-
PDF
- Split View
-
Views
-
Cite
Cite
Sangshin Park, Ian C Michelow, Young June Choe, Shifting Patterns of Respiratory Virus Activity Following Social Distancing Measures for Coronavirus Disease 2019 in South Korea, The Journal of Infectious Diseases, Volume 224, Issue 11, 1 December 2021, Pages 1900–1906, https://doi.org/10.1093/infdis/jiab231
Close - Share Icon Share
Abstract
We hypothesized that nationwide social distancing and other preventive measures for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were associated with reduced detection of other respiratory viruses in South Korea.
We analyzed national surveillance data to compare incidence of respiratory viruses during 2016–2019 vs 2020. Results of multiplex reverse-transcription polymerase chain reaction assays for 8 respiratory viruses were included: adenovirus (ADV), parainfluenza virus (PIV), respiratory syncytial virus (RSV), influenza virus (IFV), human coronavirus (HCoV; non–SARS-CoV-2), human rhinovirus (HRV), human bocavirus (HBoV), and human metapneumovirus (HMPV).
During 2016–2019, rates of detection of respiratory viruses were relatively stable: ADV, 3.7%–9.2%; PIV, 1.4%–17.0%; RSV, 0.3%–15.3%; IFV, 0.4%–35.6%; HCoV, 1.5%–8.4%; HRV, 7.0%–25.1%; HBoV, 0.6%–6.3%; and HMPV, 0.7%–14.5%. Following implementation of social distancing in February 2020, rates of detection of enveloped viruses (HCoV, HMPV, IFV, PIV, and RSV) were significantly reduced by up to 100%. However, nonenveloped viruses (ADV, HRV, and HBoV) persisted throughout 2020, and HRV rates in hospitalized patients significantly increased.
After implementation of social distancing for SARS-CoV-2 in South Korea, rates of detection of enveloped respiratory viruses decreased significantly, whereas nonenveloped viruses persisted, suggesting that enhanced infection prevention strategies are required to mitigate spread of these viruses.
As severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disseminated rapidly throughout the world in 2020, many countries implemented statewide social distancing measures and other preventive interventions to mitigate the spread of coronavirus disease 2019 (COVID-19) [1]. These strategies have been shown to delay outbreaks and flatten the epidemic curve in various settings [2–4]. Moreover, social distancing has been associated with the additional benefit of reducing the incidence of other communicable diseases such as those caused by respiratory syncytial virus (RSV) and influenza virus (IFV) [5–12]. However, it is not currently known what effect public health interventions have on other respiratory viruses [13]. The sparse published data indicate that emergence of human rhinoviruses during the COVID-19 pandemic coincided with relaxation of social distancing measures and school reopening in single cities in the United Kingdom [14] and Australia [15].
The system for national surveillance of respiratory viruses in South Korea collates results from multiplex reverse-transcription polymerase chain reaction (RT-PCR) assays from across the country. We analyzed national data from 2016 to 2020 to describe the impact of sequential social distancing interventions on common respiratory viruses in the context of universal face mask use and hand hygiene implemented in early 2020. In this study, we hypothesized that statewide public health responses were associated with reductions in incidence rates of common respiratory viruses in South Korea during 2020.
METHODS
Social Distancing Measures
In response to the outbreak of COVID-19 in China, South Korea mandated universal use of face masks and recommended modified personal behavior including physical distancing starting in February 2020. As cases surged in South Korea, social distancing was instituted at the national level with varying levels of restrictions from March 2020 onward (Figure 1, Table 1) [16]. The coordinated public health response enforced limits on gatherings in various congregate settings including entertainment venues, places of worship, schools, sporting events, and work environments (Table 1). Stringent social distancing schemes were enforced between 21 March and 5 May 2020 and were replaced on 6 May 2020 with less restrictive physical distancing in daily life when the number of cases declined [17, 18]. The public health strategy changed to a 3-tier scheme on 28 June 2020 (Figure 1) and subsequently to a 5-level model on 17 November 2020 (Table 1) to permit maximum flexibility in response to social and economic upheaval caused by the epidemic.
Five-Tier Social Distancing System in Response to Coronavirus Disease 2019 Outbreak, South Korea
| Social Distancing . | Level 1 . | Level 1.5 . | Level 2 . | Level 2.5 . | Level 3 . |
|---|---|---|---|---|---|
| Gathering limits | 500 (preauthorization) | 100 (festivals) | 100 (all events) | 50 (all events) | 10 (all events) |
| Schools | Density control 2/3 | Density control 2/3 | Density control 1/3 | Density control 1/3 | Distance learning |
| Work environment | Density control 1/5 | Density control 1/3 | Density control 1/3 | Density control 1/3 | Distance working |
| Places of worship | Spacing between people | 30% attendance | 20% attendance | <20 people | Distance service |
| Sporting events | 50% audience | 30% audience | 10% audience | No audience | Stop games |
| Social Distancing . | Level 1 . | Level 1.5 . | Level 2 . | Level 2.5 . | Level 3 . |
|---|---|---|---|---|---|
| Gathering limits | 500 (preauthorization) | 100 (festivals) | 100 (all events) | 50 (all events) | 10 (all events) |
| Schools | Density control 2/3 | Density control 2/3 | Density control 1/3 | Density control 1/3 | Distance learning |
| Work environment | Density control 1/5 | Density control 1/3 | Density control 1/3 | Density control 1/3 | Distance working |
| Places of worship | Spacing between people | 30% attendance | 20% attendance | <20 people | Distance service |
| Sporting events | 50% audience | 30% audience | 10% audience | No audience | Stop games |
Five-Tier Social Distancing System in Response to Coronavirus Disease 2019 Outbreak, South Korea
| Social Distancing . | Level 1 . | Level 1.5 . | Level 2 . | Level 2.5 . | Level 3 . |
|---|---|---|---|---|---|
| Gathering limits | 500 (preauthorization) | 100 (festivals) | 100 (all events) | 50 (all events) | 10 (all events) |
| Schools | Density control 2/3 | Density control 2/3 | Density control 1/3 | Density control 1/3 | Distance learning |
| Work environment | Density control 1/5 | Density control 1/3 | Density control 1/3 | Density control 1/3 | Distance working |
| Places of worship | Spacing between people | 30% attendance | 20% attendance | <20 people | Distance service |
| Sporting events | 50% audience | 30% audience | 10% audience | No audience | Stop games |
| Social Distancing . | Level 1 . | Level 1.5 . | Level 2 . | Level 2.5 . | Level 3 . |
|---|---|---|---|---|---|
| Gathering limits | 500 (preauthorization) | 100 (festivals) | 100 (all events) | 50 (all events) | 10 (all events) |
| Schools | Density control 2/3 | Density control 2/3 | Density control 1/3 | Density control 1/3 | Distance learning |
| Work environment | Density control 1/5 | Density control 1/3 | Density control 1/3 | Density control 1/3 | Distance working |
| Places of worship | Spacing between people | 30% attendance | 20% attendance | <20 people | Distance service |
| Sporting events | 50% audience | 30% audience | 10% audience | No audience | Stop games |
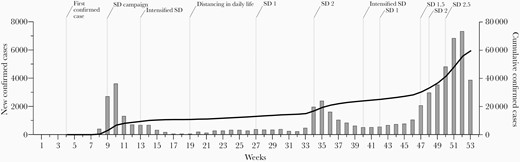
Weekly number of laboratory-confirmed coronavirus disease 2019 cases, South Korea, 2020. Levels of social distancing (SD) are indicated by 1, 1.5, 2, and 2.5 (see Table 1).
Respiratory Virus Surveillance
Respiratory virus activity in South Korea is monitored at the national level through 2 networks: the laboratory sentinel surveillance system (Korea Influenza and Respiratory Virus Surveillance System) and the clinical sentinel surveillance system [19, 20]. The laboratory sentinel surveillance system collects results of laboratory tests for respiratory specimens obtained from nonhospitalized patients with respiratory symptoms who visited 52 outpatient clinics in 17 cities and provinces [21]. This system reports weekly detection rates of respiratory viruses, which are calculated by dividing the number of positive specimens by the total number of tests performed (Supplementary Table 1). The clinical sentinel surveillance system collects data from hospitalized cases who have been confirmed to be infected with infectious disease pathogens while displaying clinical symptoms consistent with acute respiratory infection [22]. Hospitalized cases are reported from 214 nationally distributed sentinel hospitals. This system reports the number of unique patients hospitalized with respiratory viruses each week at sentinel hospitals (Supplementary Table 2). All submitted and reported data are de-identified and publicly available.
Data Analyses
We analyzed all available national surveillance data for respiratory virus activity in children and adults to compare longitudinal trends in incidence for 2016–2019 vs 2020. The surveillance system collects results of multiplex RT-PCR assays for 8 human respiratory viruses: adenovirus (ADV), parainfluenza virus (PIV), RSV, IFV, human coronavirus (HCoV; non–SARS-CoV-2), human rhinovirus (HRV), human bocavirus (HBoV), and human metapneumovirus (HMPV) [19, 20]. The detection rate was defined as the percentage of respiratory specimens submitted for multiplex RT-PCR testing that yielded a positive result. Test results of hospitalized patients are reported here as detection rates (%) and ranges per month, and interval changes in detection rates (%) between 2016–2019 and 2020 for each virus. We tested statistical differences in detection rates using χ 2 or Fisher exact tests. Outpatient results are reported as the mean weekly incidence and range per month, and changes in incidence between 2016–2019 and 2020. We tested statistical differences of these data using Wilcoxon rank-sum tests. We performed statistical analysis using SAS version 9.4 software (SAS Institute, Cary, North Carolina). A P value < .05 was considered to be statistically significant.
Ethics Statement
This study involved secondary analysis of publicly available de-identified data that did not constitute human subjects research and was exempted by the Hallym University Institutional Review Board (HIRB-2020-EX005).
RESULTS
The number of submitted respiratory specimens among hospitalized patients peaked each year in January (n = 5127 for 2016–2019 vs n = 1490 for 2020). During 2016–2019, the statewide monthly detection rates for respiratory viruses in hospitalized patients varied for ADV (3.7%–9.2%), PIV (1.4%–17.0%), RSV (0.3%–15.3%), IFV (0.4%–35.6%), HCoV (1.5%–8.4%), HRV (7.0%–25.1%), HBoV (0.6%–6.3%), and HMPV (0.7%–14.5%) (Figure 2, Supplementary Table 1). Following the introduction of statewide social distancing measures in early 2020 (Figure 1), substantial and significant reductions in the monthly proportion of positive specimens (PPS; %) relative to the corresponding PPS during 2016–2019 were observed from March onward for PIV (–88.1% to –100%), RSV (–82.1% to –100%), IFV (–98.5% to –100%), HCoV (–52.2% to –100%), and HMPV (–85.3% to –100%). On the other hand, although the monthly PPS fluctuated widely for ADV (+76.0% to –50.5%), HRV (+135.8% to –72.1%), and HBoV (+1871.8% to –82.6%), these 3 viruses continued to be detected at varying rates throughout 2020 (Figure 2, Supplementary Table 1).
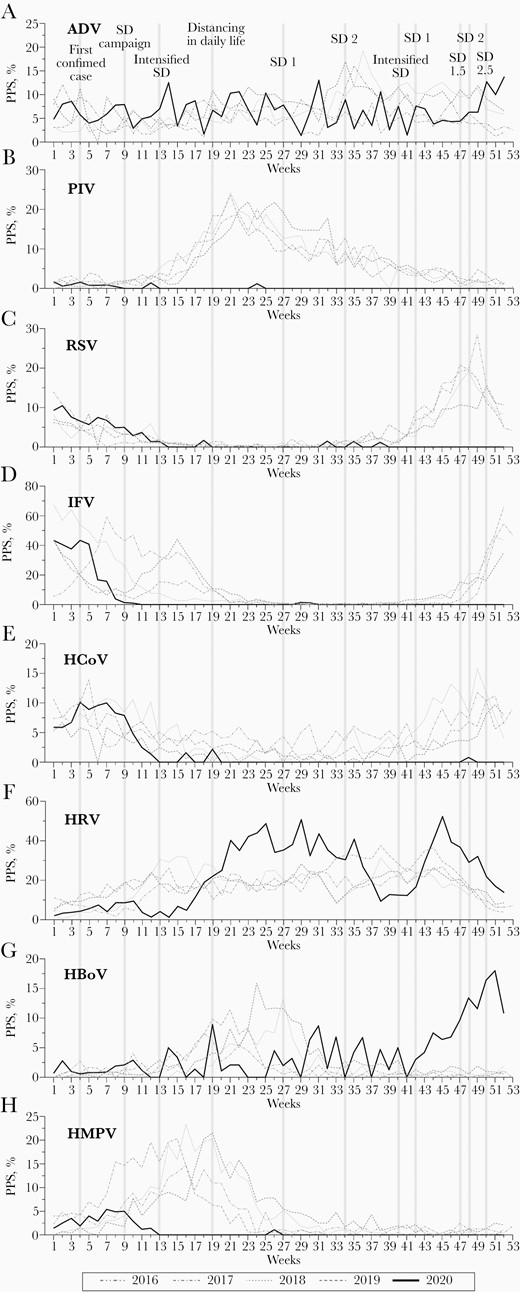
A–H, Monthly detection rates of respiratory viruses in hospitalized patients from the national surveillance system for influenza and respiratory viruses, South Korea, 2016–2019 vs 2020. Abbreviations: ADV, adenovirus; HBoV, human bocavirus; HCoV, human coronavirus (non–severe acute respiratory syndrome coronavirus 2); HMPV, human metapneumovirus; HRV, human rhinovirus; IFV, influenza virus; PIV, parainfluenza virus; PPS, proportion of positive specimens; RSV, respiratory syncytial virus; SD, social distancing.
The weekly incidence of respiratory viruses detected in outpatients during 2016–2019 vs 2020 are shown in Figure 3 and Supplementary Table 2. Mean monthly incidences for 2016–2019 varied for each virus as follows: ADV, 118–316 cases; PIV, 33–455; RSV, 12–1042; IFV, 12–983; HCoV, 16–286; HRV, 228–661; HBoV, 34–271; and HMPV, 15–412 (Supplementary Table 2). After social distancing measures were implemented in 2020, there were significant decreases in monthly mean incidence rates after March 2020 relative to 2016–2020 for all observed viruses: ADV (–77.8% to –94.9%), PIV (–86.2% to –99.0%), RSV (–68.5% to –99.9%), IFV (–63.1% to –99.0%), HCoV (–43.7% to –99.3%), HRV (–60.4% to –93.8%), HBoV (–49.7% to –96.6%), and HMPV (–94.9% to –100%) (Figure 3, Supplementary Table 2).
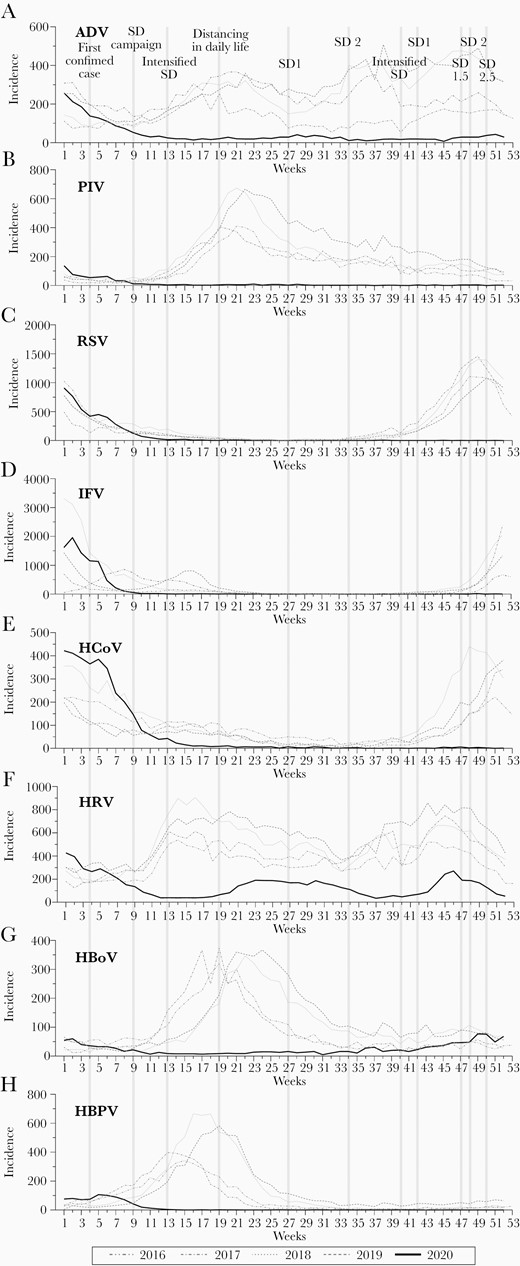
A–H, Monthly incidence of respiratory viruses in outpatients from the national surveillance system for influenza and respiratory viruses, South Korea, 2016–2019 vs 2020. Abbreviations: ADV, adenovirus; HBoV, human bocavirus; HCoV, human coronavirus (non–severe acute respiratory syndrome coronavirus 2); HMPV, human metapneumovirus; HRV, human rhinovirus; IFV, influenza virus; PIV, parainfluenza virus; RSV, respiratory syncytial virus; SD, social distancing.
Discussion
In this nationwide epidemiological study in South Korea, we demonstrated that the rate of detection of IFV and RSV decreased substantially in 2020 from a historical baseline rate in both hospitalized patients and outpatients after implementation of social distancing for COVID-19. These findings align with other investigations [6–12, 23]. In addition, we report that HCoV (non–SARS-CoV-2), HMPV, and PIV rates were significantly lower in 2020 than during 2016–2019, which expands previously published evidence supporting the role of social distancing and other protective measures against the transmission of several common respiratory viruses. The only other study that showed significant reductions in the detection rates of HMPV and PIV was performed at a single center in Israel [24].
On the other hand, ADV, HRV, and HBoV persisted throughout 2020 in hospitalized patients and to a lesser extent in outpatients, despite intensive public health interventions. The precise reasons for variation in rates of transmission between these and other respiratory viruses are not known, but are likely attributable to differences in certain intrinsic virological properties. The 95% confidence intervals (CIs) for incubation periods of many respiratory viruses overlap as follows: ADV, 5–6 days; PIV, 2–3 days; RSV, 4–5 days; HRV, 1–2 days; HCoV, 3–4 days; IFV, 0.5–1.5 days [25, 26]. Infectious periods are also similar, for example, 1–21 days for RSV, 1–9 days for IFV, and 7–16 days for HRV [27]. HRV has a basic reproduction number of 1.2–1.8, length of hospital stay of 0.4–1.7 days, and case fatality proportion of 0–0.125%, which is similar to other respiratory viruses. Therefore, these HRV characteristics do not appear to mediate higher risk of viral transmission despite social distancing measures implemented in South Korea. Our finding that HRV persisted in South Korea during 2020 aligns with a study from Hong Kong, where multiple HRV outbreaks were reported [28]. In another study, investigators in Southampton, United Kingdom reported that all tested respiratory viruses initially decreased in 2020 following the nationwide lockdown. However, 2 weeks after reopening schools in that city, there was a sharp increase in the detection of HRV in adults, suggesting that the virus had spread from schools to the broader community [14]. HRV also resurged in Sydney, Australia after relaxation of social distancing measures [15]. In South Korea, schools were closed in March and reopened in May 2020 while the authorities continued to minimize crowding and maintain mask and hand hygiene policies [29]. Nevertheless, HRV surged after schools reopened and decreased only after intensification of social distancing rules. It is possible that early social distancing measures reduced exposure to HRV during the typical transmission season from January through March, which resulted in attenuated acquired immunity and a delayed surge in the fall when social distancing was relaxed. The resurgence was controlled after public health interventions were reintensified. Overall, rates of HRV in hospitalized patients in South Korea were higher during 2020 than during 2016–2019, although smaller numbers of respiratory samples were submitted for testing in 2020. Despite the large HRV resurgences, transmission of SARS-CoV-2 remained low in South Korean school-aged children [30], indicating that different methods of transmission were likely responsible. It is notable that in the setting of preemptive testing strategy implemented in Korea, there was no significant age-specific differences in the detection rate of COVID-19 in tested cases [31], suggesting that similar proportions of children and adults were tested.
The relative importance of respiratory droplets, aerosols, contaminated fomites, and direct human contact as modes of spread for respiratory viruses is well recognized [32]. However, the nuanced differences in the mechanisms of transmission of ADV, HRV, and HBoV vs SARS-CoV-2 and other respiratory viruses have not been clearly defined. Relevant factors that determine spread of pathogens include (1) virological features such as virulence, fitness, and transmissibility (expressed as the basic reproduction number, R0), immune evasion, and seasonal variations [33]; (2) host characteristics such as age, comorbidities, asymptomatic viral carriage, personal hygiene, and proximity to other hosts; and (3) environmental conditions such as temperature, humidity, and contamination of surfaces [34]. The common virological feature missing in ADV, HRV, and HBoV but present in all other respiratory viruses is the viral envelope [35]. The absence of a lipid bilayer envelope renders these viruses more resistant to inactivation by routine surface cleaning and disinfectants, desiccation, and heat, which may explain their year-round persistence and ability to spread despite universal infection preventive measures [36]. Therefore, enhanced infection control strategies may be required to counter the biophysical robustness of these virions that enable them to survive on surfaces for extended periods.
In addition to having a favorable impact on respiratory tract diseases [9, 13, 37, 38], social distancing in the era of COVID-19 also reduced nonrespiratory communicable diseases. In 2020, the cumulative incidences of chickenpox and mumps in South Korea were 36.4% (95% CI, 23.9%–76.3%) and 63.4% (95% CI, 48.0%–93.3%) of the predicted incidence [39]. In the Northern Territory of Australia, there was a decline in communicable enteric illnesses, particularly shigellosis and rotavirus, after social distancing measures and border controls were introduced [40]. Although pooled analysis of randomized controlled trials (RCTs) and cluster RCTs showed uncertainty about the effect of physical interventions in preventing respiratory virus outbreaks [41], the findings from numerous studies from around the world referenced above, including the current findings, suggest that social distancing and other public health responses have an additive suppressive effect on communicable diseases.
There are several limitations to this retrospective study. First, the national laboratory surveillance system is a passive scheme and as such is subject to selection bias because of the subjectivity of healthcare providers and variations in individuals’ health-seeking behavior. Temporal changes in social distancing protocols during 2020 also may have impacted individuals’ interaction with the healthcare system, possibly leading to detection bias, especially related to the outpatient data. Considering that healthcare in South Korea is operated under a single-payer system, the National Health Insurance Service, accurate utilization data are available. Compared to 2017–2019, it was estimated that there was a 3.5% decline in outpatient visits nationally in 2020 [22]. The rates of respiratory sample submissions in 2020 were lower than those of 2016–2019 and have declined progressively during the year, which may have introduced reporting bias. In addition, positive results of viral molecular studies, which are highly sensitive and specific, may indicate active disease, asymptomatic infection, or prolonged shedding. A second limitation was that demographic information such as age and sex was not available. Therefore, the role of children and school attendance in driving viral transmission cannot be inferred from our data. Future research that analyzes age stratification could be valuable, as previous studies have identified age-specific differences in respiratory virus incidences [42]. An additional limitation was that we could not confirm if individuals were adherent to public health mandates, nor could we determine whether social distancing, wearing face masks, or hand and environmental hygiene had a dominant impact on preventing transmission of respiratory viruses. Nevertheless, this national epidemiological study fills an important knowledge gap in characterizing the impact of widescale public health interventions on the detection of common respiratory viruses. Furthermore, our findings are representative of an entire country and are generalizable to other countries with a comparable socioeconomic status, healthcare infrastructure, and climatic conditions.
Conclusions
Social distancing and other preventive interventions that were implemented for COVID-19 in South Korea in 2020 had the added benefit of reducing the activity of several common enveloped respiratory viruses. On the other hand, the nonenveloped respiratory viruses (ADV, HRV, and HBoV) continued to be detected during 2020. To improve the overall public health response to all circulating respiratory viruses including SARS-CoV-2, enhanced interventions targeting nonenveloped viruses are required to mitigate their ongoing transmission.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Potential conflicts of interest. All authors: No reported conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.




