-
PDF
- Split View
-
Views
-
Cite
Cite
Kyungmi Yang, Jeong Eun Lee, Won Park, Yong Chan Ahn, Seung Jae Huh, Recent trends in radiotherapy use for major cancers in Korea, Japanese Journal of Clinical Oncology, Volume 53, Issue 12, December 2023, Pages 1177–1182, https://doi.org/10.1093/jjco/hyad106
Close - Share Icon Share
Abstract
Although the trend in radiotherapy in all cancer patients has been studied, changes in radiotherapy modalities for specific cancer types have not been reported. This study aimed to analyze radiotherapy patterns for major cancers in Korea in recent years.
We collected data from claims and reimbursement records of the Health and Insurance Review and Assessment Service from 2017 to 2020, according to initial diagnostic codes. The radiotherapy modalities for major cancers, such as lung, stomach, colorectal, breast and liver cancer, were analyzed. The radiotherapy modalities consisted of two-dimensional radiotherapy, three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, proton radiotherapy and stereotactic body radiotherapy.
Overall, from 2017 to 2020, the use of two-dimensional radiotherapy and three-dimensional conformal radiotherapy decreased, and intensity-modulated radiotherapy increased. In 2017, three-dimensional conformal radiotherapy accounted for approximately half of the radiotherapy in patients for lung and colorectal cancer, which was replaced by intensity-modulated radiotherapy in 2020. In 2020, stereotactic body radiotherapy also accounted for a large proportion of radiotherapy used in liver cancer cases. Intensity-modulated radiotherapy was most used, followed by three-dimensional conformal radiotherapy and two-dimensional radiotherapy for breast cancer in 2020. Among major cancers, radiotherapy utilization for breast cancer is the highest. Compared with other cancers, the number of patients receiving radiotherapy for stomach cancer was low.
The number of patients receiving radiotherapy for major cancers has increased. The use of advanced forms of radiotherapy, such as intensity-modulated radiotherapy, is rapidly increasing for major cancers. The rate of radiotherapy utilization was higher in major cancer patients than in all cancer patients.
Introduction
Cancer is one of the leading causes of death and a significant barrier to increasing life expectancy globally (1). Radiotherapy (RT) is an effective treatment modality used to manage cancer. More than half of cancer patients receive RT in the United States (2). In Korea, the rate of RT utilization in total cancer patients nationwide was 24.5% in 2010, which has consistently increased to 36.1% in 2019 (3). Approximately 20–25% of the patients will be irradiated more than once (4).
Treatments with various RT modalities are becoming more advanced to improve therapeutic effects on tumors and reduce adjacent normal organ side effects. During the last decade, the use of two-dimensional RT (2DRT), three-dimensional conformal RT (3DCRT) and brachytherapy has decreased, whereas that of intensity-modulated RT (IMRT), stereotactic RT (SRT) and proton RT (PRT) has increased (3). There have been reports on the trend of RT in all cancer patients (3,5), but as per our knowledge, changes in RT modalities for specific cancer types have not yet been reported in Korea.
In this study, we analyzed the current trend in RT use for five specific cancers (lung, stomach, colorectum, breast and liver), which are the major cancers included in the national cancer screening program.
Methods
We analyzed the claims and reimbursements records from the Health and Insurance Review and Assessment Service (HIRA) big data based on the National Health Insurance Service (NHIS), which provides pre-processed statistics, including the annual number of patients with a specific type of cancer according to initial diagnostic codes (6) from January 2017 to December 2020. This data includes all cases of RT at initial diagnosis, RT after recurrence, curative RT for oligo-metastatic cancer, and palliative RT for multiple metastatic cancer.
For analyzing five specific cancers, patients who had the specific diagnostic codes, which have been described below, with at least one RT code were selected. The codes of the International Classification of Diseases 10th revision for cancer diagnoses are as follows: C33-C34 for lung cancer, C16 for stomach cancer, C18-C20 for colorectal cancer, C50 for breast cancer and C22 for liver cancer. Moreover, all treatment codes related to RT were sorted, including 2DRT, 3DCRT, IMRT, PRT, stereotactic body RT (SBRT), stereotactic brain RT (brain SRT), brachytherapy, total body irradiation (TBI), total skin electron beam therapy (TSEBT), intraoperative radiotherapy (IORT). NHIS of Korea defines IMRT as a RT based on inverse planning, and forward planning field-in-field techniques are classified as 3DCRT. The number of patients who received brachytherapy or TBI was below 10 for major cancers, and it was possible that these patients had double primary malignancy or secondary malignancy. There were no patients who received TSEBT or IORT for major cancers. Therefore brachytherapy, TBI, TSEBT and IORT were excluded from the analysis. However, the number of patients who received brachytherapy or TBI was below 10 for major cancers, and it was possible that these patients had double primary malignancy or secondary malignancy. There were no patients who received TSEBT or IORT for major cancers. Therefore brachytherapy, TBI, TSEBT and IORT were excluded from the analysis.
Results
Major cancer incidence and the number of patients who received RT from 2017 to 2019 are shown in Table 1. The cancer incidence in 2020 has not yet been announced; hence, it has not been shown in Table 1. The number of cancer patients in major cancers increased from 124 453 in 2017 to 129 021 in 2019. The number of patients receiving RT for major cancers increased from 55 794 in 2017 to 59 094 in 2020.
The number of patients with major cancers who received radiotherapy from 2017 to 2019
| . | . | Year . | ||
|---|---|---|---|---|
| Type of Cancer | 2017 | 2018 | 2019 | |
| Lung (C33-C34) | Number of cancer patients per year (7) | 27 464 | 28 891 | 29 960 |
| Number of cases who received radiotherapy (%) | 14 594 (53.1%) | 15 424 (53.4%) | 16 232 (54.2%) | |
| Stomach (C16) | Number of cancer patients per year (7) | 30 082 | 29 408 | 29 493 |
| Number of cases who received radiotherapy (%) | 1341 (4.5%) | 1272 (4.3%) | 1229 (4.2%) | |
| Colorectum (C18-C20) | Number of cancer patients per year (7) | 28 596 | 28 186 | 29 030 |
| Number of cases who received radiotherapy (%) | 5871 (20.5%) | 6023 (21.4%) | 6158 (21.2%) | |
| Breast (C50) | Number of cancer patients per year (7) | 22 641 | 23 723 | 24 933 |
| Number of cases who received radiotherapy (%) | 30 166 (133.2%) | 30 350 (127.9%) | 30 701 (123.1%) | |
| Liver (C20) | Number of cancer patients per year (7) | 15 670 | 15 834 | 15 605 |
| Number of cases who received radiotherapy (%) | 3822 (24.4%) | 3954 (25.0%) | 3867 (24.8%) | |
| All major cancers | Number of cancer patients per year (7) | 124 453 | 126 042 | 129 021 |
| Number of cases who received radiotherapy (%) | 55 794 (44.8%) | 57 023 (45.2%) | 58 187 (45.1%) | |
| . | . | Year . | ||
|---|---|---|---|---|
| Type of Cancer | 2017 | 2018 | 2019 | |
| Lung (C33-C34) | Number of cancer patients per year (7) | 27 464 | 28 891 | 29 960 |
| Number of cases who received radiotherapy (%) | 14 594 (53.1%) | 15 424 (53.4%) | 16 232 (54.2%) | |
| Stomach (C16) | Number of cancer patients per year (7) | 30 082 | 29 408 | 29 493 |
| Number of cases who received radiotherapy (%) | 1341 (4.5%) | 1272 (4.3%) | 1229 (4.2%) | |
| Colorectum (C18-C20) | Number of cancer patients per year (7) | 28 596 | 28 186 | 29 030 |
| Number of cases who received radiotherapy (%) | 5871 (20.5%) | 6023 (21.4%) | 6158 (21.2%) | |
| Breast (C50) | Number of cancer patients per year (7) | 22 641 | 23 723 | 24 933 |
| Number of cases who received radiotherapy (%) | 30 166 (133.2%) | 30 350 (127.9%) | 30 701 (123.1%) | |
| Liver (C20) | Number of cancer patients per year (7) | 15 670 | 15 834 | 15 605 |
| Number of cases who received radiotherapy (%) | 3822 (24.4%) | 3954 (25.0%) | 3867 (24.8%) | |
| All major cancers | Number of cancer patients per year (7) | 124 453 | 126 042 | 129 021 |
| Number of cases who received radiotherapy (%) | 55 794 (44.8%) | 57 023 (45.2%) | 58 187 (45.1%) | |
The number of patients with major cancers who received radiotherapy from 2017 to 2019
| . | . | Year . | ||
|---|---|---|---|---|
| Type of Cancer | 2017 | 2018 | 2019 | |
| Lung (C33-C34) | Number of cancer patients per year (7) | 27 464 | 28 891 | 29 960 |
| Number of cases who received radiotherapy (%) | 14 594 (53.1%) | 15 424 (53.4%) | 16 232 (54.2%) | |
| Stomach (C16) | Number of cancer patients per year (7) | 30 082 | 29 408 | 29 493 |
| Number of cases who received radiotherapy (%) | 1341 (4.5%) | 1272 (4.3%) | 1229 (4.2%) | |
| Colorectum (C18-C20) | Number of cancer patients per year (7) | 28 596 | 28 186 | 29 030 |
| Number of cases who received radiotherapy (%) | 5871 (20.5%) | 6023 (21.4%) | 6158 (21.2%) | |
| Breast (C50) | Number of cancer patients per year (7) | 22 641 | 23 723 | 24 933 |
| Number of cases who received radiotherapy (%) | 30 166 (133.2%) | 30 350 (127.9%) | 30 701 (123.1%) | |
| Liver (C20) | Number of cancer patients per year (7) | 15 670 | 15 834 | 15 605 |
| Number of cases who received radiotherapy (%) | 3822 (24.4%) | 3954 (25.0%) | 3867 (24.8%) | |
| All major cancers | Number of cancer patients per year (7) | 124 453 | 126 042 | 129 021 |
| Number of cases who received radiotherapy (%) | 55 794 (44.8%) | 57 023 (45.2%) | 58 187 (45.1%) | |
| . | . | Year . | ||
|---|---|---|---|---|
| Type of Cancer | 2017 | 2018 | 2019 | |
| Lung (C33-C34) | Number of cancer patients per year (7) | 27 464 | 28 891 | 29 960 |
| Number of cases who received radiotherapy (%) | 14 594 (53.1%) | 15 424 (53.4%) | 16 232 (54.2%) | |
| Stomach (C16) | Number of cancer patients per year (7) | 30 082 | 29 408 | 29 493 |
| Number of cases who received radiotherapy (%) | 1341 (4.5%) | 1272 (4.3%) | 1229 (4.2%) | |
| Colorectum (C18-C20) | Number of cancer patients per year (7) | 28 596 | 28 186 | 29 030 |
| Number of cases who received radiotherapy (%) | 5871 (20.5%) | 6023 (21.4%) | 6158 (21.2%) | |
| Breast (C50) | Number of cancer patients per year (7) | 22 641 | 23 723 | 24 933 |
| Number of cases who received radiotherapy (%) | 30 166 (133.2%) | 30 350 (127.9%) | 30 701 (123.1%) | |
| Liver (C20) | Number of cancer patients per year (7) | 15 670 | 15 834 | 15 605 |
| Number of cases who received radiotherapy (%) | 3822 (24.4%) | 3954 (25.0%) | 3867 (24.8%) | |
| All major cancers | Number of cancer patients per year (7) | 124 453 | 126 042 | 129 021 |
| Number of cases who received radiotherapy (%) | 55 794 (44.8%) | 57 023 (45.2%) | 58 187 (45.1%) | |
Lung
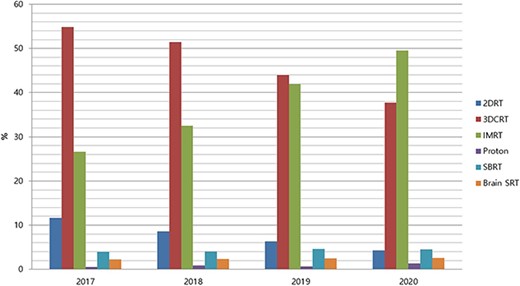
Between 2017 and 2020, the number of newly diagnosed patients with lung cancer steadily increased, and the number of patients receiving RT for lung cancer also increased (Table 1). In 2017, 3DCRT was the most common RT modality for patients with lung cancer (40.4%), followed by IMRT (29.6%). In 2020 with the increase in the number of patients receiving IMRT, IMRT accounted for 48.5% of all patients receiving RT, while 3DCRT accounted for 26.4%. The use of SBRT increased from 7% in 2017 to 8.2% in 2020, and that of brain SRT increased from 9.4% in 2017 to 11% in 2020. The use of 2DRT decreased from 12.5% in 2017 to 4.6% in 2020, while that of PRT has not changed enough to reach the 1% level (Fig. 1).
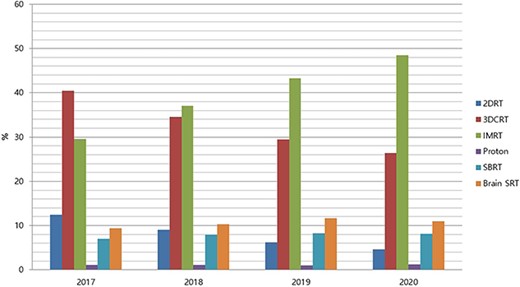
Proportion of radiotherapy modalities for lung cancer in Korea between 2017 and 2020 (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
Stomach
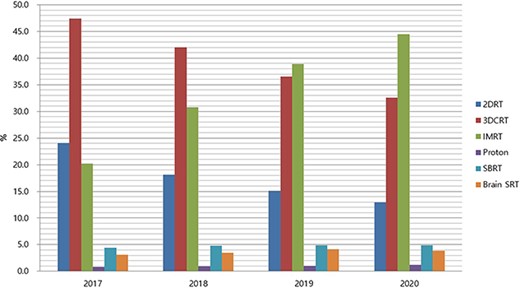
Compared with the incidence of stomach cancer, the number of patients receiving RT for it was low. About 30 000 new stomach cancer cases occurred, and 1341 stomach cancer patients received RT in 2017 (Table 1). In the case of stomach cancer, similar to lung cancer, the use of IMRT increased, and that of 2DRT and 3DCRT decreased. But the proportion of 3DCRT for stomach cancer (37.7%) was higher than that of lung cancer (26.4%) in 2020 (Fig. 2).
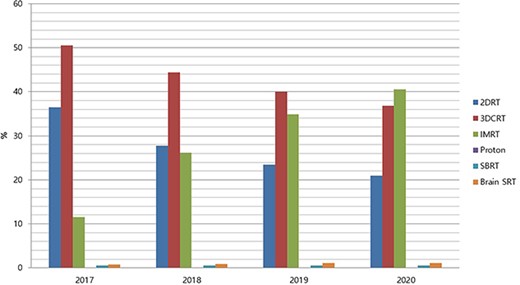
Proportion of radiotherapy modalities for stomach cancer in Korea between 2017 and 2020 (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
Colorectum
Between 2017 and 2020, the number of patients with colorectal cancer receiving RT did not change significantly (Table 1). In 2017, 3DCRT accounted for 53.3% of all colorectal cancer cases receiving RT, gradually decreasing to 37.5% in 2020, while the use of IMRT increased from 32.7% in 2017 to 49.7% in 2020. 2DRT use accounted for only 5.4% in 2017 but decreased further to 2.3% in 2020. There was no significant change in the use of SBRT, brain SRT and PRT for colorectal cancer (Fig. 3).
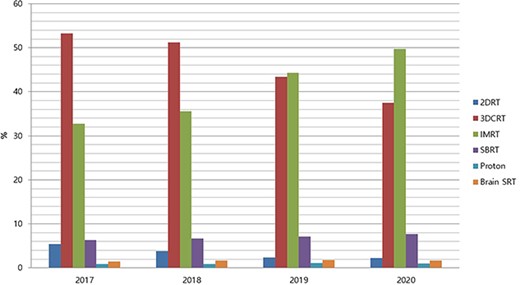
Proportion of radiotherapy modalities for colorectal cancer in Korea between 2017 and 2020 (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
Breast
From 2017 to 2020, the number of breast cancer patients receiving RT was higher than that of newly diagnosed breast cancer patients each year, and the number of RT patients has steadily increased (Table 1). In 2017, 3DCRT and 2DRT accounted for 87% of all RT modalities, but the use of 3DCRT and 2DRT decreased significantly from 50.5% and 36.5% in 2017 to 36.8% and 21% in 2020, respectively. Instead, the use of IMRT, which was 11.6% in 2017, became 40.5% in 2020. The number of cases where PRT, SBRT and brain SRT were used was ˂1%; hence, there was no difference (Fig. 4).
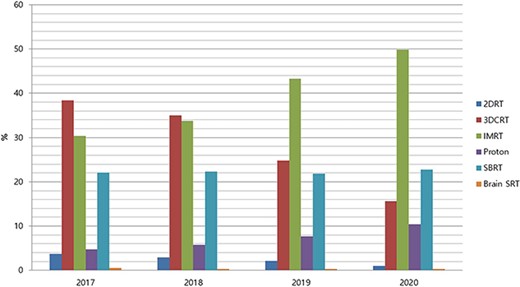
Proportion of radiotherapy modalities for breast cancer in Korea between 2017 and 2020 (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
Liver
For liver cancer, there were fewer patients receiving RT compared with the incidence rate. In 2017, there were 15 670 newly diagnosed patients with liver cancer, of which 3822 received RT (Table 1). There was no significant change in the incidence of liver cancer and the number of patients treated with RT for it between 2017 and 2020. In 2017, 3DCRT was the most common RT modality for liver cancer at 38.4%, followed by IMRT (30.4%) and SBRT (22.1%). However, the use of IMRT increased sharply thereafter, reaching 49.9%, followed by that of SBRT (22.8%) in 2020. In 2020, 3DCRT accounted for 15.6% of RT modalities. The number of patients who received PRT increased from 4.8% in 2017 to 10.4% in 2020. The use of 2DRT, which was 3.7% in 2017, decreased further to 1%. The use of brain SRT continued to be ˂1% from 2017 to 2020 (Fig. 5).
Proportion of radiotherapy modalities for liver cancer in Korea between 2017 and 2020 (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
All major cancers
3DCRT was the most commonly used modality among all forms of RT until 2018 (47.4% in 2017 and 42.0% in 2018), followed by IMRT (20.2% in 2017 and 30.8% in 2018), and from 2019 the use of IMRT (38.9% in 2019 and 44.5% in 2020) exceeded that of 3DCRT (36.5% in 2019 and 32.6% in 2020) (Fig. 6). The percentage of cancer patients who underwent RT for major cancer was 44.8% in 2017 and 45.1% in 2019.
Proportion of radiotherapy modalities for all major cancers in Korea between 2017 and 2020. In this study, major cancers refer to lung, stomach, colorectal, breast and liver cancers (2DRT, two-dimensional radiotherapy; 3DCRT, three-dimensional conformal radiotherapy; IMRT, intensity-modulated radiotherapy; PRT, proton radiotherapy; SBRT, stereotactic body radiotherapy; SRT, stereotactic radiotherapy).
Discussion
The use of RT for cancer patients in Korea has increased over the past decade, reaching 36.1% in 2019 (3). From 2017 to 2020, the number of patients who received RT for major cancers has also increased. Lee et al. reported that the rate of IMRT utilization had increased noticeably since 2016 (3). The NHIS coverage for IMRT has expended for almost all cancers since 2015. In Korea, implementation of IMRT has been partially covered for specific cancers (head and neck, brain, prostate and spinal cancers and re-irradiation cases) from 2011 and the coverage has expended to include almost all cancers since 2015 (7). SBRT has been partially covered by NHIS for specific cancers such as head and neck, spinal, medically inoperable lung, hepatobiliary, pancreatic and urinary cancers, oligometastases and re-irradiation cases from 2014 (8). NHIS of Korea coverage criteria for PRT expanded coverage criteria from childhood cancer alone to some adulthood cancers in 2015 (CNS, hand and neck, thoracic and abdominal malignancies except breast and prostate cancer) (9).
The trend for the use of RT for major cancers is the same as for all cancers. Our study found that 3DCRT was the most used modality among various RTs for major cancers until 2018, followed by IMRT, and from 2019 the use of IMRT exceeded that of 3DCRT. Overall, from 2017 to 2020, the use of 2DRT and 3DCRT decreased, and that of IMRT increased. There has been no increase in PRT facilities in Korea since 2015. Currently, it is only available at the National Cancer Center and Seoul Samsung Hospital. The number of patients receiving particle therapy is expected to increase with the introduction of the Heavy particle therapy facility in Yonsei Cancer Center in 2023. But there is still a lack of particle therapy facility in Korea, so there is no significant change compared with the total number of patients treated with RT.
In Korea, the RT utilization rate for total cancer patients nationwide was 24.5% in 2010, which consistently increased to 36.1% in 2019 (3). Our study shows that the rate of RT utilization was higher in patients with major cancer than that in patients with all forms of cancer, which was 44.8% in 2017 and 45.1% in 2019.
Lung
Since 2017, the number of lung cancer patients has been on the rise, and the use of RT for patients with lung cancer has been increasing; hence, the proportion of patients receiving RT among patients with lung cancer has remained similar.
RT plays a potential role in all stages of non-small cell lung cancer (NSCLC) as well as small cell lung cancer (SCLC). In the secondary analysis of radiation technique in NRG Oncology clinical trial RTOG 0617 (10), the patients treated with IMRT for locally advanced NSCLC had lower rates of severe pneumonitis than patients treated with 3DCRT despite these patients having larger and more advanced tumors. Hence, the authors concluded that IMRT should be used routinely for locally advanced NSCLC. National Comprehensive Cancer Network (NCCN) guideline also prefers IMRT over three-dimensional conformal EBRT on the basis of reduced toxicity in the setting of concurrent chemoRT (11). IMRT is also recommended for SCLC (11). In Korea, the use of IMRT for patients with lung cancer is rapidly increasing. Since 2018, the use of IMRT has overtaken 3DCRT, and in 2020, 48.5% of all RT for lung cancer was IMRT, approximately twice as much as 3DCRT and half of all RT patients.
SBRT for lung cancer increased slightly from 7% in 2017 to 8.2% in 2020. For node-negative early stage lung cancer, SBRT is an appropriate option for patients with high surgical risk (11). The Korean Association for Lung Cancer also recommends SBRT for early stage lung cancer if surgery is not performed due to poor lung/heart function, other medical conditions or refusal to operate (12).
The number of patients treated with PRT for lung cancer is ˂1% of all patients treated with RT for lung cancer. PRT for lung cancer accounted for 14% of PRT use in Korea between 2018 and 2019 (9). Several clinical trials comparing PRT with IMRT have shown no benefit in local control or survival (13,14), but a single prospective non-randomized trial reported that PRT is associated with lower rates of grade ≥3 cardiopulmonary toxicity (13).
Notably, the utilization rate of brain SRT among RT modalities for lung cancer is higher than that of SBRT. Several studies have suggested that aggressive management of NSCLC patients with synchronous brain-only metastasis is associated with improved survival (15,16). Based on these promising results, it is believed that aggressive treatment for brain metastasis is performed.
Stomach
The incidence of gastric cancer has been on the decline in the past decade in Korea (17). Compared with the incidence of stomach cancer, the number of patients receiving RT for it was low. The RT utilization rate for stomach cancer was 4.5% in 2017, 4.3% in 2018 and 4.1% in 2019. Although the number of patients receiving RT for gastric cancer was smaller than that of other cancers, the pattern of changes in RT modalities was similar, resulting in an increase in the use of IMRT and a decrease in the use of 2DRT and 3DCRT.
Colorectum
In HIRA data, the colorectal cancer codes were combined into C18, C19 and C20. As such, it was impossible to separate and analyze RT patterns for colon and rectal cancer individually.
Seo et al. reported that the number of colorectal cancer patients treated with RT had not increased between 2011 and 2015 (5). Moreover, between 2017 and 2020, the number of patients with colon cancer receiving RT did not change significantly. However, the modalities of RT have changed in that 3DCRT, which accounted for ˃50% (53.3%) of all RT in 2017, decreased to about one-third (37.5%) in 2020, while IMRT, which accounted for approximately one-third (32.7%) of all RTs in 2017, accounted for almost 50% (49.7%) in 2020.
The use of 2DRT was as low as 5.4% in 2017 and then decreased further to 2.3% in 2020, which is believed to be due to the wide use of 3DCRT for curative treatment for rectal cancer in the early 3DCRT era, fearing side effects during pelvic irradiation. NCCN guidelines also highly recommend the use of conformal RT, such as 3DCRT, IMRT and SBRT (11). In patients with minimal liver or lung metastasis, SBRT is considered to be a good option (18). SBRT use accounted for 6.3% in 2017 and 7.7% in 2020 of the proportion of RT modalities for colorectal cancer.
Breast
In 2019, the number of breast cancer cases was 259 116, ranking third among all cancers in Korea (462 151 for thyroid cancer and 318 948 for stomach cancer). Among cancers in women, the incidence of breast cancer is the second highest, following thyroid cancer (377 586) (17). Between 2017 and 2020, breast cancer has had a higher number of patients receiving RT than its incidence rate. This is because the survival rate and prevalence of breast cancer is high, and there is a possibility of recurrence even after decades. In 2017, 3DCRT and 2DRT accounted for 87% of all RT modalities but decreased significantly to 57.8% in 2020. Among patients receiving RT for breast cancer, 2DRT accounted for 36.5% in 2017 and 21% in 2020, which is not decreasing compared with other cancers.
Instead, the use of IMRT increased from 11.6% in 2017 to 40.5% in 2020. Huh et al. reported that head and neck cancer was the most frequently treated cancer with IMRT in 2011; however, it was replaced by breast cancer in 2018 (7). According to the American Society for Radiation Oncology (ASTRO)'s Choosing Wisely list in 2013 (19), routine use of IMRT is not recommended for whole breast cancer as part of breast conservation therapy because the term ‘IMRT’ has generally been applied to describe methods as field-in-field 3DCRT. However, the ASTRO withdrew this recommendation in July 2022. In 2018, the ASTRO guideline for whole breast irradiation was published (20). According to this guideline, 3DCRT with a ‘field-in-field’ technique is still recommended as the initial treatment approach for whole breast RT. However, the NCCN guideline recommends IMRT is one of the treatment options for improved homogeneity of the target dose and sparing of normal issues, compared with the routine use of three-dimensional computed tomography-based treatment planning and the use of compensators such as wedges or forward planning (11). IMRT is one of the effective treatments for partial breast irradiation in early stage low risk breast cancer patients (21).
Liver
Liver cancer had fewer patients receiving RT compared with its incidence rate. In Korea, the RT utilization rate for liver cancer was 24.4% in 2017, 24.9% in 2018 and 24.8% in 2019.
The role of RT for liver cancer is gradually expanding. The Korean Liver Cancer Association published the 2022 Korea Practice Guidelines for the Management of Hepatocellular Carcinoma in June 2020 (22). According to this guideline, RT can be performed in liver cancer when hepatic resection, liver transplantation, local modalities or transarterial chemoembolization (TACE) is difficult. Moreover, RT can be performed for liver cancer patients who exhibit an incomplete response to TACE or those with portal vein invasion. RT and systemic treatment can be performed parallelly for patients with liver cancer. This guideline does not recommend any specific RT modality.
NCCN guideline also recommends RT as a treatment option for patients with unresectable disease or for those who are medically inoperable due to comorbidity; however, NCCN guidelines do not recommend the specific RT modality (11). In 2017, 3DCRT was the most common RT modality for liver cancer, followed by IMRT and SBRT. However, in 2020 IMRT use increased rapidly, reaching about half of all the cases using RT, followed by SBRT and 3DCRT. In our study, SBRT steadily occupied ˃20% of RT for liver cancer from 2017. SBRT can be considered as an alternative to radiofrequency ablation. Moreover, SBRT appears to be a reasonable first-line treatment for larger tumors ˃3 cm (23).
The number of PRT patients among all RT patients is small, but the number of PRT patients is steadily increasing every year. Liver cancer is the most common primary cancer receiving PRT (9). In Korea, the number of patients who received PRT for liver cancer increased from 4.8% in 2017 to 10.4% in 2020.
Overall
While analyzing the HIRA big data based on NHIS, it was thought that several improvements were needed in the national cancer patient statistics. In HIRA data, it was impossible to analyze RT use of rectal cancer alone because the codes of colorectal cancer were combined into C18-C20 in HIRA data. Also, if patients who had the specific cancer diagnostic codes with RT codes were selected, there was no way to determine whether this RT was the first RT after diagnosis or after recurrence or palliative RT.
In the future, when constructing such big national data, it is necessary to design data information well from the beginning. In addition, it is thought that continuous improvement is needed by coordinating opinions with related academic societies.
Conclusions
The rate of RT utilization was higher in patients with major cancer than in all cancer patients. The overall trend is to use more sophisticated RT, such as IMRT and SBRT. However, 2DRT and 3DCRT still play a substantial role in the treatment of major cancers.
This study is meaningful because it examines the trend of RT in cancers with high incidence rates. In the future, we hope to analyze changes in RT trends in other cancers.


