-
PDF
- Split View
-
Views
-
Cite
Cite
Pamela P Martinez, Ayesha S Mahmud, Mohammad Yunus, A S G Faruque, Tahmeed Ahmed, Mercedes Pascual, Caroline O Buckee, Tube Well Use as Protection Against Rotavirus Infection During the Monsoons in an Urban Setting, The Journal of Infectious Diseases, Volume 221, Issue 2, 15 January 2020, Pages 238–242, https://doi.org/10.1093/infdis/jiz436
Close - Share Icon Share
Abstract
Rotavirus, a diarrheal pathogen spread via fecal-oral transmission, is typically characterized by a winter incidence peak in most countries. Unlike for cholera and other waterborne infections, the role of sanitation and socioeconomic factors on the spatial variation of rotavirus seasonality remains unclear. In the current study, we analyzed their association with rotavirus seasonality, specifically the odds of monsoon cases, across 46 locations from 2001 to 2012 in Dhaka. Drinking water from tube wells, compared to other sources, has a clear protective effect against cases during the monsoon, when flooding and water contamination are more likely. This finding supports a significant environmental component of transmission.
Rotavirus is the most common cause of diarrheal deaths among children <5 years old worldwide, causing >215 000 deaths in 2013 [1]. Globally, rotavirus exhibits significant heterogeneity in seasonality. The highest incidence typically occurs during cooler and dryer seasons in most countries [2]. In some regions, where the disease tends to have a more endemic transmission, an additional peak occurs during the summer or monsoon season, for reasons that are not well defined [3, 4]. Bangladesh is an example of a country with high incidence all year round, particularly in Dhaka, the capital city, where high temperatures, low humidity, and flooding events have been associated with an increased risk for rotavirus [5]. Current dogma suggests that person-to-person contact is the dominant mode of transmission of the virus, although it has been shown to persist in water [6] and to respond to climatic changes [7]. Dhaka has >18 million inhabitants and a population growth of about 4% annually, making it one of the densest and fastest-growing megacities in the world. Heterogeneities in urbanization within Dhaka have been previously shown to affect the sensitivity and interannual variability of rotavirus to climate forcing [7].
In the current study we looked at the extent to which specific indicators of socioeconomic and sanitary conditions within Dhaka are associated with rotavirus seasonality. We leverage spatial variation in seasonal patterns across 11 years of data, to identify the external factors that are associated with disease transmission at different times of the year. This is of particular relevance in endemic settings such as Bangladesh, where rotavirus incidence remains high and vaccine effectiveness is still low [8].
METHODS
Data
A total of 8481 confirmed rotavirus cases between 2001 and 2016 were obtained from the Dhaka Hospital, through the ongoing surveillance program of the International Centre for Diarrheal Disease Research, Bangladesh. Stool samples were collected to determine the presence of enteric pathogens using an enzyme-linked immunosorbent assay, for every 50th patient attending the hospital for treatment of diarrhea. Each case in the data set includes the residence location (thana) of the patient. Because the administrative boundaries of each thana within the Dhaka metropolitan area changed during the period of our analysis, we aggregated the data for newer, smaller administrative units to match the 2001 boundary definitions, resulting in a total of 46 locations (Supplementary Figure 1). This ensures that the spatial patterns are consistent across the period of analysis. For a random subset of patients (about 11%) who tested positive for rotavirus between January 2001 and May 2012 (658 of the 5833 confirmed cases for this period), we have additional demographic and socioeconomic information from a survey administered to the patients (Supplementary Tables 1 and 2).
Statistical Analysis
We characterized the spatial heterogeneity of rotavirus seasonality by classifying cases into “monsoon cases” (April–September) and “winter cases” (January–March or October–December), aggregated for each location. We computed the Moran index (Moran I) to examine spatial patterns in rotavirus seasonality. The global Moran I was used to measure the degree of spatial autocorrelation in the fraction of cases occurring during the monsoon across all locations in our data; the local Moran I was computed to identify local spatial clusters. The Moran statistics were calculated assuming that neighboring locations had equal weight. We used a contiguity neighbor definition based on neighbors sharing ≥1 polygon vertex, but our results are robust to using a distance-based neighbor definition (Supplementary Figure 2). We computed pseudo P values for the Moran statistics by comparing the observed values to a sampling distribution of Moran I values generated using a random distribution assumption.
We used a generalized linear mixed-effects model to identify the relative importance of demographic, economic, and sanitary conditions on the likelihood of cases occurring during the monsoon season relative to the rest of the year. The outcome of interest is a binary variable indicating whether or not a case occurred during the monsoon season. Specifically, we modeled the log odds of the outcome variable as a linear combination of a set of independent variables and a random effect for each location. The full model specification is as follows:
where Yik is the log-odds of a case occurring in the monsoon season for individual i in location k; β 0, the intercept (grand mean across all individuals and locations); Xj,ik, a set of individual-level independent variables; β j, the corresponding estimated fixed effects; and uk, the estimated random effects (location-specific deviation from the grand mean). The random effects are assumed to be normally distributed with a mean of 0 and a variance of σ 2k.
We tested 3 sets of fixed effects at the individual level: (1) demographic factors (age and sex); (2) sanitary conditions (use of tube well [long stainless-steel tube or pipe bored into an underground aquifer], defecating in the open, and treatment of drinking water); and (3) socioeconomic factors (father’s income and the roofing material of the individual’s house). All continuous independent variables were normalized to have a mean of 0 and a standard deviation of 1. Variables for the analysis were selected based on the 3 categories. We compared models containing combinations of the different sets of independent variables (Supplementary Table 3), and we report results for the full model including all variables and for the model with the lowest Akaike information criterion. The 95% confidence intervals for the fixed effect estimates were computed using a simulation method developed by Gelman and Hill [9], implemented in the R package merTools. The confidence intervals for the fixed effects are estimated assuming that the conditional modes of the random effects are fixed.
RESULTS
The average annual fraction of rotavirus cases during the monsoon season exhibits a strong latitudinal gradient across the locations in our data, with locations in the south and in the Dhaka metropolitan area experiencing a higher percentage of cases during this season (Figure 1A). We detected significant spatial autocorrelation in rotavirus seasonality (global Moran I = 0.37; P < .05) and the existence of spatial clustering, indicated by a significant local Moran I statistic, particularly in the north of the city (Figure 1B). The clustering of locations in the north captures locations that have a low fraction of cases during the monsoons surrounded by locations whose fraction is low.
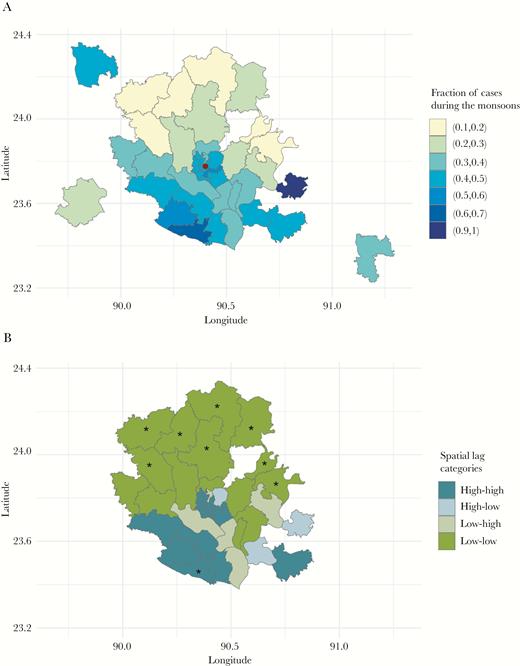
Rotavirus seasonality. A, Average annual fraction of rotavirus cases occurring during the monsoon season for each location, based on 16 years of data. (Red dot indicates location of the Dhaka Hospital.) B, Spatial clusters in rotavirus seasonality identified using the local Moran index (I) statistic. Asterisks represent locations with a significant local Moran I statistic (pseudo P < .05); colors represent the type of spatial classification. High-high indicates locations with a high fraction of cases during the monsoons that are surrounded by other locations with a high fraction; high-low, locations with a high fraction surrounded by locations with a low fraction; low-high, locations with a low fraction surrounded by locations with a high fraction; and low-low, locations with a low fraction surrounded by other locations with a low fraction. Map showing residence locations, within and outside Dhaka metropolitan area, for rotavirus patients at the Dhaka Hospital.
To characterize the indicators associated with the spatial heterogeneity in the seasonality of the aggregated data, we analyzed the individual-level survey data. The spatial patterns in the winter (Figure 2A) and monsoon (Figure 2B) incidences in these survey data are consistent with the pattern for all reported cases (Supplementary Figure 3), indicating that the subset data are representative of the overall incidence data. When we model rotavirus seasonality as a function of demographic, socioeconomic, and sanitation factors at the individual level, we find a statistically significant association between reported tube well use and the odds of a case occurring during the monsoon season versus the rest of the year (Figure 2C).
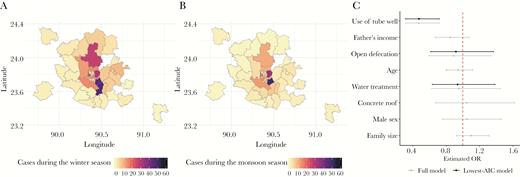
A, B, Spatial distribution of cases in the individual-level survey data that occurred during the winter (A) and monsoon (B) seasons. C, Estimated fixed effects (and 95% confidence interval) for the full model (gray) and for the model with the lowest Akaike information criterion (AIC) (black). The estimated fixed effects represent the estimated association between each of the independent variables and the odds of a case occurring during the monsoons, holding all else fixed (including random effects). The red dashed line indicates an odds ratio (OR) of 1. Map showing residence locations, within and outside Dhaka metropolitan area, for rotavirus patients at the Dhaka Hospital.
Specifically, we find that in the selected model (lowest Akaike information criterion), individuals who obtained their drinking water primarily from a tube well, rather than from a tap, pond, or other sources, had decreased odds of infection during the monsoons. The odds were 0.47 times lower (95% confidence interval, .31–.71), holding all else fixed. This change corresponds to a 53% decrease in the odds of experiencing a monsoon case for those reporting tube well use compared with those relying on other sources for their drinking water. Although a majority of the cases occurred in children <1 year old (Supplementary Table 2), only a low proportion (2%) of these children were exclusively breastfed (Supplementary Table 4), suggesting that the majority of individuals with rotavirus consumed drinking water.
DISCUSSION
We show that drinking water from tube wells, which are less likely to be contaminated during flooding events, is protective against rotavirus during the monsoon season. Although rotavirus transmission is typically considered to occur via direct person-to-person contact, this result highlights the importance of environmental transmission via water in Dhaka. Our findings, in combination with the low duration of exclusive breastfeeding reported in Bangladesh [10], suggest that contaminated water is likely to be an important driver of rotavirus transmission among children. These results are consistent with those of previous studies showing that waterborne transmission alone is sufficient to spread rotavirus between hydrologically connected locations [6] and that monsoon flooding modulates its transmission [7].
The use of tube wells has also been shown to provide a protective effect against other diarrheal diseases in Bangladesh, such as cholera [11, 12] and shigellosis [12], especially in areas that are not protected from flooding [13]. Although we do not have data on tube well depth for this study, a previous study from rural Bangladesh showed that deep tube wells may reduce disease burden by accessing deep aquifers [14], which are less likely than other water supply systems to have fecal contamination during flooding events. The consequences of a possible environmental reservoir are unclear, especially in Bangladesh, where recent shifts in monsoon rainfall have been observed across different regions [15]. An increase in heavy precipitation has the potential to trigger flooding events, and in so doing, to increase the incidence of rotavirus and other waterborne diarrheal diseases.
There are several limitations that should be noted. Our analyses compared individuals with confirmed rotavirus infection at different times of the year. Because there were no control group without the disease, we were unable to test whether tube well use is protective against rotavirus in general. We also do not provide a mechanistic explanation for the spatial gradient observed in rotavirus seasonality at the aggregate level, or for the differences observed between winter and monsoon incidence. Thus, we cannot rule out potential unobserved confounders that could also explain the seasonal pattern described here. More detailed spatiotemporal data, with a well-defined control group, is needed to address some of these limitations.
In conclusion, our findings support the hypothesis that consumption of clean water plays an important role in protecting against rotavirus infection, particularly during the monsoon season, when flooding can contaminate surface water. The potential transmission of rotavirus through water should be recognized when planning control interventions beyond just vaccination. This is especially important in highly populated regions of low-income countries where rotavirus is highly endemic, and where transmission may be modulated seasonally by the existence of environmental reservoirs.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank the donors to the International Centre for Diarrheal Disease Research, Bangladesh (ICDDR,B) for their support and commitment to the ICDDR,B’s research efforts.
Financial support. This work was supported by the ICDDR,B and its donors, which provide unrestricted support for the ICDDR,B’s operation and research; current donors include the Government of the People’s Republic of Bangladesh; the Department of Foreign Affairs, Trade, and Development Canada; the Swedish International Development Cooperation Agency; and the Department for International Development (UK Aid). The work was also supported by the National Institutes of Health (grants U54 GM088558-10 to P. P. M. and R35 GM124715-02 to C. O. B.) and The Rockefeller Foundation (Planetary Health Fellowship to A. S. M.).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Author notes
P. P. M. and A. S. M. contributed equally to this work.




