict does in our model. Finally, it may also be that greater family conflict links problems with self-regulation to glycemic control via other pathways in addition to adherence behaviors, such as changes in stress physiology that are evidenced in youths raised in risky family contexts (Repetti et al., 2002).
Limitations of this study should also be considered when interpreting results. The sample vastly comprised White, non-Hispanic, middle-class families, as the region and clinics the sample was recruited from had limited racial/ethnic diversity. This lack of representation of other races and ethnicities and low socioeconomic status families does not allow findings to be generalized to other populations. Additionally, this study restricted participation to adolescents with an HbA1c ≥ 8%, a requisite for participation in the intervention that followed this assessment. This inclusion criteria constrained the variability of HbA1c, which may limit power to identify significant findings and generalization of findings to adolescents with more optimal glycemic control. At the same time, owing to the limited number of participants with an HbA1c ≥10% in the sample, these findings may also not be specific to youths with more extreme problems in managing diabetes. Further, owing to the cross-sectional nature of this study, there was no temporal precedence for the measures. This was taken into consideration when exploring alternate pathway models; however, this study could not establish or test temporal precedence or causality of these processes in explaining glycemic control. The sample size was also small and future longitudinal studies with larger sample sizes would also be useful in testing more complex structural equation models, in particular models that examine demographic variables (e.g., gender, age, developmental status) that might moderate associations among self-regulation, family conflict, adherence, and glycemic control. The measure used to index problems with self-regulation was derived from an empirical measure of psychopathology and may better characterize risks of broad self-regulation problems linked directly to psychopathology rather than adherence and diabetes outcomes. Future studies should consider other measures that capture specific aspects of self-regulation such as cognitive, emotional, or behavioral self-regulation problems to examine if a specific deficit may be more relevant for family conflict, adherence, and glycemic control in adolescence than broad self-regulation problems. Finally, this study used reports by the primary caregiver only. Although neither parent nor teen reported adherence pathways were significant in our models, there are data to suggest that further clarity is needed in understanding self-reports and parent reports of adherence as they relate to HbA1c across time (Berg et al., 2016). Future studies would benefit from the use of multiple reporters to limit method variance and better understand how multiple caregivers’ perspectives on self-regulation and family conflict are associated with adherence and glycemic control.
There are multiple future research directions and clinical implications that can be drawn from this study. Future research should conduct longitudinal studies in samples of children and adolescents with type 1 diabetes with both at and above target range glycemic control and with greater ethnic diversity to clarify the links between problems with self-regulation, family conflict, adherence, and glycemic control across development. Also, targeting family conflict in interventions to promote optimal glycemic control when teens with type 1 diabetes have problems with self-regulation is an important area for future research. There are multiple evidence-based interventions for teens with type 1 diabetes that directly address family conflict that could be tested for this purpose including Diabetes Behavioral Family Systems therapy (Wysocki et al., 2008), Multisystemic Therapy for Diabetes (Ellis et al., 2005), and parent training to increase parental monitoring of diabetes management (Lansing, Stanger, Budney, Christiano, & Casella, 2016). Programs targeting executive functioning, a construct overlapping with self-regulation, could also be valuable in promoting self-regulation to reduce family conflict and improve glycemic control (Lansing, Stanger, et al., 2016; Perez et al., 2016; Wasserman, Hilliard, Schwartz, & Anderson, 2015). Finally, given that individual differences in self-regulation are largely stable by adolescence, preventive interventions targeting self-regulation in younger children diagnosed with type 1 diabetes may be particularly important to study. For example, educational programs that promote a balance between emotional and cognitive regulation have shown to be an efficacious prevention method to prevent problem behaviors’ negative psychosocial outcomes (Blair & Diamond, 2008).
Funding
This work was supported by a grant from the National Institute of Child Health and Human Development (grant number DP3 HD076602) and the National Institute on Drug Abuse (grant number P30 DA029926 to [C.S.]) (PI: Lisa A. Marsch).
Conflicts of interest: None declared.
Footnotes
An alternate model was also tested using teen-reported adherence on the same measure, rather than parent-reported adherence. While the model had good fit (X2 (7) = 3.03, p = .88, CFI = 1.00, and RMSEA < 0.001, 90% CI [0.0, 0.06]), the overall findings were the same as the a priori proposed model such that only family conflict explained the association between problems with self-regulation and HbA1c.
References
Author notes
Amy Hughes Lansing is now at the Department of Psychology, University of Nevada.



