-
PDF
- Split View
-
Views
-
Cite
Cite
Jennifer Reiter-Purtill, Marissa A. Gowey, Heather Austin, Kevin C. Smith, Dana L. Rofey, Todd M. Jenkins, Beth H. Garland, Meg H. Zeller, for the TeenView Study Group and in cooperation with Teen-LABS Consortium, Peer Victimization in Adolescents With Severe Obesity: The Roles of Self-Worth and Social Support in Associations With Psychosocial Adjustment, Journal of Pediatric Psychology, Volume 42, Issue 3, April 2017, Pages 272–282, https://doi.org/10.1093/jpepsy/jsw078
Close - Share Icon Share
Abstract
Objective To examine the associations of peer victimization with internalizing symptoms, externalizing symptoms, social competence, and academic performance in a clinical sample of adolescents with severe obesity, and whether self-worth and social support affect these associations. Methods Multisite cross-sectional data from 139 adolescents before weight loss surgery (Mage = 16.9; 79.9% female, 66.2% White; MBody Mass Index [BMI] = 51.5 kg/m2) and 83 nonsurgical comparisons (Mage = 16.1; 81.9% female, 54.2% White; MBMI = 46.9 kg/m2) were collected using self-reports with standardized measures. Results As a group, participants did not report high levels of victimization. Self-worth mediated the effects of victimization on a majority of measures of adjustment, and further analyses provided evidence of the buffering effect of social support for some mediational models. Conclusions Self-worth and social support are important targets for prevention and intervention for both victimization and poor adjustment in adolescent severe obesity.
Introduction
A recent study of public perceptions of weight bias using a multinational sample suggested that adults believed weight was the most common reason for bullying and teasing among youth (Puhl et al., 2016). Peer victimization is highly prevalent among youth who are overweight/obese (Haines, Neumark-Sztainer, Hannan, van den Berg, & Eisenberg, 2008; Janssen, Craig, Boyce, & Pickett, 2004), with some studies suggesting that risk increases with body mass index (BMI; Puhl, Peterson, & Luedicke, 2013). Peer victimization has been associated with internalizing and externalizing symptoms, poor self-concept, loneliness, and academic difficulties, both in the developmental literature (Copeland, Wolke, Angold, & Costello, 2013; Hawker & Boulton, 2000; Nakamoto & Schwartz, 2010; Prinstein, Boergers, & Vernberg, 2001) and in community and clinic-based studies of youth with overweight/obesity (Adams & Bukowski, 2008; Gray, Kahhan & Janicke, 2009; Gunnarsdottir, Njardvik, Olafsdottir, Craighead, & Bjarnason, 2012; Neumark-Sztainer et al., 2002; Puhl & Latner, 2007). These findings, coupled with evidence of a significant increase in levels of pediatric severe obesity (i.e., BMI ≥ 120% of the BMI-for-age 95th percentile) among youth in the United States (Skinner & Skelton, 2014), are concerning. Despite being a high-need population, the literature on the psychosocial comorbidities of adolescent severe obesity is in its infancy. Early evidence suggests that this group (BMI ≥ 99th percentile) may indeed present worse psychosocially than the obese counterpart (BMI = 95th to 98th percentile) (Phillips et al., 2012). However, there is also evidence of subgroups of youth with severe obesity reporting minimal psychopathology (Sysko, Zakarin, Devlin, Bush, & Walsh, 2011), including internalizing and externalizing symptoms (Rofey et al., 2015). Understanding this variability and identifying risk factors (e.g., victimization), as well as careful exploration of the mechanistic underpinnings and/or protective factors for adjustment, is imperative to intervention efforts.
Few studies have examined victimization specifically among adolescents with severe obesity. Preliminary evidence suggests that adolescents in residential treatment for severe obesity who report victimization and/or cyberbullying experienced greater psychological distress and more barriers to healthy lifestyle changes (DeSmet et al., 2014). Furthermore, limited research has examined potential mediators or moderators of the association of victimization with internalizing and externalizing symptoms and problems with social competence and academic performance among samples of youth who are overweight/obese. In the developmental literature, self-worth has been primarily identified as a mediator of peer victimization and difficulties, such as internalizing symptoms (Grills & Ollendick, 2002). Social information processing theory would posit that negative peer interactions such as experiences of victimization would lead some youth to develop negative self-perceptions (Crick & Dodge, 1994). These negative self-perceptions would in turn result in difficulties, particularly internalizing symptoms (e.g., anxiety; Grills & Ollendick, 2002) or less competent social behavior (i.e., withdrawn behavior, see Crick & Dodge, 1994). In contrast, the role of social support has been as a moderator, whereby social support provides protection against the damaging effects of life stressors (e.g., Moos, 2002). In particular, friendships (i.e., peer social support) have been found to provide a buffer against the effects of victimization, including the increase of internalizing and externalizing symptoms over time (Hodges, Boivin, Vitaro, & Bukowski, 1999). In the pediatric obesity literature, Adams and Bukowski (2008) found self-perceptions of appearance significantly mediated the association of victimization and depressive symptoms for a community sample of obese adolescent girls. Lim and colleagues (2011) demonstrated that peer social support appeared to moderate the associations of victimization and depressive symptoms for a clinical sample of obese girls, but not boys.
Victimization has been characterized as either direct such as overt victimization (i.e., physical aggression) or indirect such as relational victimization (i.e., social exclusion) and reputational victimization (i.e., damaging a person’s social reputation), and these types have been suggested to have different implications for understanding the victim (see Garandeau & Cillessen, 2006, Prinstein et al., 2001). No studies were identified that specifically examined the associations of these types of peer victimization (i.e., overt, relational, or reputational) on a diverse set of clinically important outcomes such as internalizing symptoms, externalizing symptoms, social competence (i.e., one’s perception of their own social behavior and acceptance), and academic performance for a sample of treatment-seeking adolescents with severe obesity, nor what factors might mediate or moderate those associations.
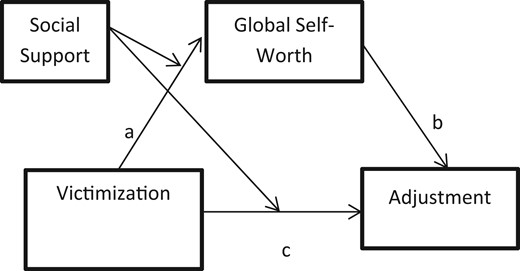
Conceptual model.
Note: “Victimization” could either be overt, relational, or reputational. “Adjustment” could be internalizing symptoms, externalizing symptoms, social competence, or academic performance. Pathways: a = (victimization type → global self-worth); Pathway b = (global self-worth → adjustment, with victimization type in the model), and Pathway c = (victimization type → adjustment with global self-worth in the model).
Methods
The present study used presurgical/baseline data from the TeenView study, which examines the psychosocial health of adolescents with severe obesity undergoing WLS. TeenView is an ancillary to the Teen Longitudinal Assessment of Bariatric Surgery consortium (Teen-LABS; NCT00474318), a prospective observational cohort study executed at five academic tertiary care centers in the United States to document the safety and efficacy of WLS in 242 adolescent patients (enrollment 2007–2011; Inge et al., 2007; Michalsky et al., 2014). Consecutive patients at each care center who were undergoing WLS were approached for Teen-LABS study participation. TeenView recruited two cohorts (enrollment 2008–2011): (1) Teen-LABS participants (“WLS”), and (2) demographically similar comparison adolescents with severe obesity in nonsurgical behavioral weight loss programs at the same five academic medical centers. TeenView was not designed as a comparative intervention trial (i.e., WLS vs. behavioral weight loss), but to examine psychosocial benefits and risks associated with adolescent WLS relative to a more “natural course” for adolescent severe obesity. The institutional review board at each institution approved study protocols.
Participants and Procedures
TeenView participants and procedures have been reported on previously (see Rofey et al., 2015; Zeller et. al., 2015) but are summarized below. Baseline/preoperative data from 222 TeenView adolescents and a caregiver were used. Eligibility criteria required that the Teen-LABS adolescent: (1) had a BMI ≥ 40 kg/m2; (2) was 13–18 years of age; (3) was not receiving full-time special education services owing to the high reading demand; (4) had a caregiver willing to participate; and (5) was able to speak/read English. Eligible participants were approached about TeenView participation during a presurgical clinic visit at each care center. Of the 159 eligible WLS participants, 14 declined and 4 (consented) were unable to participate before surgery, leaving 141 participating adolescents (recruitment: 88.7%). For sibling pairs (n = 2), the older sibling was excluded from analyses. In addition, one caregiver consented but did not complete forms before surgery, resulting in a final WLS cohort of 139 adolescents and 138 caregivers, who completed baseline data collection within 30 days before surgery.
NSComps were recruited from TeenView research registries that identified study eligible youth presenting at lifestyle modification programs at each care center and whose families agreed to be contacted for study enrollment should the adolescent become a demographic match (i.e., gender, race, ±6 months in age) to a WLS participant at any site. Once a family was identified as a potential match, they were contacted via phone and asked to participate in the study. During enrollment, 86 eligible NSComps were approached, of whom 3 declined, resulting in a final sample of 83 adolescents/caregivers (recruitment: 96.5%).
Assessments were completed at in-person clinic visits by study trained personnel. Adolescents and caregivers independently completed paper/pencil measures. Adolescent and caregiver heights and weights were measured by certified research staff, using digital scales and stadiometers provided at each care center. Participants were weighed and measured in street clothing without shoes, with weight and height measurements taken in triplicate.
Measures
Revised Peer Experiences Questionnaire
Victimization was assessed using the 18-item victim version of the Revised Peer Experiences Questionnaire (Prinstein et al., 2001), a self-report measure of overt (three items, e.g., “a teen hit, kicked, or pushed me in a mean way”), relational (three items, e.g., “a teen left me out of what they were doing”), and reputational (three items, e.g., “another teen gossiped about me so others would not like me”) victimization. Adolescents rated each item regarding past year frequency of occurrence (1 = never to 5 = a few times a week), with scales computed as the average across items. This measure has acceptable psychometrics (Prinstein et al., 2001; De Los Reyes & Prinstein, 2004) with internal consistencies for the current sample ranging from α = 0.65 to α = 0.84.
Youth Self-Report
Adolescent-reported internalizing and externalizing symptoms in the past 6 months were obtained via two broadband scales of the Youth Self-Report (YSR; Achenbach & Rescorla, 2001). The Social Competence (e.g., participation in organizations and groups, number and contact with friends, and behavior with others) and the Academic Performance scales (mean performance in academic subjects from failing [0] to above average [3]) were also used. The strong psychometric properties of the YSR are well-established (Achenbach & Rescorla, 2001; Song, Singh, & Singer, 1994), and it has been used extensively with youth with chronic medical conditions (Pinquart & Shen, 2011).
Self-Perception Profile for Adolescents
The Self-Perception Profile for Adolescents is 45-item self-report measure assessing adolescent self-perceptions of competence in specific domains as well as a global perception of self-worth (Harter, 2012). Each item is rated from 1 (low perceived competence) to 4 (high perceived competence), with domains scored as the average across items. The global self-worth scale was used (five items), which serves as a general assessment of how happy adolescents are with themselves or their lives. This measure has demonstrated good validity (Harter, 2012), as well as good internal consistency (α = 0.80) for global self-worth for the current sample.
Children’s Social Support Questionnaire
The Children’s Social Support Questionnaire measured adolescent perception of the size and quality of their social support network (Bogat, Chin, Sabbath, & Schwartz, 1985). Adolescents were asked to list people who were part of their “social network” and rate how happy they were with each relationship (1 = very unhappy to 5 = very happy). Network size was obtained by summing all individuals listed, and the average of their happiness rating across all individuals was computed. If no individuals were listed, a “0” was entered for happiness with social support. This measure has acceptable psychometrics (Bogat et al., 1985).
Other Measures
Caregivers completed a demographic questionnaire to assess caregiver gender, age, level of education, and family composition. Adolescents were asked about current school enrollment. Mean height and weight were used to calculate BMI (kg/m2).
Analyses
Missing data ranged from 0.5% to 2.7% for all variables and were handled via maximum likelihood estimation in Mplus (Version 7.3). The nesting of participants within the five data collection sites was controlled in hypothesized analyses via specialized variable and analysis commands in Mplus to avoid possible Type-1 errors. Preliminary analyses using two-tailed independent t tests or Chi-square tests for demographic factors and BMI as well as analyses of covariance (ANCOVA) for variables of interest compared groups (WLS vs. NSComps). Demographic variables for which significant differences were found were controlled in group comparison analyses. To test proposed models of mediation, separate path analyses were completed with the significance of each indirect effect (i.e., the effect of victimization [overt, relational, or reputational] on adjustment [internalizing, externalizing, social competence, or academic performance] through global self-worth) evaluated using the “Indirect” command in Mplus with bootstrapped confidence intervals (CI). Bootstrapping with 5,000 resamples was used to create CI, as this strategy provides a nonparametric approach that can be effectively used with small samples. Tests of whether these individual models of mediation were moderated (i.e., moderated mediation) by social support (i.e., adolescent perception of happiness with social support) were also completed in Mplus using path analysis and “Model Constraint” commands as suggested in the Mplus user’s guide (Muthen & Muthen, 1998,–2012). For each model, CI for the conditional indirect effects (i.e., at +1 SD or −1 SD of the moderator) were also generated with a bootstrapping procedure.
Results
Descriptives
Adolescents were primarily female, White, and living in two-caregiver homes (Table I). WLS participants were significantly older and had a higher mean BMI relative to NSComps. No other significant demographic differences were identified. Table II presents descriptive information for all variables of interest for the total sample and by group. The means for relational and reputational victimization were similar to those found for a sample of high school students, although slightly lower for overt victimization (De Los Reyes & Prinstein, 2004). Of those participants who had not yet graduated high school, the majority attended school with their peers (i.e., not home schooled/early leaving), with mean social competence T scores indicating good adjustment. A number of significant group (WLS vs. NSComp) differences were identified using ANCOVA after controlling for adolescent age and BMI. NSComps reported greater experiences of relational victimization and lower academic performance relative to the WLS group. Groups were similar for measures of global self-worth and social support. Finally, although not included in Table II, group differences have been reported previously for internalizing symptoms and externalizing symptoms, which are dependent variables in the current study’s analyses. Specifically, NSComps had significantly higher levels of self-reported internalizing symptoms and externalizing symptoms on the YSR (see Rofey et al., 2015).
Demographic Characteristics of WLS Adolescents and NSComp Adolescents and their Families
| Demographics . | Total (N = 222) . | WLS (n = 139) . | NSComp (n = 83) . | pa . |
|---|---|---|---|---|
| Mean ± SD% . | Mean ± SD% . | Mean ± SD% . | ||
| Adolescent | ||||
| BMI | 49.77 ± 7.89 | 51.52 ± 8.32 | 46.85 ± 6.12 | <.001 |
| Age | 16.59 ± 1.44 | 16.86 ± 1.39 | 16.11 ± 1.40 | <.001 |
| % Female | 80.6% | 79.9% | 81.9% | .71 |
| % Whiteb | 61.7% | 66.2% | 54.2% | .08 |
| Caregiverc | ||||
| BMI | 38.05 ± 9.63 | 37.84 ± 9.35 | 38.35 ± 10.08 | .71 |
| Age | 44.27 ± 7.50 | 44.47 ± 6.41 | 43.93 ± 9.05 | .63 |
| % Female | 93.6% | 93.4% | 94.0% | .86 |
| Education | .18 | |||
| % ≤ High School Graduation | 42.5% | 39.0% | 48.2% | |
| % 1+ years after secondary | 57.5% | 61.0% | 51.8% | |
| Family | ||||
| % Single caregiver home | 33.3% | 31.6% | 36.1% | .49 |
| Demographics . | Total (N = 222) . | WLS (n = 139) . | NSComp (n = 83) . | pa . |
|---|---|---|---|---|
| Mean ± SD% . | Mean ± SD% . | Mean ± SD% . | ||
| Adolescent | ||||
| BMI | 49.77 ± 7.89 | 51.52 ± 8.32 | 46.85 ± 6.12 | <.001 |
| Age | 16.59 ± 1.44 | 16.86 ± 1.39 | 16.11 ± 1.40 | <.001 |
| % Female | 80.6% | 79.9% | 81.9% | .71 |
| % Whiteb | 61.7% | 66.2% | 54.2% | .08 |
| Caregiverc | ||||
| BMI | 38.05 ± 9.63 | 37.84 ± 9.35 | 38.35 ± 10.08 | .71 |
| Age | 44.27 ± 7.50 | 44.47 ± 6.41 | 43.93 ± 9.05 | .63 |
| % Female | 93.6% | 93.4% | 94.0% | .86 |
| Education | .18 | |||
| % ≤ High School Graduation | 42.5% | 39.0% | 48.2% | |
| % 1+ years after secondary | 57.5% | 61.0% | 51.8% | |
| Family | ||||
| % Single caregiver home | 33.3% | 31.6% | 36.1% | .49 |
Note: BMI = Body mass index; NSComp = nonsurgical comparison; WLS = weight loss surgery.
p-values are based on two-tailed independent t tests when examining mean values and on Chi-square tests when examining percentages.
The remaining self-identified as Black (26.1%), more than one race (5.4%), or Hispanic (6.8%).
Demographic information was available for 136 WLS caregivers, with the exception of caregiver BMI, which was available for 123 caregivers. Demographic information was available for all 83 comparison caregivers.
Demographic Characteristics of WLS Adolescents and NSComp Adolescents and their Families
| Demographics . | Total (N = 222) . | WLS (n = 139) . | NSComp (n = 83) . | pa . |
|---|---|---|---|---|
| Mean ± SD% . | Mean ± SD% . | Mean ± SD% . | ||
| Adolescent | ||||
| BMI | 49.77 ± 7.89 | 51.52 ± 8.32 | 46.85 ± 6.12 | <.001 |
| Age | 16.59 ± 1.44 | 16.86 ± 1.39 | 16.11 ± 1.40 | <.001 |
| % Female | 80.6% | 79.9% | 81.9% | .71 |
| % Whiteb | 61.7% | 66.2% | 54.2% | .08 |
| Caregiverc | ||||
| BMI | 38.05 ± 9.63 | 37.84 ± 9.35 | 38.35 ± 10.08 | .71 |
| Age | 44.27 ± 7.50 | 44.47 ± 6.41 | 43.93 ± 9.05 | .63 |
| % Female | 93.6% | 93.4% | 94.0% | .86 |
| Education | .18 | |||
| % ≤ High School Graduation | 42.5% | 39.0% | 48.2% | |
| % 1+ years after secondary | 57.5% | 61.0% | 51.8% | |
| Family | ||||
| % Single caregiver home | 33.3% | 31.6% | 36.1% | .49 |
| Demographics . | Total (N = 222) . | WLS (n = 139) . | NSComp (n = 83) . | pa . |
|---|---|---|---|---|
| Mean ± SD% . | Mean ± SD% . | Mean ± SD% . | ||
| Adolescent | ||||
| BMI | 49.77 ± 7.89 | 51.52 ± 8.32 | 46.85 ± 6.12 | <.001 |
| Age | 16.59 ± 1.44 | 16.86 ± 1.39 | 16.11 ± 1.40 | <.001 |
| % Female | 80.6% | 79.9% | 81.9% | .71 |
| % Whiteb | 61.7% | 66.2% | 54.2% | .08 |
| Caregiverc | ||||
| BMI | 38.05 ± 9.63 | 37.84 ± 9.35 | 38.35 ± 10.08 | .71 |
| Age | 44.27 ± 7.50 | 44.47 ± 6.41 | 43.93 ± 9.05 | .63 |
| % Female | 93.6% | 93.4% | 94.0% | .86 |
| Education | .18 | |||
| % ≤ High School Graduation | 42.5% | 39.0% | 48.2% | |
| % 1+ years after secondary | 57.5% | 61.0% | 51.8% | |
| Family | ||||
| % Single caregiver home | 33.3% | 31.6% | 36.1% | .49 |
Note: BMI = Body mass index; NSComp = nonsurgical comparison; WLS = weight loss surgery.
p-values are based on two-tailed independent t tests when examining mean values and on Chi-square tests when examining percentages.
The remaining self-identified as Black (26.1%), more than one race (5.4%), or Hispanic (6.8%).
Demographic information was available for 136 WLS caregivers, with the exception of caregiver BMI, which was available for 123 caregivers. Demographic information was available for all 83 comparison caregivers.
Mean Levels of Adolescent Victimization, Level of Social Disengagement and Competence, Academic Performance, Self-Perceptions and Social Support for WLS Adolescents and NSComp Adolescents
| Adolescent Self Report . | Total . | WLS (n = 137–139) . | NSComp (n = 82–83) . | pa . | Cohen’s db . | Range of scores Total N . |
|---|---|---|---|---|---|---|
| Mean ± SD n (%) . | Mean ± SD n (%) . | Mean ± SD n (%) . | . | . | . | |
| General victimization (RPEQ) | ||||||
| Overt victimization | 1.19 ± 0.39 | 1.15 ± 0.35 | 1.25 ± 0.44 | .45 | 0.26 | 1–3, N = 221 |
| Relational victimization | 1.97 ± 0.90 | 1.87 ± 0.85 | 2.13 ± 0.95 | .03 | 0.29 | 1–5, N = 222 |
| Reputational victimization | 1.72 ± 0.89 | 1.62 ± 0.83 | 1.90 ± 0.98 | .17 | 0.32 | 1–5, N = 221 |
| Social competence/academic | ||||||
| % Home schooled/not in schoolc | 23 (10.8%) | 15 (11.5%) | 8 (9.8%) | .98 | 0.99 | |
| % In school with peers | 190 (89.2%) | 116 (88.5%) | 74 (90.2%) | |||
| Social competence (YSR)d | 45.56 ± 10.63 | 45.96 ± 10.59 | 44.88 ± 10.73 | .08 | 0.10 | 22–65, N = 218 |
| Academic performance (YSR)d | 2.20 ± 0.54 | 2.25 ± 0.52 | 2.13 ± 0.56 | .01 | 0.21 | 0.50–3.00, N = 205 |
| Self-Perceptions (SPPA) | ||||||
| Global Self-Worth | 2.76 ± 0.72 | 2.84 ± 0.70 | 2.64 ± 0.75 | .48 | 0.28 | 1–4, N = 220 |
| Social Support (CSSQ) | ||||||
| Total Network Size | 8.05 ± 4.04 | 8.33 ± 3.98 | 7.58 ± 4.11 | .08 | 0.19 | 0–17, N = 222 |
| Total Happiness | 4.25 ± 0.86 | 4.33 ± 0.87 | 4.14 ± 0.84 | .18 | 0.22 | 0–5, N = 222 |
| Adolescent Self Report . | Total . | WLS (n = 137–139) . | NSComp (n = 82–83) . | pa . | Cohen’s db . | Range of scores Total N . |
|---|---|---|---|---|---|---|
| Mean ± SD n (%) . | Mean ± SD n (%) . | Mean ± SD n (%) . | . | . | . | |
| General victimization (RPEQ) | ||||||
| Overt victimization | 1.19 ± 0.39 | 1.15 ± 0.35 | 1.25 ± 0.44 | .45 | 0.26 | 1–3, N = 221 |
| Relational victimization | 1.97 ± 0.90 | 1.87 ± 0.85 | 2.13 ± 0.95 | .03 | 0.29 | 1–5, N = 222 |
| Reputational victimization | 1.72 ± 0.89 | 1.62 ± 0.83 | 1.90 ± 0.98 | .17 | 0.32 | 1–5, N = 221 |
| Social competence/academic | ||||||
| % Home schooled/not in schoolc | 23 (10.8%) | 15 (11.5%) | 8 (9.8%) | .98 | 0.99 | |
| % In school with peers | 190 (89.2%) | 116 (88.5%) | 74 (90.2%) | |||
| Social competence (YSR)d | 45.56 ± 10.63 | 45.96 ± 10.59 | 44.88 ± 10.73 | .08 | 0.10 | 22–65, N = 218 |
| Academic performance (YSR)d | 2.20 ± 0.54 | 2.25 ± 0.52 | 2.13 ± 0.56 | .01 | 0.21 | 0.50–3.00, N = 205 |
| Self-Perceptions (SPPA) | ||||||
| Global Self-Worth | 2.76 ± 0.72 | 2.84 ± 0.70 | 2.64 ± 0.75 | .48 | 0.28 | 1–4, N = 220 |
| Social Support (CSSQ) | ||||||
| Total Network Size | 8.05 ± 4.04 | 8.33 ± 3.98 | 7.58 ± 4.11 | .08 | 0.19 | 0–17, N = 222 |
| Total Happiness | 4.25 ± 0.86 | 4.33 ± 0.87 | 4.14 ± 0.84 | .18 | 0.22 | 0–5, N = 222 |
Note: CSSQ = Child Social Support Questionnaire; NSComp = nonsurgical comparison; RPEQ = Revised Peer Experiences Scale; SPPA = Self-Perception Profile for Adolescents; WLS = weight loss surgery; YSR = Youth Self Report.
For mean levels, p-values were based on analyses of covariance. For prevalence estimates, p-values were based on logistic regressions. Adolescent age and BMI were used as covariates in both sets of analyses.
Effect sizes are reported as Cohen’s d, and are defined at small = 0.20, medium = 0.50, and large = 0.80.
For the analyses comparing those participants home schooled/not in regular school versus those in school, participants who graduated high school (7 WLS, 1 NSComp) were excluded. One WLS participant was missing data for this question. The effect size for this variable is given as an odds ratio.
For the YSR, means and SDs are provided as T scores for Social Competence in the table to aid in interpretation, but all analyses were completed using raw scores. T scores are not computed for academic performance. For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11), leaving 205 of 211.
Mean Levels of Adolescent Victimization, Level of Social Disengagement and Competence, Academic Performance, Self-Perceptions and Social Support for WLS Adolescents and NSComp Adolescents
| Adolescent Self Report . | Total . | WLS (n = 137–139) . | NSComp (n = 82–83) . | pa . | Cohen’s db . | Range of scores Total N . |
|---|---|---|---|---|---|---|
| Mean ± SD n (%) . | Mean ± SD n (%) . | Mean ± SD n (%) . | . | . | . | |
| General victimization (RPEQ) | ||||||
| Overt victimization | 1.19 ± 0.39 | 1.15 ± 0.35 | 1.25 ± 0.44 | .45 | 0.26 | 1–3, N = 221 |
| Relational victimization | 1.97 ± 0.90 | 1.87 ± 0.85 | 2.13 ± 0.95 | .03 | 0.29 | 1–5, N = 222 |
| Reputational victimization | 1.72 ± 0.89 | 1.62 ± 0.83 | 1.90 ± 0.98 | .17 | 0.32 | 1–5, N = 221 |
| Social competence/academic | ||||||
| % Home schooled/not in schoolc | 23 (10.8%) | 15 (11.5%) | 8 (9.8%) | .98 | 0.99 | |
| % In school with peers | 190 (89.2%) | 116 (88.5%) | 74 (90.2%) | |||
| Social competence (YSR)d | 45.56 ± 10.63 | 45.96 ± 10.59 | 44.88 ± 10.73 | .08 | 0.10 | 22–65, N = 218 |
| Academic performance (YSR)d | 2.20 ± 0.54 | 2.25 ± 0.52 | 2.13 ± 0.56 | .01 | 0.21 | 0.50–3.00, N = 205 |
| Self-Perceptions (SPPA) | ||||||
| Global Self-Worth | 2.76 ± 0.72 | 2.84 ± 0.70 | 2.64 ± 0.75 | .48 | 0.28 | 1–4, N = 220 |
| Social Support (CSSQ) | ||||||
| Total Network Size | 8.05 ± 4.04 | 8.33 ± 3.98 | 7.58 ± 4.11 | .08 | 0.19 | 0–17, N = 222 |
| Total Happiness | 4.25 ± 0.86 | 4.33 ± 0.87 | 4.14 ± 0.84 | .18 | 0.22 | 0–5, N = 222 |
| Adolescent Self Report . | Total . | WLS (n = 137–139) . | NSComp (n = 82–83) . | pa . | Cohen’s db . | Range of scores Total N . |
|---|---|---|---|---|---|---|
| Mean ± SD n (%) . | Mean ± SD n (%) . | Mean ± SD n (%) . | . | . | . | |
| General victimization (RPEQ) | ||||||
| Overt victimization | 1.19 ± 0.39 | 1.15 ± 0.35 | 1.25 ± 0.44 | .45 | 0.26 | 1–3, N = 221 |
| Relational victimization | 1.97 ± 0.90 | 1.87 ± 0.85 | 2.13 ± 0.95 | .03 | 0.29 | 1–5, N = 222 |
| Reputational victimization | 1.72 ± 0.89 | 1.62 ± 0.83 | 1.90 ± 0.98 | .17 | 0.32 | 1–5, N = 221 |
| Social competence/academic | ||||||
| % Home schooled/not in schoolc | 23 (10.8%) | 15 (11.5%) | 8 (9.8%) | .98 | 0.99 | |
| % In school with peers | 190 (89.2%) | 116 (88.5%) | 74 (90.2%) | |||
| Social competence (YSR)d | 45.56 ± 10.63 | 45.96 ± 10.59 | 44.88 ± 10.73 | .08 | 0.10 | 22–65, N = 218 |
| Academic performance (YSR)d | 2.20 ± 0.54 | 2.25 ± 0.52 | 2.13 ± 0.56 | .01 | 0.21 | 0.50–3.00, N = 205 |
| Self-Perceptions (SPPA) | ||||||
| Global Self-Worth | 2.76 ± 0.72 | 2.84 ± 0.70 | 2.64 ± 0.75 | .48 | 0.28 | 1–4, N = 220 |
| Social Support (CSSQ) | ||||||
| Total Network Size | 8.05 ± 4.04 | 8.33 ± 3.98 | 7.58 ± 4.11 | .08 | 0.19 | 0–17, N = 222 |
| Total Happiness | 4.25 ± 0.86 | 4.33 ± 0.87 | 4.14 ± 0.84 | .18 | 0.22 | 0–5, N = 222 |
Note: CSSQ = Child Social Support Questionnaire; NSComp = nonsurgical comparison; RPEQ = Revised Peer Experiences Scale; SPPA = Self-Perception Profile for Adolescents; WLS = weight loss surgery; YSR = Youth Self Report.
For mean levels, p-values were based on analyses of covariance. For prevalence estimates, p-values were based on logistic regressions. Adolescent age and BMI were used as covariates in both sets of analyses.
Effect sizes are reported as Cohen’s d, and are defined at small = 0.20, medium = 0.50, and large = 0.80.
For the analyses comparing those participants home schooled/not in regular school versus those in school, participants who graduated high school (7 WLS, 1 NSComp) were excluded. One WLS participant was missing data for this question. The effect size for this variable is given as an odds ratio.
For the YSR, means and SDs are provided as T scores for Social Competence in the table to aid in interpretation, but all analyses were completed using raw scores. T scores are not computed for academic performance. For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11), leaving 205 of 211.
Intercorrelations of Victimization With Adjustment and Social Support
Using Pearson correlations (Table III), associations were in the expected directions with greater victimization correlated with greater internalizing symptoms and externalizing symptoms as well as lower global self-worth. Few significant associations were identified with measures of social competence, academic performance, or social support.
Intercorrelations of Measures of Victimization With Adolescent Adjustment, Self-Perceptions and Social Support for Severely Obese Adolescents (N = 218–221)
| Adolescent Self Report . | Overt victimization . | Relational victimization . | Reputational victimization . |
|---|---|---|---|
| Psychopathology (YSR) | |||
| Internalizing symptoms | .19* | .32** | .34** |
| Externalizing symptoms | .13 | .22* | .31** |
| Social/academic competencea | |||
| Social competence (YSR) | −.03 | −.07 | −.13 |
| Academic performance (YSR) | −.05 | .04 | −.01 |
| Home schooled/not in regular school | .19** | −.07 | −.06 |
| Self-perceptions (SPPA) | |||
| Global self-worth | −.26* | −.30** | −.33** |
| Social support (CSSQ) | |||
| Network size | .06 | −.004 | −.01 |
| Happiness | −.04 | −.13 | −.21 |
| Adolescent Self Report . | Overt victimization . | Relational victimization . | Reputational victimization . |
|---|---|---|---|
| Psychopathology (YSR) | |||
| Internalizing symptoms | .19* | .32** | .34** |
| Externalizing symptoms | .13 | .22* | .31** |
| Social/academic competencea | |||
| Social competence (YSR) | −.03 | −.07 | −.13 |
| Academic performance (YSR) | −.05 | .04 | −.01 |
| Home schooled/not in regular school | .19** | −.07 | −.06 |
| Self-perceptions (SPPA) | |||
| Global self-worth | −.26* | −.30** | −.33** |
| Social support (CSSQ) | |||
| Network size | .06 | −.004 | −.01 |
| Happiness | −.04 | −.13 | −.21 |
Note: CSSQ = Children’s Social Support Questionnaire; SPPA = Self-Perception Profile for Adolescents; YSR = Youth Self Report. To control for Type I error, the significance level was set at p < .01. p < .01; **p < .001.
Sample size for social competence was from n = 218. For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11), leaving a sample size of n = 205.
Intercorrelations of Measures of Victimization With Adolescent Adjustment, Self-Perceptions and Social Support for Severely Obese Adolescents (N = 218–221)
| Adolescent Self Report . | Overt victimization . | Relational victimization . | Reputational victimization . |
|---|---|---|---|
| Psychopathology (YSR) | |||
| Internalizing symptoms | .19* | .32** | .34** |
| Externalizing symptoms | .13 | .22* | .31** |
| Social/academic competencea | |||
| Social competence (YSR) | −.03 | −.07 | −.13 |
| Academic performance (YSR) | −.05 | .04 | −.01 |
| Home schooled/not in regular school | .19** | −.07 | −.06 |
| Self-perceptions (SPPA) | |||
| Global self-worth | −.26* | −.30** | −.33** |
| Social support (CSSQ) | |||
| Network size | .06 | −.004 | −.01 |
| Happiness | −.04 | −.13 | −.21 |
| Adolescent Self Report . | Overt victimization . | Relational victimization . | Reputational victimization . |
|---|---|---|---|
| Psychopathology (YSR) | |||
| Internalizing symptoms | .19* | .32** | .34** |
| Externalizing symptoms | .13 | .22* | .31** |
| Social/academic competencea | |||
| Social competence (YSR) | −.03 | −.07 | −.13 |
| Academic performance (YSR) | −.05 | .04 | −.01 |
| Home schooled/not in regular school | .19** | −.07 | −.06 |
| Self-perceptions (SPPA) | |||
| Global self-worth | −.26* | −.30** | −.33** |
| Social support (CSSQ) | |||
| Network size | .06 | −.004 | −.01 |
| Happiness | −.04 | −.13 | −.21 |
Note: CSSQ = Children’s Social Support Questionnaire; SPPA = Self-Perception Profile for Adolescents; YSR = Youth Self Report. To control for Type I error, the significance level was set at p < .01. p < .01; **p < .001.
Sample size for social competence was from n = 218. For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11), leaving a sample size of n = 205.
Models of Mediation
Separate models of mediation tested whether the indirect effects of victimization (i.e., either overt, relational, or reputational) on various measures of self-reported adjustment (internalizing symptoms, externalizing symptoms, social competence, or academic performance) through global self-worth were significant (Figure 1). Given significant group (WLS vs. NSComp) differences noted above, group was controlled for in all models. Standardized beta estimates for pathways “a,” “b,” and “c” for these individual models as shown in Figure 1, as well as unstandardized beta estimates of all indirect effects with 95% CIs, are presented in Table IV.
Mediation Analyses Testing the Indirect Effects of Victimization Type (i.e., Overt, Relational, or Reputational) on Adjustment (i.e., Internalizing Symptoms, Externalizing Symptoms, Social Competence, or Academic Performance) Through Global Self-Worth for 222 Adolescents With Severe Obesity
| Mediational models . | Standardized B . | Indirect effecta . | R2 . | ||
|---|---|---|---|---|---|
| A . | b . | c . | (95% CI) . | . | |
| 1. Overt/internalizing | −.27*** | −.50*** | .05 | 3.09 (1.65 – 4.92) | 0.27 |
| 2. Relational/internalizing | −.30*** | −.45*** | .17 | 1.36 (0.95 – 1.79) | 0.30 |
| 3. Reputational/internalizing | −.33*** | −.45*** | .18** | 1.48 (1.02 – 2.39) | 0.30 |
| 4. Overt/externalizing | −.27** | −.18** | .06 | 0.87 (0.35 – 1.96) | 0.09 |
| 5. Relational/externalizing | −.30*** | −.14** | .15 | 0.32 (0.13 – 0.50) | 0.11 |
| 6. Reputational/externalizing | −.33*** | −.11* | .24* | 0.28 (−0.06 – 0.85) | 0.14 |
| 7. Overt/social competence | −.26** | .33*** | .06 | −0.59 (−1.21 – −0.26) | 0.11 |
| 8. Relational/social competence | −.30*** | .33*** | .03 | −0.30 (−0.41 – −0.22) | 0.11 |
| 9. Reputational/social competence | −.33*** | .31*** | −.03 | −0.30 (−0.56 – −0.22) | 0.11 |
| 10. Overt/academicb | −.27** | .19 | .01 | −0.07 (−0.18 – −0.01) | 0.04 |
| 11. Relational/academicb | −.30*** | .21** | .12 | −0.04 (−0.06 – −0.003) | 0.05 |
| 12. Reputational/Academicb | −.34*** | .20 | .05 | −0.04 (−0.09 – 0.00) | 0.04 |
| Mediational models . | Standardized B . | Indirect effecta . | R2 . | ||
|---|---|---|---|---|---|
| A . | b . | c . | (95% CI) . | . | |
| 1. Overt/internalizing | −.27*** | −.50*** | .05 | 3.09 (1.65 – 4.92) | 0.27 |
| 2. Relational/internalizing | −.30*** | −.45*** | .17 | 1.36 (0.95 – 1.79) | 0.30 |
| 3. Reputational/internalizing | −.33*** | −.45*** | .18** | 1.48 (1.02 – 2.39) | 0.30 |
| 4. Overt/externalizing | −.27** | −.18** | .06 | 0.87 (0.35 – 1.96) | 0.09 |
| 5. Relational/externalizing | −.30*** | −.14** | .15 | 0.32 (0.13 – 0.50) | 0.11 |
| 6. Reputational/externalizing | −.33*** | −.11* | .24* | 0.28 (−0.06 – 0.85) | 0.14 |
| 7. Overt/social competence | −.26** | .33*** | .06 | −0.59 (−1.21 – −0.26) | 0.11 |
| 8. Relational/social competence | −.30*** | .33*** | .03 | −0.30 (−0.41 – −0.22) | 0.11 |
| 9. Reputational/social competence | −.33*** | .31*** | −.03 | −0.30 (−0.56 – −0.22) | 0.11 |
| 10. Overt/academicb | −.27** | .19 | .01 | −0.07 (−0.18 – −0.01) | 0.04 |
| 11. Relational/academicb | −.30*** | .21** | .12 | −0.04 (−0.06 – −0.003) | 0.05 |
| 12. Reputational/Academicb | −.34*** | .20 | .05 | −0.04 (−0.09 – 0.00) | 0.04 |
Note: Pathways: a = (victimization type → global self-worth); Pathway b = (global self-worth → measure of adjustment, with victimization type in the model), and Pathway c = (victimization type → measure of adjustment with global self-worth in the model). Group status (Weight Loss Surgery and Nonsurgical Comparisons) was controlled for in all models.
p < .05;
p < .01;
p < .001.
Unstandardized beta estimates with 95% confidence intervals are provided for all indirect effects.
For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11).
Mediation Analyses Testing the Indirect Effects of Victimization Type (i.e., Overt, Relational, or Reputational) on Adjustment (i.e., Internalizing Symptoms, Externalizing Symptoms, Social Competence, or Academic Performance) Through Global Self-Worth for 222 Adolescents With Severe Obesity
| Mediational models . | Standardized B . | Indirect effecta . | R2 . | ||
|---|---|---|---|---|---|
| A . | b . | c . | (95% CI) . | . | |
| 1. Overt/internalizing | −.27*** | −.50*** | .05 | 3.09 (1.65 – 4.92) | 0.27 |
| 2. Relational/internalizing | −.30*** | −.45*** | .17 | 1.36 (0.95 – 1.79) | 0.30 |
| 3. Reputational/internalizing | −.33*** | −.45*** | .18** | 1.48 (1.02 – 2.39) | 0.30 |
| 4. Overt/externalizing | −.27** | −.18** | .06 | 0.87 (0.35 – 1.96) | 0.09 |
| 5. Relational/externalizing | −.30*** | −.14** | .15 | 0.32 (0.13 – 0.50) | 0.11 |
| 6. Reputational/externalizing | −.33*** | −.11* | .24* | 0.28 (−0.06 – 0.85) | 0.14 |
| 7. Overt/social competence | −.26** | .33*** | .06 | −0.59 (−1.21 – −0.26) | 0.11 |
| 8. Relational/social competence | −.30*** | .33*** | .03 | −0.30 (−0.41 – −0.22) | 0.11 |
| 9. Reputational/social competence | −.33*** | .31*** | −.03 | −0.30 (−0.56 – −0.22) | 0.11 |
| 10. Overt/academicb | −.27** | .19 | .01 | −0.07 (−0.18 – −0.01) | 0.04 |
| 11. Relational/academicb | −.30*** | .21** | .12 | −0.04 (−0.06 – −0.003) | 0.05 |
| 12. Reputational/Academicb | −.34*** | .20 | .05 | −0.04 (−0.09 – 0.00) | 0.04 |
| Mediational models . | Standardized B . | Indirect effecta . | R2 . | ||
|---|---|---|---|---|---|
| A . | b . | c . | (95% CI) . | . | |
| 1. Overt/internalizing | −.27*** | −.50*** | .05 | 3.09 (1.65 – 4.92) | 0.27 |
| 2. Relational/internalizing | −.30*** | −.45*** | .17 | 1.36 (0.95 – 1.79) | 0.30 |
| 3. Reputational/internalizing | −.33*** | −.45*** | .18** | 1.48 (1.02 – 2.39) | 0.30 |
| 4. Overt/externalizing | −.27** | −.18** | .06 | 0.87 (0.35 – 1.96) | 0.09 |
| 5. Relational/externalizing | −.30*** | −.14** | .15 | 0.32 (0.13 – 0.50) | 0.11 |
| 6. Reputational/externalizing | −.33*** | −.11* | .24* | 0.28 (−0.06 – 0.85) | 0.14 |
| 7. Overt/social competence | −.26** | .33*** | .06 | −0.59 (−1.21 – −0.26) | 0.11 |
| 8. Relational/social competence | −.30*** | .33*** | .03 | −0.30 (−0.41 – −0.22) | 0.11 |
| 9. Reputational/social competence | −.33*** | .31*** | −.03 | −0.30 (−0.56 – −0.22) | 0.11 |
| 10. Overt/academicb | −.27** | .19 | .01 | −0.07 (−0.18 – −0.01) | 0.04 |
| 11. Relational/academicb | −.30*** | .21** | .12 | −0.04 (−0.06 – −0.003) | 0.05 |
| 12. Reputational/Academicb | −.34*** | .20 | .05 | −0.04 (−0.09 – 0.00) | 0.04 |
Note: Pathways: a = (victimization type → global self-worth); Pathway b = (global self-worth → measure of adjustment, with victimization type in the model), and Pathway c = (victimization type → measure of adjustment with global self-worth in the model). Group status (Weight Loss Surgery and Nonsurgical Comparisons) was controlled for in all models.
p < .05;
p < .01;
p < .001.
Unstandardized beta estimates with 95% confidence intervals are provided for all indirect effects.
For academic performance, those participants who were not attending any school/educational training were excluded from analyses (n = 11).
For all models involving internalizing symptoms, indirect effects were significant, suggesting that greater victimization, regardless of type, was associated with lower global self-worth, which in turn was associated with greater internalizing symptoms. As indicated by the standardized betas for path c, the association for reputational victimization remained significant even with global self-worth in the model. In addition, R2 values suggest that these models explain a substantial amount of variance. For externalizing symptoms, indirect effects for models involving overt victimization or relational victimization were significant. The indirect effect for reputational victimization was nonsignificant, although its association with externalizing symptoms (pathway c) remained significant even with global self-worth in the model. Finally, although zero-order correlations indicated few significant associations between types of victimization with social competence and academic performance (Table III), tests of mediation indicated that the majority of indirect effects through global self-worth were significant, with the only exception involving reputational mediation with academic performance. Little variance was explained by these models, particularly for academic performance.
Moderation by Social Support
For mediational models with significant indirect effects, moderation by adolescent perception of social support network happiness was tested. Moderation was tested for both direct effects (pathway “c” in Figure 1: interaction of social support and victimization type → adjustment) and indirect effects (pathway “a”: effect of social support and victimization type through global self-worth) at low (−1 SD) and high (+1 SD) values of the moderator.
Results suggested that several mediational models were significantly moderated by social support. In these cases, the independent variable was relational victimization, with no significant moderation for models including overt or reputational victimization. In addition, significant moderation occurred only for the indirect paths but not for the direct paths. For relational victimization → global self-worth → internalizing, the indirect effect was nonsignificant at high levels of social support (β = 0.63; 95% CI = −0.30 to 0.99) but remained significant at low levels (β = 1.12; 95% CI = 0.56 to 1.81). For relational victimization → global self-worth → social competence, the indirect effect remained significant at low levels of social support (β = −0.21; 95% CI = −0.38 to −0.07), but at high levels, was nonsignificant (β = −0.12; 95% CI = −0.20 to 0.04). For all other mediation models tested for potential moderation, indirect effects through global self-worth remained significant regardless of the level of social support. These results suggest that an adolescent’s happiness with social support may be protective against the effects relational victimization operating through global self-worth, but that social support did not have an impact for other types of victimization.
Discussion
The present study extends the literature by providing a comprehensive assessment of overt, relational, and reputational peer victimization and their associations with a diverse set of clinically important outcomes for a sample of treatment-seeking adolescents with severe obesity at known risk. Consistent with the literature (Copeland et al., 2013; Hawker & Boulton, 2000), adolescent perception of greater victimization was associated with greater levels of adolescent internalizing symptoms and externalizing symptoms as well as lower global self-worth, although there were few significant associations with social competence or academic performance.
When testing mediational models, indirect effects involving overt victimization and relational victimization through global self-worth on each dependent variable (e.g., internalizing, externalizing, social competence, and academic performance) were significant, whereas the pathways from victimization to the dependent variables were nonsignificant when global self-worth was also in the model. These results are consistent with social information processing theory (Crick & Dodge, 1994), which would suggest that negative peer interactions such as experiences of victimization would lead some youth to develop negative self-perceptions, which in turn could result in difficulties. In contrast, mediational results for reputational victimization were more complex. For the model involving externalizing symptoms, there was no significant indirect effect of reputational victimization through global self-worth, but instead, a significant direct effect after controlling for self-worth. Thus, adolescents who perceive this type of victimization, which involves others spreading rumors and gossip about them, also endorse greater externalizing symptoms regardless of their level of global self-worth. Perhaps these adolescents might have a more confrontational style noticeable to others, making them more likely to be gossiped about by a group of individuals. In addition, some aggressive youth have been characterized as “provocative victims” (Garandeau & Cillessen, 2006). These youth are less likely to hold negative self-perceptions but instead respond to negative peer interactions with hostile attribution biases, which results in more externalizing behaviors.
When examining results for academic performance, zero-order correlations indicated no significant associations between victimization and academic performance in contrast to the general developmental literature (Nakamoto & Schwartz, 2010). Moreover, the indirect effect of reputational victimization on academic performance through self-worth was not significant, which is inconsistent with a recent study, in which Jenkins and Demaray (2015) found significant mediation of victimization on academic performance through academic self-concept for a sample of middle school girls, but not boys. Although significant indirect effects were found for models involving overt and reputational victimization, the amount of variance explained by these models was small. Given the multidimensional structure of self-concept and consistent with findings by Jenkins and Demaray (2015), it may be that the indirect paths from victimization to academic performance are not through global self-worth but through self-perceptions in specific domains (i.e., self-perception of scholastic competence). Alternatively, the physical limitations of adolescents with severe obesity might prevent them from being fully engaged with their peers, including attending school. Approximately 11% of youth in the current sample who had not yet graduated high school were homeschooled/not in regular school, and as such, victimization might have less of an effect on their grades. Future research will need to address these issues. Taken together, these data suggest that the associations of peer victimization on adjustment are complex, and further, seem to indicate self-worth as an important target for prevention and intervention for some types of victimization as well as for poor adjustment in adolescent severe obesity.
Analyses provided some evidence of the buffering effect of social support on some indirect pathways, consistent with literature regarding the benefits of social support (Lim et al., 2011; Moos, 2002). Higher levels of happiness with social support may be protective against negative outcomes such as greater internalizing symptoms and lower social competence from victimization that is relational in nature. However, social support did not appear to have an impact on the effects of overt or reputational victimization. Perhaps for this sample of severely obese adolescents, social support is a more effective buffer against less confrontational styles of victimization such as relational victimization (e.g., social exclusion) as compared with styles of victimization characterized as more confrontational (e.g., overt) or group-based (e.g., reputational), requiring the cooperation of a group of others to spread rumors or gossip. Still, it is encouraging that among youth with severe obesity, often characterized as socially isolated, there is a subsample with social resources available to protect them from some adverse effects.
Unexpectedly, BMI was negatively associated with measures of general victimization. Explaining these associations proves more difficult, as the literature seems to suggest the opposite effect (Puhl et al., 2013). As was stated earlier, it may be that youth at the highest levels of BMI have more physical limitations that keep them from being fully engaged with their peers, and thus, have fewer opportunities to perceive victimization. This could also potentially explain why mean levels of victimization for the current sample appeared similar to levels reported in the literature for the general adolescent population (De Los Reyes & Prinstein, 2004), in contrast to previously reported high rates of victimization in pediatric overweight/obesity.
Strengths of the present study include the multisite and controlled design and a focus on adolescents who have reached severe levels of obesity. We also took a multidimensional approach to understanding victimization and its associations with a diverse set of outcomes using measures with well-established psychometrics. However, this study has several limitations. First, the reliance on self-report of victimization limited potentially important peer insights to understanding victimization. Second, the WLS sample was primarily female and White, limiting our ability to generalize findings to males and other racial/ethnic groups known to be at heightened risk for severe obesity (Kelly et al., 2013) and adolescents in less severe excess weight status ranges or community settings. Further, adolescents who demographically “matched” and participated in the nonoperative comparison group may have been different than those who did not match, or those who initially declined being listed as potential matches on the registry. Third, the cross-sectional nature of the present study limits our ability to draw causal or directional conclusions. Although a temporal ordering of associations was assumed in tests of mediation based on theory, longitudinal studies are needed to test this ordering and to address potential reciprocal effects between victimization and adjustment. Future studies should examine the impact of victimization over time as adolescents enter young adulthood. Finally, although we examined several domains of traditional victimization, future research might address cyberbullying as well, particularly given the implication of the current study’s finding that social support did little to buffer the impact of reputational victimization (i.e., rumors or gossip).
Clinical Implications
Although few group differences were identified, the NSComp group was characterized by poorer functioning when differences were significant. We have documented similar group differences for this cohort in other domains (Rofey et al., 2015; Zeller et al., 2015). While beyond current aims and thus speculative, we argue that unlike adolescents presenting for first-line behavioral weight treatment, adolescents who undergo WLS may be a unique clinical group. Achieving WLS candidacy involves navigating a complex process with multiple levels of decision-makers (i.e., adolescent motivation, supportive caregivers, a referring physician, the clinical team, insurance coverage and approval). It is possible that adolescents with greater psychosocial impairment (i.e., psychopathology, family dysfunction, victimization) or fewer financial resources are less likely to pursue or be referred for surgery. Moreover, adolescents with greater psychosocial impairment who do pursue WLS may drop out of the intensive WLS clinical care pathway during the preoperative phase, or are deferred or denied access to surgery by the clinical team. These are important areas for future research. In addition, youth who do achieve candidacy may benefit from the support and attention from their families and medical team as they prepare for WLS.
Pediatric psychologists or other mental health practitioners involved in pre-WLS evaluations or behavioral weight management programs may want to assess the adolescent’s self-worth and social support as part of intake, to further inform the treatment of psychosocial difficulties, and should be wary of stereotypes that all youth with obesity have significant social difficulties and impaired self-worth. For patients who already express a strong self-worth and/or social support network, mental health practitioners should support and foster the influences contributing to these strengths, while focusing therapy on other issues of importance to the patient. For adolescents experiencing peer difficulties, cognitive behavioral therapies may be useful to deal with victimization proactively, improve self-esteem, and educate the adolescent regarding the value of social support. In particular, adolescents could be encouraged to engage in activities (e.g., volunteering) that provide opportunities for building social support and increasing self-worth not tied to weight management or body esteem. Finally, future work will be necessary to examine group differences in the associations among the variables in this study over time, after one group (WLS) likely experiences significant weight loss while the other group (NSComp) likely maintains or gains weight over time.
Acknowledgments
The authors acknowledge the contributions of additional TeenView Study Group Co-Investigators and staff. Cincinnati Children’s Hospital Medical Center: Faye Doland, BS, Ashley Morgenthal, BS, Taylor Howarth, BS, Shelley Kirk, PhD, Thomas H. Inge, MD, PhD, Michael Helmrath, MD, PhD; Texas Children’s Hospital, Baylor Medical Center: Margaret Callie Lee, MPH, David Allen, BS, Gia Washington, PhD, Carmen Mikhail, PhD, Mary L. Brandt, MD; University of Pittsburgh Medical Center: Ronette Blake, BS, Nermeen El Nokali, PhD, Silva Arslanian, MD, Anita P. Courcoulas, MD, MPH, Children’s Hospital of Alabama University of Alabama: Krishna Desai, MD, Amy Seay, PhD, Beverly Haynes, BSN, Carroll Harmon, MD, PhD; Nationwide Children’s Hospital Medical Center: Melissa Ginn, BS, Amy E. Baughcum, PhD, Marc P. Michalsky, MD; Temple University: David Sarwer, PhD; Teen-LABS Data Coordinating Center: Michelle Starkey Christian, Jennifer Andringa, BS, Carolyn Powers, RD, Rachel Akers, MPH. The authors also acknowledge the significant contributions made by the parent Teen-LABS Consortium (U01DK072493, UM1DK072493l; PI: Inge, MD, PhD), the Teen-LABS Data Coordinating Center (UM1DK095710; PI: Ralph Buncher, ScD), and the NIDDK/Teen-LABS Project Scientist, Mary Horlick, MD.
Methods for this study were first reported in (1) Zeller, M. H., et al. (2015). Child maltreatment and the adolescent patient with severe obesity: Implications for clinical care. Journal of Pediatric Psychology, 40, 640–648 and (2) Rofey, D. L., et al. (2015). A multi-site view of psychosocial risks in patients presenting for bariatric surgery. Obesity, 23, 1218–1225.
Funding
This research was supported by a grant from the National Institutes of Health (R01DK080020, PI: Zeller).
All authors were supported by a grant from the National Institutes of Health (R01DK080020, PI: Zeller), with the exception of Dr Gowey who was funded by a NIH training grant (T32DK062710).
Conflicts of interest: None declared.
References



