-
PDF
- Split View
-
Views
-
Cite
Cite
Rustem Makhmutov, Gabriele Meyer, Moriah E Ellen, Steffen Fleischer, Avoidable Care Transitions: A Consensus-Based Definition Using a Delphi Technique, Innovation in Aging, Volume 7, Issue 8, 2023, igad106, https://doi.org/10.1093/geroni/igad106
Close - Share Icon Share
Abstract
Older adults are at increased risk of frequent transitions between care settings, even though some care transitions are avoidable. The term “avoidable care transitions” is not clearly defined in the research literature. This study aimed to find a consensus-based definition for “avoidable care transitions.”
This study was conducted as part of the TRANS-SENIOR research network. A 4-round Delphi survey was based on a literature review that identified existing definitions of “avoidable care transitions.” Articles in MEDLINE via PubMed and CINAHL were searched. In total 95 references were included, and 106 definitions were identified. Definitions were coded to find themes, resulting in 3 themes with 2 codes for each.
In total, 99 experts from 9 countries were invited, and the response rates in Delphi Rounds 1, 2, 3, and 4 were 37.5%, 19.1%, 33.3%, and 23.3%, respectively. Upon reaching the predefined minimum of 90% agreement, the following definition was declared as final: “Avoidable care transitions (a) are without significant patient-relevant benefits or with a risk of harm outweighing patient-relevant benefits and/or (b) are when a comparable health outcome could be achieved in lower resource settings using the resources available in that place/health care system, and/or (c) violate a patient’s/informal caregiver’s preference or an agreed care plan.”
Consensus on a definition for “avoidable care transitions” was reached by a multidisciplinary and international panel of experts comprising researchers and providers. The resulting definition consists of 3 distinct dimensions relating to the balance of benefit and harm to a patient, resource consumption, and a patient’s or informal caregiver’s preferences. The new definition might enhance the common understanding of avoidable care transitions and is now ready for application in research and quality and safety management in health care.
Translational Significance: The concept of “avoidable care transitions” is mainly interpreted from a single perspective: the health care system’s or clinician’s perspective. Nevertheless, no consensus on defining avoidable care transitions has been reached. A systematically developed definition seemed necessary. The resulting consensus-based definition embraces multiple dimensions and addresses the shortcomings of the former definitions. It can guide patients, clinicians, and policymakers in decision-making and lay the groundwork for practical solutions aimed at identifying and reducing avoidable care transitions, thus resulting in positive implications at the clinical, system, and patient levels. The new definition may also improve comparability among future studies.
Background and Objectives
Older adults are at an increased risk of frequent transitions between care settings. These transitions are often associated with negative outcomes for the person concerned, such as a decline in autonomy, reduced quality of life, more adverse medical events, and even increased mortality, as well as for the health care system with increased direct and opportunity costs (Naylor & Keating, 2008; Storm et al., 2014).
Care transitions have been defined as changes in the setting of care provision (Morrison et al., 2016), encompassing care settings such as hospitals, nursing homes (NH), primary care, home care, and palliative care. Hence, a care transition is an umbrella term that embraces different types of transitions, such as readmission and discharge. Moreover, care transitions occur not only between care settings but also within care settings (World Health Organization, 2016), for instance, between wards and medical departments in the same hospital.
Some of these care transitions are avoidable, and the phenomenon of avoidable transitions has received greater attention within the last two decades, resulting in more research due to the striking numbers of avoidable care transitions and due to the increased burden on patients and health systems (Enderlin et al., 2013; Gruneir, 2013; Hall et al., 2020; Lemoyne et al., 2019; Theresa Dreyer, 2014; Thwaites et al., 2017; van der Does et al., 2020; Yam, Wong, Chan, Leung, et al., 2010; Yam, Wong, Chan, Wong, et al., 2010). Thus, certain types of avoidable transitions are used as outcomes in research, such as re-hospitalization within 30 days of discharge, which is a widely accepted indicator of quality of care (Blume et al., 2021). Ambulatory care-sensitive conditions (ACSCs) are used as quality indicators in the primary care setting by the Organization for Economic Cooperation and Development (OECD), representing a subtype of avoidable hospital admissions attributed to specific chronic diseases (OECD, 2021). Although ACSCs cover more than 30 conditions for which hospitalization is deemed avoidable, there is no single, universal list of ACSCs that is internationally established and used (Purdy et al., 2009). Five core conditions (i.e., diabetes, hypertension, congestive heart failure, chronic obstructive pulmonary disease, and asthma) are considered important in European countries and show substantial variation between European countries (OECD & European Union, 2018, 2022). These five ACSCs accounted for over 4.6 million hospital admissions across the European Union (EU) in 2015, representing 37 million bed days and amounting to 5.6% of all admissions that might have been avoided (OECD & European Union, 2018).
Overall, hospital readmission rates vary widely across studies depending on the methodology and investigated population, ranging from 5% to 80% (van der Does et al., 2020; Yam, Wong, Chan, Wong, et al., 2010). The variability between studies regarding the magnitude of avoidable transitions can be explained to a certain extent by varying disease prevalence and availability of hospital care or institutional care or different assessment methods (e.g., chart review by one clinician, multidisciplinary meetings, or patient interviews) among studies and countries (Soong & Bell, 2015; van der Does et al., 2020; Yam, Wong, Chan, Wong, et al., 2010).
It is important to note that avoidable re-hospitalizations represent only a part of all avoidable care transitions. For example, avoidable hospital admissions occur among people living at home or in NHs (Afonso-Argilés et al., 2020).
Scanning the literature on the topic, it becomes obvious that the concept of “avoidable care transitions” and related terms are interpreted and used differently throughout all publications, and no consensus on a definition has been reached thus far (Gruneir, 2013; Lemoyne et al., 2019; Morphet et al., 2015; Nolte et al., 2012; Vossius et al., 2013). Some studies interpret the term “potentially avoidable” from a system and/or clinician perspective, and other studies assess “avoidability” from a patient perspective (Thwaites et al., 2017; Yam, Wong, Chan, Leung, et al., 2010). For example, patient factors may include socioeconomic status, health status, and a person’s behaviors, such as noncompliance with treatment or failure of a person to seek prompt medical attention when symptoms recur (Yam, Wong, Chan, Leung, et al., 2010). Clinical factors refer to the appropriateness of assessment and treatment, for instance, the adequacy of clinical management and stabilization prior to discharge or outpatient care after discharge (Yam, Wong, Chan, Leung, et al., 2010). System factors normally relate to the availability, accessibility, and coordination of care across the health care system, such as the provision of resources at home that meet a person’s needs (Yam, Wong, Chan, Leung, et al., 2010). These factors are also reflected in two very recent studies, confirming that these factors are still relevant and important today. For example, Kasdorf et al. (2021) identified four factors for potentially avoidable transitions: the health care system, organization, health care professionals, and patients and relatives. These four factors could be grouped into more general, overarching factors, such as system-, clinician-, and patient-related factors, as described earlier. Another study by Schippel et al. (2022) identified three risk factors for burdensome transitions, namely, transparent communication in the face of an incurable disease, coordination of care, and consideration of patient preferences. These three factors, as in the previous example, could also be grouped into overarching clinician-, system-, and patient-related factors.
A comprehensive consensus-based definition for “avoidable care transitions” seems timely, and the potential for forestalling avoidable transitions appears to be expansive. It is important to involve researchers and providers when addressing the avoidability of care transitions. A clear definition might foster a mutual understanding among different stakeholders and patients to support decision-making and care planning.
The aim of this study was to deliver a new research-informed, consensus-based definition for “avoidable care transitions.”
Research Design and Methods
This study comprised two consecutive parts: (a) a preparatory literature review as the basis for (b) a Delphi survey.
Literature Review in Preparation for the Delphi Survey
The objective of the literature review was to identify definitions of interest, that is, existing definitions of “avoidable care transitions” and its related terms that were used interchangeably or described the same issue.
Search strategy
A literature search in the MEDLINE via PubMed and CINAHL electronic databases was conducted in two steps between February and April 2020. The first search step was sensitive and yielded a broad range of results, while the second search step was more specific and provided fewer but better-matching results. The two search steps were independent. Part of the results from the first search and all of the results from the second search were reviewed. The searches included the words avoidable, transition, and health care, and their related terms. We did not include specific search terms for the population or care settings because the aim was to gain a broad understanding of avoidable care transitions. A summary of the search terms is shown in Table 1. The reference lists of the included publications were screened for further eligible publications that included additional definitions. The literature review aimed to achieve data saturation by retrieving a complete representation of definitions of interest, rather than having a complete representation of the literature by retrieving every single definition from every single publication that exists. Screening and data extraction were performed simultaneously, and the stage when further retrieved definitions did not add new information to core ideas discovered in the already retrieved definitions was defined as data saturation. Two researchers independently conducted the full-text screening (R.M. and C.M.J.). Any conflicts were resolved by a third reviewer.
| Order . | Terms . |
|---|---|
| First search | avoidable, inappropriate, burdensome, unfavorable, undesirable, preventable, inadequate, transit*, transfer*, discharge, shift, handover, hospitals*, re-admission*, handoff, health*, nurs*, medic*, hospital*, care. |
| Second search | avoid*, inappropriate, burden*, unfavour*, undesir*, prevent*, inadequate, transit*, transfer*, discharge*, admission*, readmission*, visit*, stay*, re-hospitali*. |
| Order . | Terms . |
|---|---|
| First search | avoidable, inappropriate, burdensome, unfavorable, undesirable, preventable, inadequate, transit*, transfer*, discharge, shift, handover, hospitals*, re-admission*, handoff, health*, nurs*, medic*, hospital*, care. |
| Second search | avoid*, inappropriate, burden*, unfavour*, undesir*, prevent*, inadequate, transit*, transfer*, discharge*, admission*, readmission*, visit*, stay*, re-hospitali*. |
Note: “*” indicates that a search term may have various endings after an asterisk. For example, “avoid*” can be “avoid,” “avoidable,” “avoidability,” and so on.
| Order . | Terms . |
|---|---|
| First search | avoidable, inappropriate, burdensome, unfavorable, undesirable, preventable, inadequate, transit*, transfer*, discharge, shift, handover, hospitals*, re-admission*, handoff, health*, nurs*, medic*, hospital*, care. |
| Second search | avoid*, inappropriate, burden*, unfavour*, undesir*, prevent*, inadequate, transit*, transfer*, discharge*, admission*, readmission*, visit*, stay*, re-hospitali*. |
| Order . | Terms . |
|---|---|
| First search | avoidable, inappropriate, burdensome, unfavorable, undesirable, preventable, inadequate, transit*, transfer*, discharge, shift, handover, hospitals*, re-admission*, handoff, health*, nurs*, medic*, hospital*, care. |
| Second search | avoid*, inappropriate, burden*, unfavour*, undesir*, prevent*, inadequate, transit*, transfer*, discharge*, admission*, readmission*, visit*, stay*, re-hospitali*. |
Note: “*” indicates that a search term may have various endings after an asterisk. For example, “avoid*” can be “avoid,” “avoidable,” “avoidability,” and so on.
Inclusion criteria
English-language references published from January 2005 onwards were considered for inclusion. The literature review by Kralik et al. (2006) explored how the term “transition” has been used in the health care literature; they searched for papers published between 1994 and 2004. The authors of the review noted that the concept of transition had undergone altered understandings in the social science and health disciplines over time, with nurses contributing to more recent understandings of the transition process (Kralik et al., 2006). Taking into account this literature review and the notion that a concept evolves over time, we decided to search for articles published after 2004 (i.e., from January 2005) to find the most relevant definitions of interest, and at the same time, this time frame allowed for some variation in the definitions that we believe only enriched our search results.
A study was deemed eligible if it presented a complete or partial definition of the subject of “avoidable care transitions” and related terms. Complete definitions were included that consisted of definiendum and definiens, where a definiendum was an “avoidable care transition” or related/synonym terms, and definiens were characteristics of such terms. Partial definitions comprised of definiens were also included (i.e., descriptions or explanations of a term that could be implicitly inferred as definiens for a definiendum).
Synthesis
Retrieved definitions were inductively coded to identify themes. The coding was conducted by two researchers (R.M. and S.F.), and the codes were further reviewed, commented on, and adjusted several times until the research team members (R.M., S.F., G.M., and M.E.) reached a full consensus.
Delphi Survey
The Delphi survey is a method designed to gather the most reliable consensus from a group of experts. This is achieved by a series of structured questionnaires or so-called rounds, coupled with controlled opinion feedback (Dalkey & Helmer, 1963). Researchers employ the method to translate scientific knowledge and professional experience into informed judgment and to support decision-making (Akins et al., 2005). This approach enables feedback from a greater number of experts than could feasibly be included in a group or committee meeting and from participants who are geographically widespread. The following four fundamental principles are considered important for defining a procedure as a “Delphi”: anonymity, iteration, controlled feedback, and statistical aggregation of group responses (Rowe & Wright, 1999). The Delphi method is used to make the best use of available information but not to create new knowledge (Bleijlevens et al., 2016).
Participants
This study is part of the TRANS-SENIOR network, an EU-funded project with an overall focus on transitional care innovation for older adults. TRANS-SENIOR includes 11 early-stage researchers, seven partner organizations including the World Health Organization, and beneficiaries in six countries: Germany, the Netherlands, Belgium, Switzerland, Poland, and Israel.
Candidates for the Delphi survey had to be fluent in English and affiliated with the health care system (i.e., a member of a health care profession, working in a health care sector, research in health care, etc.). Selected members within the TRANS-SENIOR Consortium, among other individually chosen participants identified via the research team’s professional networks, were invited to participate in the Delphi survey. TRANS-SENIOR members represented a good sampling pool for the Delphi survey because they are experts in the field of transitional care among older adults. The TRANS-SENIOR Consortium was also encouraged to invite other colleagues in their network. This ensured the richness of information gathered from the experts because they were located in different countries, namely, Germany, the Netherlands, Belgium, Switzerland, Poland, Israel, Iraq, Spain, and Austria.
According to former studies that recruited from 10 to 100 experts (Akins et al., 2005; Armstrong et al., 2005; Bleijlevens et al., 2016; De Vet et al., 2005; Howell & Kemp, 2005; Nekolaichuk et al., 2005; Stolee et al., 2005), we aimed for approximately 20–50 experts in our sample as a good and feasible compromise, because too few experts may be insufficient for data saturation and involving more than 100 participants could make data analysis too resource-consuming.
Delphi strategy
The Delphi questionnaire was pilot-tested with three individual representatives of the target group and was further adapted before commencing with the first round of the official Delphi survey.
The Delphi survey was conducted between November 2020 and July 2021. The internet-based survey tool Qualtrics was used as a platform. In each round, the participants received an invitation email with a brief study summary and a link asking them to participate in the online survey. They were asked to forward the invitation email to other relevant experts. The invited individuals were also asked to complete the survey in approximately 2 weeks; a reminder email was sent to the whole sample. An invitation email was sent to all identified experts over all rounds (i.e., invitations to participate were not limited only to those who completed earlier rounds).
Codes that were synthesized during the literature review formed the base for the first round of the Delphi survey. The participants were provided with these codes and with corresponding examples to further illustrate the codes. They were asked to rank the importance of the proposed codes from 0 to 10, in which 0 was “not at all important” and 10 was “extremely important,” and to provide professional opinions. Four preliminary definitions were developed by two researchers (R.M. and S.F.) based on the codes and participants’ feedback from Round 1. We developed four preliminary definitions with different formulations and tried to keep all key meanings/ideas that emerged from the codes and feedback in each definition. This allowed some variation among four preliminary definitions while still preserving common key meanings/ideas. Four preliminary definitions were further reviewed, commented on, and adjusted several times until the research team members reached a full consensus. In Round 2, the participants were provided with four preliminary definitions and were asked to provide their professional opinions and rank the definitions in order of preference. In Round 3, the participants were asked whether the proposed definition was final and if the answer was “no,” to provide their professional opinions on how to further improve the proposed definition. Round 3 could be iteratively repeated until an agreement of at least 90% was reached.
Delphi round analysis
The research team calculated a statistical aggregation of the group responses and performed a qualitative analysis on open-formulated text data gathered from the Delphi survey rounds. During the qualitative analysis, the proposed definitions were altered by reformulating or incorporating or removing some elements from the definitions according to the experts’ feedback. Upon completion of each round, a summary of the findings from the previous round was sent to the pool of identified experts. Following a study protocol (not published), the predefined agreement rate in the group of participants concerning a proposed definition was set at a minimum of 90%, which corresponds to that in a comparable study by Bleijlevens et al. (2016). Upon fulfillment of this requirement, the proposed definition was claimed as final, meaning that a consensus regarding the definition had been reached. Following the completion of the Delphi survey, the final definition was communicated to all the experts.
Results
The literature review revealed more than 100 definitions, and consecutive synthesis yielded six codes in total. During the survey, 96 experts were invited to the first round and 99 to the following rounds, and the response rates in Delphi rounds 1, 2, 3, and 4 were 37.5%, 19.1%, 33.3%, and 23.3%, respectively. At the time of the survey, experts were located in nine countries, and the majority of them were employed as researchers with vast clinical experience; some held clinical positions such as general practitioner, physician, geriatrician, or nurse. Experts were from various backgrounds, including public health, primary care, medicine, nursing science, epidemiology, health science, emergency medicine, geriatrics, health services research, and health economics. Four Delphi survey rounds were conducted, and consensus was reached on a new definition for “avoidable care transitions” with a 91% agreement rate. A flowchart of the study procedures and participant selection process is shown in Figure 1.
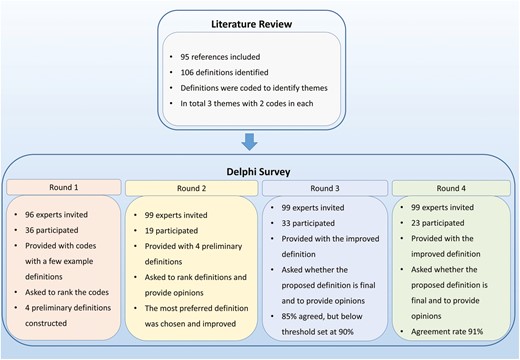
Flowchart of the study procedures and participant selection process.
Literature Review
As a result of the review, 95 references were included, and 106 definitions were identified. A list of the 95 included references is provided in the Appendix. The key messages described in the identified definitions led to a total of six codes. Each code was assigned a short description and grouped into one of the themes, resulting in three themes with two codes for each. A summary of the themes and codes is shown in Table 2.
Summary of Themes and Codes from 95 References on Avoidable Care Transitions
| Theme . | Code . | Description . |
|---|---|---|
| 1. Identification by frequency, shift of responsibility, and low extent of measures/ interventions | Code 1. Short-term, highly frequent transitions and back and forth “ping-pong” (repeating between place A and place B), which can be related to responsibility aversion and finding the right place of care. | Frequent transitions between care settings with a short length of stay in between, with a likelihood of little benefit. Mainly back and forth from the same settings or institutions with the intention to avoid taking responsibility or due to being unable to find an appropriate place of care. |
| Code 2. Short-term, highly frequent transitions (i.e., chain-like, when a care setting is an intermediate/temporary step with inadequate care in the overall transfer process that could have been avoided, like from place A to place B, to place C, and so on). | Frequent transitions between care settings with a short length of stay in between, with the likelihood of little benefit. One setting after the other with inadequate care taking place in single settings between the origin and destination, with the intention to transfer responsibility or due to being unable to find the proper place of care. | |
| 2. Benefit–harm balance | Code 3. Absence of benefit (MCID: minimal clinically important difference) | Transitions where there are neither beneficial nor harmful effects. |
| Code 4. Presence of harm. | Transitions with associated harm OR harm that outweighs the positive effects (note: often associated with end-of-life care OR terminal illness). | |
| 3. Existing alternatives with equivalent or even better outcomes and lower resource utilization | Code 5. Current opportunities. | Transition where the same/similar outcome can be reached in an alternative setting with possible lower resource utilization. |
| Code 6. Foregone opportunities. | Inappropriate use of resources in the past may lead to avoidable transitions in the present or could include diagnosis/therapy-related errors; management-related errors; and quality of provided services. |
| Theme . | Code . | Description . |
|---|---|---|
| 1. Identification by frequency, shift of responsibility, and low extent of measures/ interventions | Code 1. Short-term, highly frequent transitions and back and forth “ping-pong” (repeating between place A and place B), which can be related to responsibility aversion and finding the right place of care. | Frequent transitions between care settings with a short length of stay in between, with a likelihood of little benefit. Mainly back and forth from the same settings or institutions with the intention to avoid taking responsibility or due to being unable to find an appropriate place of care. |
| Code 2. Short-term, highly frequent transitions (i.e., chain-like, when a care setting is an intermediate/temporary step with inadequate care in the overall transfer process that could have been avoided, like from place A to place B, to place C, and so on). | Frequent transitions between care settings with a short length of stay in between, with the likelihood of little benefit. One setting after the other with inadequate care taking place in single settings between the origin and destination, with the intention to transfer responsibility or due to being unable to find the proper place of care. | |
| 2. Benefit–harm balance | Code 3. Absence of benefit (MCID: minimal clinically important difference) | Transitions where there are neither beneficial nor harmful effects. |
| Code 4. Presence of harm. | Transitions with associated harm OR harm that outweighs the positive effects (note: often associated with end-of-life care OR terminal illness). | |
| 3. Existing alternatives with equivalent or even better outcomes and lower resource utilization | Code 5. Current opportunities. | Transition where the same/similar outcome can be reached in an alternative setting with possible lower resource utilization. |
| Code 6. Foregone opportunities. | Inappropriate use of resources in the past may lead to avoidable transitions in the present or could include diagnosis/therapy-related errors; management-related errors; and quality of provided services. |
Summary of Themes and Codes from 95 References on Avoidable Care Transitions
| Theme . | Code . | Description . |
|---|---|---|
| 1. Identification by frequency, shift of responsibility, and low extent of measures/ interventions | Code 1. Short-term, highly frequent transitions and back and forth “ping-pong” (repeating between place A and place B), which can be related to responsibility aversion and finding the right place of care. | Frequent transitions between care settings with a short length of stay in between, with a likelihood of little benefit. Mainly back and forth from the same settings or institutions with the intention to avoid taking responsibility or due to being unable to find an appropriate place of care. |
| Code 2. Short-term, highly frequent transitions (i.e., chain-like, when a care setting is an intermediate/temporary step with inadequate care in the overall transfer process that could have been avoided, like from place A to place B, to place C, and so on). | Frequent transitions between care settings with a short length of stay in between, with the likelihood of little benefit. One setting after the other with inadequate care taking place in single settings between the origin and destination, with the intention to transfer responsibility or due to being unable to find the proper place of care. | |
| 2. Benefit–harm balance | Code 3. Absence of benefit (MCID: minimal clinically important difference) | Transitions where there are neither beneficial nor harmful effects. |
| Code 4. Presence of harm. | Transitions with associated harm OR harm that outweighs the positive effects (note: often associated with end-of-life care OR terminal illness). | |
| 3. Existing alternatives with equivalent or even better outcomes and lower resource utilization | Code 5. Current opportunities. | Transition where the same/similar outcome can be reached in an alternative setting with possible lower resource utilization. |
| Code 6. Foregone opportunities. | Inappropriate use of resources in the past may lead to avoidable transitions in the present or could include diagnosis/therapy-related errors; management-related errors; and quality of provided services. |
| Theme . | Code . | Description . |
|---|---|---|
| 1. Identification by frequency, shift of responsibility, and low extent of measures/ interventions | Code 1. Short-term, highly frequent transitions and back and forth “ping-pong” (repeating between place A and place B), which can be related to responsibility aversion and finding the right place of care. | Frequent transitions between care settings with a short length of stay in between, with a likelihood of little benefit. Mainly back and forth from the same settings or institutions with the intention to avoid taking responsibility or due to being unable to find an appropriate place of care. |
| Code 2. Short-term, highly frequent transitions (i.e., chain-like, when a care setting is an intermediate/temporary step with inadequate care in the overall transfer process that could have been avoided, like from place A to place B, to place C, and so on). | Frequent transitions between care settings with a short length of stay in between, with the likelihood of little benefit. One setting after the other with inadequate care taking place in single settings between the origin and destination, with the intention to transfer responsibility or due to being unable to find the proper place of care. | |
| 2. Benefit–harm balance | Code 3. Absence of benefit (MCID: minimal clinically important difference) | Transitions where there are neither beneficial nor harmful effects. |
| Code 4. Presence of harm. | Transitions with associated harm OR harm that outweighs the positive effects (note: often associated with end-of-life care OR terminal illness). | |
| 3. Existing alternatives with equivalent or even better outcomes and lower resource utilization | Code 5. Current opportunities. | Transition where the same/similar outcome can be reached in an alternative setting with possible lower resource utilization. |
| Code 6. Foregone opportunities. | Inappropriate use of resources in the past may lead to avoidable transitions in the present or could include diagnosis/therapy-related errors; management-related errors; and quality of provided services. |
Delphi Survey
Round 1
In total, 96 experts were identified and were sent an invitation email to participate in Round 1 of the Delphi survey. The invited experts were located in nine countries: Germany (n = 66), Poland (n = 3), Belgium (n = 9), the Netherlands (n = 7), Switzerland (n = 6), Israel (n = 2), Spain (n = 1), Iraq (n = 1), and Austria (n = 1). A total of 36 experts participated in the survey (37.5% response rate). On a scale from 0 to 10, each code was rated 5 or above by more than 83% of the experts, implying that all the codes were relevant and important. The vast majority of the participants agreed that the proposed six codes were comprehensive. The experts also suggested taking a patient’s and his or her caregiver’s preferences into account. Finally, four preliminary definitions were constructed using the codes and the experts’ suggestions (Table 3).
Preliminary Definitions Generated from Round 1 Delphi Survey and Submitted for Round 2 Feedback
| Version . | Definitions . |
|---|---|
| 1 | Avoidable care transitions (1) are short-term and frequent between care settings or (2) are without significant benefit to a patient’s quality of life or (3) imply a risk of harm outweighing the benefit to a patient’s quality of life or (4) indicate that the same health outcome is feasible in lower resource settings or (5) are caused by inadequate diagnosis/therapy/health care management or (6) violate a patient’s preference. |
| 2 | Avoidable care transitions are transitions (1) where no proper place of care could be found, indicated by frequent changes in care settings or (2) caused by inadequate diagnosis/therapy/health care management or (3) where the same health outcome is feasible in lower resource settings or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where a patient’s preference is violated. |
| 3 | Avoidable care transitions are transitions (1) that are short-term and frequent between care settings or (2) where responsibility is not properly taken or (3) where no proper place of care could be found or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management or (7) where a patient’s preference is violated. |
| 4 | Avoidable care transitions are transitions (1) that are burdensome or (2) that happen in the end-of-life stage of a patient or (3) where a patient’s preference is violated or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management. |
| Version . | Definitions . |
|---|---|
| 1 | Avoidable care transitions (1) are short-term and frequent between care settings or (2) are without significant benefit to a patient’s quality of life or (3) imply a risk of harm outweighing the benefit to a patient’s quality of life or (4) indicate that the same health outcome is feasible in lower resource settings or (5) are caused by inadequate diagnosis/therapy/health care management or (6) violate a patient’s preference. |
| 2 | Avoidable care transitions are transitions (1) where no proper place of care could be found, indicated by frequent changes in care settings or (2) caused by inadequate diagnosis/therapy/health care management or (3) where the same health outcome is feasible in lower resource settings or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where a patient’s preference is violated. |
| 3 | Avoidable care transitions are transitions (1) that are short-term and frequent between care settings or (2) where responsibility is not properly taken or (3) where no proper place of care could be found or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management or (7) where a patient’s preference is violated. |
| 4 | Avoidable care transitions are transitions (1) that are burdensome or (2) that happen in the end-of-life stage of a patient or (3) where a patient’s preference is violated or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management. |
Preliminary Definitions Generated from Round 1 Delphi Survey and Submitted for Round 2 Feedback
| Version . | Definitions . |
|---|---|
| 1 | Avoidable care transitions (1) are short-term and frequent between care settings or (2) are without significant benefit to a patient’s quality of life or (3) imply a risk of harm outweighing the benefit to a patient’s quality of life or (4) indicate that the same health outcome is feasible in lower resource settings or (5) are caused by inadequate diagnosis/therapy/health care management or (6) violate a patient’s preference. |
| 2 | Avoidable care transitions are transitions (1) where no proper place of care could be found, indicated by frequent changes in care settings or (2) caused by inadequate diagnosis/therapy/health care management or (3) where the same health outcome is feasible in lower resource settings or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where a patient’s preference is violated. |
| 3 | Avoidable care transitions are transitions (1) that are short-term and frequent between care settings or (2) where responsibility is not properly taken or (3) where no proper place of care could be found or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management or (7) where a patient’s preference is violated. |
| 4 | Avoidable care transitions are transitions (1) that are burdensome or (2) that happen in the end-of-life stage of a patient or (3) where a patient’s preference is violated or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management. |
| Version . | Definitions . |
|---|---|
| 1 | Avoidable care transitions (1) are short-term and frequent between care settings or (2) are without significant benefit to a patient’s quality of life or (3) imply a risk of harm outweighing the benefit to a patient’s quality of life or (4) indicate that the same health outcome is feasible in lower resource settings or (5) are caused by inadequate diagnosis/therapy/health care management or (6) violate a patient’s preference. |
| 2 | Avoidable care transitions are transitions (1) where no proper place of care could be found, indicated by frequent changes in care settings or (2) caused by inadequate diagnosis/therapy/health care management or (3) where the same health outcome is feasible in lower resource settings or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where a patient’s preference is violated. |
| 3 | Avoidable care transitions are transitions (1) that are short-term and frequent between care settings or (2) where responsibility is not properly taken or (3) where no proper place of care could be found or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management or (7) where a patient’s preference is violated. |
| 4 | Avoidable care transitions are transitions (1) that are burdensome or (2) that happen in the end-of-life stage of a patient or (3) where a patient’s preference is violated or (4) without potential significant benefit or with a high risk of harm to a patient’s quality of life or (5) where the same health outcome is feasible in lower resource settings or (6) caused by inadequate diagnosis/therapy/health care management. |
Round 2
Three additional experts from Israel joined the expert panel: one with a background in geriatric and internal medicine, one with a background in geriatric medicine, and another with a background in public health. In total, 99 experts were sent an invitation email to complete Round 2, 19 of whom participated in the survey (19.1% response rate). As a result of this round, the most preferred definition was chosen and modified according to the experts’ feedback. The most preferred definition and its modified version are shown in Figure 2. The definition was adjusted by removing two elements from it and reformulating some parts. The first element was removed, as some experts suggested that avoidable care transitions are not always short-term and not necessarily frequent. Another element, “inadequate diagnosis/therapy/health care management,” was also removed, as it was believed to be too broad and very difficult to determine. It was also suggested to incorporate an aspect such as “violation of established care plan.” Finally, the modified definition was proposed to the experts in Round 3.
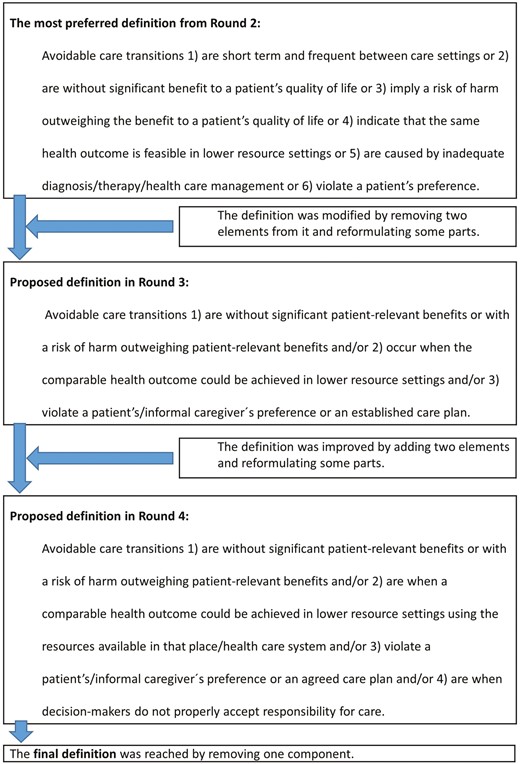
Flow diagram shows how the preferred definition from Round 2 was modified in subsequent rounds to reach its final version.
Round 3
Ninety-nine participants were invited to participate in Round 3, 33 of whom participated in the survey (33.3% response rate). In this round, almost 85% of the expert panel agreed with the proposed definition. However, the agreement rate was below the set threshold of 90%. The definition was further adjusted in accordance with the feedback. The proposed definition and its adjusted version are shown in Figure 2. Six commentaries were provided on how to improve the proposed definition. The majority of the commentaries were accounted for and incorporated into the proposed definition. However, some commentaries were not accounted for in the proposed definition because our research team considered them to be very detailed and specific. The rationale behind this is that incorporating very detailed and specific aspects would considerably extend the definition, thus making it impractical or inconvenient to use. The definition was improved by adding two elements and reformulating some parts. The first element related to the “usage of resources available in a particular place or health care system.” The second added element related to when “nobody accepts responsibility for care.” Finally, the adjusted definition was proposed in Round 4.
Round 4
The 99 participants were invited to participate in Round 4, 23 of whom participated in the survey (23.2% response rate). The experts’ commentaries were accounted for, and the following component was removed from the proposed definition: “when decision-makers do not properly accept the responsibility for care.” In the end, 21 out of 23 individuals agreed with the definition, thus resulting in an agreement rate of 91%.
The following definition was considered final: “Avoidable care transitions (1) are without significant patient-relevant benefits or with a risk of harm outweighing patient-relevant benefits and/or (2) are when a comparable health outcome could be achieved in lower resource settings using the resources available in that place/health care system and/or (3) violate a patient’s/informal caregiver’s preference or an agreed care plan.”
Discussion
Consensus on the definition of “avoidable care transitions” was successfully reached after four Delphi survey rounds by a multidisciplinary and international panel of experts comprising researchers and providers. The new systematically developed definition addresses several limitations that were inherent in former definitions.
The resulting definition consists of three distinct dimensions relating to the balance of benefit and harm to a patient, resource consumption, and a patient’s or informal caregiver’s preferences. Former definitions were narrowly defined and touched mainly upon a single perspective. For example, Ouslander et al. (2009) referred to the benefit and risk of harm to a patient in the case of hospitalization among NH residents, where such transitions may be “… inappropriate, because the transfer exposes NH [nursing home] residents to additional risks associated with hospitalization, without substantial potential benefit for the residents’ clinical and functional status or quality of life.” Another example shows the perspective of resource consumption: “… inappropriate transfers represent situations in which care in a lower-cost setting (i.e., the NH) would be as safe as and less disruptive than care in a higher-cost hospital setting” (Lemoyne et al., 2019). The third element that related to the violation of preferences and of an agreed care plan was incorporated into the consensus-based definition following the experts’ feedback during the Delphi survey. The definition developed in this study was based on former definitions and experts’ opinions and was approved by the international group of experts during the Delphi process. The development process of the definition involved incorporating, removing, and reformulating some elements. In particular, as a result of Delphi Round 1, four preliminary definitions were constructed using the codes and by additionally incorporating one element on a “patient” factor, as was suggested by the experts. As a result of Round 2, the most preferred definition was modified by (a) removing two elements on “short-term and frequent transitions” and “inadequate health care management,” (b) incorporating an element on “violation of the established care plan,” and (c) reformulating some elements. As a result of the subsequent rounds, the final definition was achieved by incorporating the element of “resource usage in a particular place or health care system,” followed by reformulation of some elements. The new definition is more saturated and embraces multiple perspectives, thus overcoming the shortcomings of former definitions identified through the literature review. This was a necessary and important step to facilitate the understanding of “avoidable care transitions.”
The new definition was developed using well-established methodological approaches based (a) on the relevant scientific literature acquired via a systematic literature search process and (b) on a reliable consensus of opinion from a group of experts by using a Delphi technique. This combination of methodological approaches has also been implemented in a number of studies in various research disciplines (Bleijlevens et al., 2016; Guseva Canu et al., 2021; Vakil et al., 2006; van der Horst et al., 2017). Other studies employed only the Delphi survey (Adams et al., 2021; Dribin et al., 2020; van den Steene et al., 2019; Zanker et al., 2019). The present study was as complex as these examples and aimed to develop new definitions for various topics, such as physical restraints, multiple, and complex needs among children, anaphylaxis outcomes, sarcopenia, hyperacusis, occupational burnout, and gastroesophageal reflux disease. Former studies dealing with other topics have substantially contributed to the harmonization of their corresponding fields of study and were well-received and frequently cited (Bleijlevens et al., 2016; Guseva Canu et al., 2021; Vakil et al., 2006; van der Horst et al., 2017). Therefore, we expect a comparable effect and an impact on transition research.
Strengths and Limitations
A strength of this study is that a well-established methodological approach was used to reach a consensus over a new definition. Approximately 30% of the invited experts were members of the TRANS-SENIOR Consortium with a focus on care transitions. The rest of the participants strengthened this study further by providing various perspectives because they came from different countries and diverse backgrounds.
A limitation of our Delphi survey was the relatively low response rate among experts invited to participate. Nevertheless, the recruitment aim of approximately 20–50 experts was reached. Second, the literature search was limited to only two databases; however, data saturation was achieved. This study presents the views of only researchers and providers, which leads to another limitation: even though a patient perspective was incorporated into the new definition during the Delphi process, patients or their representatives were not personally involved in the process. Furthermore, the literature review was limited to English-language publications. On the other hand, it was rational to consider English-language publications because the literature review focused on terminology in English, and the results were reported in English. Within and among countries, there are considerable differences in health that are closely linked with social conditions (Commission on Social Determinants of Health, 2008). Political, social, and economic forces in turn shape these conditions (Commission on Social Determinants of Health, 2008). Obviously, different countries have different social conditions, which might also affect how people view and perceive health and health care. This leads to another limitation of this study: some potentially different and important ideas may not have been collected and incorporated in the resulting definition, because the Delphi study involved experts only from certain countries (predominantly European), while other countries with different social conditions were not covered. Hence, this study represents the views of experts from predominantly developed countries with developed health systems, which may limit the applicability of the findings, especially for other, non-European countries or countries with developing health care systems. In addition, invitations to participate in the Delphi study were sent to experts identified by using our institute’s network. Most of the identified experts resided in Germany, which explains the prevalence of German experts in the pool of invited individuals. However, because the survey was anonymous, we did not have data on those who participated, as participants’ characteristics were not collected to guarantee anonymity. Hence, the number of participating experts from a particular country remained unknown.
Implications and Future Research
Although the consensus-based definition could be used in research and in practice, it may require additional evaluation and enhancement. Further studies with different designs are needed that seek the perspectives of a more diverse pool of participants, for example, frontline clinical providers, patients, patient representatives, and patients’ families and caregivers. Involving experts from other, non-European countries or countries with developing health care systems will certainly be beneficial to further enrich the definition. Careful translation of the definition into various languages will ensure its widespread use.
Growing research points to the importance of identifying and reducing avoidable care transitions due to the increased burden on patients and health systems. However, the phenomenon of avoidable care transitions has been interpreted differently across studies, and no consensus has been reached thus far. The absence of a commonly accepted, consensus-based definition for this phenomenon may have contributed to limited comparability across studies and hindered the identification of avoidable transitions. Efforts have been made to discriminate avoidable care transitions from other types of transitions, but there is still disagreement on how to systematically define and identify such avoidable care transitions (Shams et al., 2015). It seemed logical to systematically define the phenomenon of avoidability in the first place before addressing the identification of avoidable care transitions. Therefore, it was vital to come up with a new definition first to “speak the same language” when addressing avoidable care transitions.
The new definition is rather general and nonspecific to a particular care transition and population. The definition’s multiple aspects allow its use across different care settings in countries with predominantly developed health care systems. The definition can be used not only as a single guide but also in conjunction with other means in the decision-making process, such as local guidelines and expert opinions. Furthermore, it can be used not only to develop new guidelines, policies, and decision tools that touch upon avoidable care transitions but also to analyze and adapt existing tools.
In the case of a transition from an NH to a hospital, decision-makers guided by the new definition will ask themselves the following questions: Will the patient receive a much higher potential benefit in a hospital setting as opposed to the risks associated with the transfer or staying at a nursing home? Can the patient achieve a comparable health outcome in a lower resource setting, for example, in an ambulatory care setting? Does the patient or his or her caregiver prefer a transition to a hospital? Asking oneself these questions in practice may be challenging. However, this can be achieved by designing educational programs that are rooted in comprehensive theoretical frameworks for the implementation of innovations (e.g., active implementation frameworks, www.activeimplementation.org).
As older adults tend to prefer aging in place (Vasunilashorn et al., 2012), their right of choice becomes particularly essential in light of the increasing risk of frequent care transitions when a person gets older. This points to the importance of patient preferences in decision-making, which was addressed in the consensus-based definition but was not covered in the former definitions. The new definition has dimensions related to clinical parameters, resource utilization, and patients’ preferences and thus represents the voices of health professionals and the perspectives of health care service users. This delivers added value to the new definition as (1) it engages diverse stakeholders in the decision-making process and (2) it supports the concept of aging in place, as older adults may prefer to stay in their homes as long as possible despite increased risk.
Because older adults are at increased risk of frequent transitions and associated negative outcomes, it is possible that the new definition may be applied more frequently in situations involving older adults as opposed to situations involving younger individuals. Thus, older adults may represent a larger proportion of the population who might benefit from decisions guided by the new definition. In particular, this may help to reduce unnecessary transitions and associated negative outcomes such as moral hazard and unnecessary treatment for older adults. In addition, this may save substantial health care costs, which may be further allocated to the medical management of those older adults who truly need it.
Implications
The adverse impact of avoidable care transitions and the lack of consensus on what avoidable care transitions mean underline the importance of this research. The newly developed definition has the potential to improve the shared understanding of avoidable care transitions and is now available for use in a variety of contexts, including policy-making, intervention development, research, and quality and safety management in health care. In particular, the consensus-based definition can further guide studies aimed at identifying and reducing avoidable care transitions and support the classification and synthesis of these studies.
Funding
This work was supported by the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie Actions (grant number 812656). The funders had no role in the design of the study, data collection, analysis, interpretation, or preparation of the manuscript.
Conflict of Interest
None.
Data Availability
All the data generated or analyzed during this study are not publicly available. The data analysis from the literature review may be provided by the corresponding author upon reasonable request. Delphi survey data are not available because the participants were informed that access was granted only to the research team.
Acknowledgments
We wish to thank Carlotta Micaela Jarach for her assistance during the full-text screening phase of the literature review.
Author Contributions
All of the authors participated in the design of this study. Data collection: All authors. Data extraction: All authors. Data interpretation and analysis: All authors. Drafting of the manuscript: R. Makhmutov. Critical revision of the manuscript: All authors. Supervision: G. Meyer, M. E. Ellen, and S. Fleischer. All of the authors read and approved the final manuscript.
Ethics Approval and Consent to Participate
An official document was received on October 29, 2020 (# 2020-179), from the Ethical Committee (Medical Faculty, Martin Luther University Halle-Wittenberg) stating that no formal ethical approval was needed because this study was conducted in accordance with the data protection requirements and the ICH-GCP guidelines. Information on the survey was sent directly to the potential participants. All the addressed individuals had the opportunity to ask questions about the survey beforehand. In the Introduction section of the online Delphi survey, participants were informed that starting the survey indicated their informed consent to take part in the survey and to provide the data for analysis.




Comments