-
PDF
- Split View
-
Views
-
Cite
Cite
Rachel Emmott, Sophy K Barber, Wendy Thompson, Antibiotics and toothache: a social media review, International Journal of Pharmacy Practice, Volume 29, Issue 3, June 2021, Pages 210–217, https://doi.org/10.1093/ijpp/riaa024
Close - Share Icon Share
Abstract
Antibiotics are inappropriate for the treatment of toothache, yet many seek them. Social media allows users to express their opinions, share experiences and offer support. This study used social media to investigate the public’s experiences of, and attitudes towards, antibiotics for toothache.
A systematic search of posts on Facebook and Twitter was undertaken. Eligibility criteria were applied to select relevant social media posts for thematic analysis of word content. An inductive descriptive coding system was developed from the data and exemplary quotes were identified to illustrate the themes and subthemes identified.
Key findings Searches identified 174 posts, of which 144 were selected for analysis. Five themes were identified: experience and expectations, self-care and professional treatment, access to dental care, quality of life and coping strategies. The belief that antibiotics are an appropriate treatment for a toothache was widespread. Antibiotic-seeking behaviour was related to access to professional dental care, including avoiding dental appointments due to dental anxiety and the perceived affordability of dentistry. A range of strategies to cope with the severe impact toothache was having on people’s quality of life were identified, from prayer to antibiotics.
Social media is used extensively to seek antibiotics, avoid dental treatment and provide support to people with toothache. A general belief that antibiotics are an appropriate and necessary treatment for toothache exists. This improved understanding about the factors driving antibiotic-seeking behaviour provides new targets for the development of approaches to tackling antibiotic resistance, by reducing unnecessary antibiotic use in dental clinics and beyond.
Introduction
Across the globe, antimicrobial resistance continues to spread, resulting in a growing number of infections becoming harder to treat as the drugs used to treat them become less effective.[1] Whilst antimicrobial resistance occurs naturally over time, usually, through genetic changes, the misuse and overuse of antimicrobials are accelerating this process.[1] The World Health Organization (WHO) global action plan on antimicrobial resistance focuses on improving awareness and understanding about antimicrobial resistance, reducing the incidence of infections, and optimizing the use of antimicrobial agents.[2]
Internationally, dentists are estimated to be responsible for 10% of all antibiotics prescribed to humans.[3] Studies in the United Kingdom (UK) and United States (US) have shown up to 80% of dental antibiotic use is unnecessary.[4–6] Internationally, dental antibiotic guidelines vary to account for local contextual differences, such as patterns of antibiotic resistance and access to dental services.[7] Generally, national guidelines for treating dental pain and/or infection are based on the principle of removing the cause of dental pain and/or infection using a procedure such as extraction of a tooth.[8–10] Antibiotics do not cure toothache and are only required for a spreading infection.[9, 11, 12]
A range of non-clinical factors influencing dentists’ decisions to prescribe antibiotics for adults with acute dental conditions have been identified, with patient expectations and pressure reported as particularly important.[13, 14] People are known to regularly seek antibiotics for toothache from non-dental professionals, including general practitioners (GPs) and in the emergency department.[15, 16] Self-medication by people with a toothache is also reported.[17, 18] Much has been published about antibiotic prescribing behaviour by dentists and a variety of antibiotic stewardship interventions targeting the prescriber’s decision-making process exist.[14, 19–21] Little has been published, however, from the perspective of those with the toothache.[14, 22]
Social media describes ‘websites and applications that enable users to create and share content or to participate in social networking.’ [23] It provides an accessible, real time account of people’s experiences and opinions from across the world.[24] Social media has been used for investigating public experience and opinion about other dental topics including wisdom teeth,[25] dental trauma,[26] and hypodontia.[24] These studies have shown social media is used for sharing experiences, seeking information and offering support. Two social media studies have been published that examine antibiotic discussion on Twitter: both presented quantitative data and were outside of dentistry. The first study assessed the quantity of antibiotic mentions on Twitter to determine the reason behind variation in how often antibiotics were mentioned.[27] The second looked at the number of health-related topics being discussed on Twitter, including those related to antibiotics.[28]
This study aimed to investigate people’s experiences of and attitudes towards antibiotics for toothache. This information is important for the wider and future ambition of developing new, person-centered, evidence-based approaches to tackling antibiotic resistance.
Methods
The research was a cross-sectional study in three stages: a search of posts on social media, selection of relevant posts for analysis, and thematic analysis of the word content of posts. For this study, Twitter and Facebook were selected as two of the most popular social media platforms where people share their thoughts and experiences in the written word. Photo-sharing platforms, such as Instagram and Tumblr were not included in this study because analysing imagery was outside the scope of the study. The terms of service of Facebook[29] and Twitter[30] state that posting content authorises any user across the world to copy and publish this in any format; however, ethical approval was sought from the University of Leeds Dental Student Ethics Committee (FYP2019SOCMED, approval granted 3 July 2019) regarding the ethical use of social media data, as per best practice guidance.[31]
A systematic search of posts on the social media platforms Facebook and Twitter was undertaken by one researcher (RE) on 3 September 2019 using the search term: ‘antibiotic dentist toothache’. No restriction was placed on the location of those posting on social media and it was not possible to identify where all posts originated. Based on previous social media reviews, a sample size of at least 40 posts per platform was deemed sufficient to allow meaningful analysis. Initial searches of public posts between September 2018 and 2019 yielded insufficient Facebook posts, so Facebook posts from the period September 2017 through August 2018 inclusive were added, using the term ‘antibiotic toothache’. Pre-defined eligibility criteria were applied to select the dataset for analysis (Table 1). Data were extracted by one RE. All posts were anonymised to maintain confidentiality and prevent bias during analysis.
| Criteria . | Included . | Excluded . |
|---|---|---|
| Author | Member of the public affected by or supporting others with toothache. | Dental healthcare professionals Academics/researchers Commercial use |
| Language | English language | Not in English language |
| Type of post | Written word | Photographs Emojis Advertisements |
| Audience | Friends and family General public Healthcare professionals | Nil |
| Criteria . | Included . | Excluded . |
|---|---|---|
| Author | Member of the public affected by or supporting others with toothache. | Dental healthcare professionals Academics/researchers Commercial use |
| Language | English language | Not in English language |
| Type of post | Written word | Photographs Emojis Advertisements |
| Audience | Friends and family General public Healthcare professionals | Nil |
| Criteria . | Included . | Excluded . |
|---|---|---|
| Author | Member of the public affected by or supporting others with toothache. | Dental healthcare professionals Academics/researchers Commercial use |
| Language | English language | Not in English language |
| Type of post | Written word | Photographs Emojis Advertisements |
| Audience | Friends and family General public Healthcare professionals | Nil |
| Criteria . | Included . | Excluded . |
|---|---|---|
| Author | Member of the public affected by or supporting others with toothache. | Dental healthcare professionals Academics/researchers Commercial use |
| Language | English language | Not in English language |
| Type of post | Written word | Photographs Emojis Advertisements |
| Audience | Friends and family General public Healthcare professionals | Nil |
Thematic analysis was undertaken following the method described by Braun and Clarke.[32] Following familiarisation with the dataset, each post was divided into meaningful units based on content to allow examination of meaning. This highlighted topics and patterns within the data from which initial thematic coding was generated by the primary RE. Overall themes with similarities were linked to produce a framework of themes and subthemes. The data and framework were reviewed by the authors (SB and WT) to finalise the framework. Any disagreements were resolved through discussion between the authors. To avoid bias as far as possible during the thematic analysis, particularly when assessing the values and beliefs implicit in posts, the authors undertook individual and group reflection.
Quotes were chosen to illustrate each of the subthemes and provide concise and interesting accounts from the data. Each quote is presented verbatim – no attempt has been made to correct grammar or spelling. To ensure post authors could not be identified based on the quotes used, the excerpts were input back into the social media platform search function before inclusion in the presented results.
Results
In total, searches identified 174 posts from Twitter (n = 120) and Facebook (n = 54). Following application of the eligibility criteria, 30 posts were excluded: 14 posts from dental professionals, nine educational posts, five from research bodies or professional dental associations and two advertisements. The final dataset contained 144 posts (n = 105 and n = 39 respectively).
Thematic analysis identified five main themes: 1) experience and expectations; 2) self-care and professional treatment; 3) access to dental care; 4) quality of life; and 5) advice and coping strategies. Subthemes and illustrative quotes from the data are presented below for each theme.
Experiences and expectations
Previous experiences of antibiotics and/or dental treatment together with the beliefs and expectations expressed by post authors (see Figure 1) found that the social media users frequently expected antibiotics would be the outcome of dental appointments.
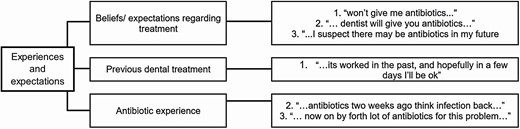
‘Experiences and expectations’ theme and subthemes together with illustrative quotes.
…so I’m going to go back to the dentist this morning for antibiotics…
The emergency department (A&E) and GPs were both identified as avenues for obtaining antibiotics for toothache.
… go to the nearest A&E they can prescribe antibiotics…
Antibiotic prescriptions were often associated automatically with the toothache. Frustration or disappointment were often expressed when antibiotics were not provided.
…I ask for antibiotics to be told that don’t prescribe freely so refused to give me any… WHAT IS THE MATTER WITH THESE PEOPLE!
Some social media users reported previous experience of antibiotic prescription being the only treatment provided for dental pain. Several had experienced the failure of antibiotics to cure the toothache.
nothing like having a mysterious tooth ache reappear
Self-care and professional treatment
The self-care and professional treatment theme included self-medication and antibiotic seeking behaviour by the social media users (see Figure 2). Some people reported self-medication with antibiotics and/or painkillers.
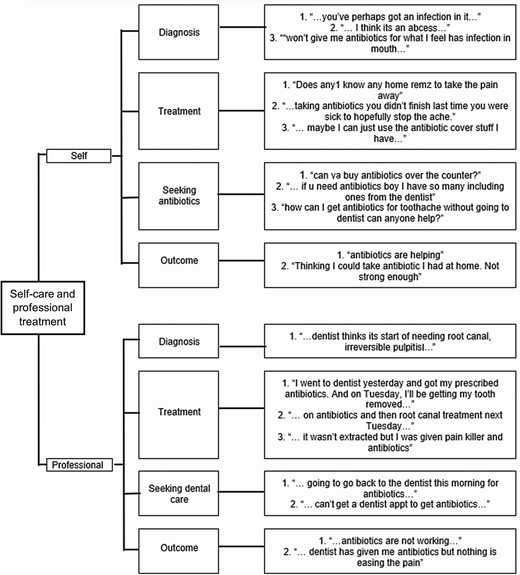
‘Self-care’ and ‘Professional’ theme and subthemes together with illustrative quotes.
Thinking I could take antibiotic I have at home.
Advice about the ‘strongest’ available painkillers to help relieve symptoms was commonly sought.
Does any1 know any home remz to take the pain away
Some social media users requested antibiotics from friends and social media followers, including the purchase of any spare antibiotics left over from previous prescriptions, or advice about how to acquire antibiotics without having to attend a dental appointment.
PLEASE! If anyone is awake and has any strong pain killers or antibiotics for toothache… Il come to you and pay whatever…
Of those who sought professional treatment, more than a third of posts stated the aim of their appointment was to get antibiotics. Whilst most talked about visiting the dentist, a few described visiting a ‘doctor’ or ‘urgent care’.
I need to get antibiotics TODAY either from GP or dentist…
Several posts explained antibiotic treatment had not improved their symptoms and, for some, their condition had worsened. Adverse effects associated with antibiotics, such as ‘sickness’ and ‘yeast infection’ were discussed as recognised and/or accepted side-effects. Some post authors talked about the failure of antibiotics to resolve their problem or of them working only for a short period before ‘infection back.’
and it’s just getting worse
I’ve been dentist for the last 6 months with toothache
all they keep doing is giving antibiotics instead of sorting it out
Access to dental care
Availability and the cost of dental treatment were the most prominent factors associated with access the dental care (see Figure 3). One reported barrier to accessing care was people’s ability to get dental appointments on the same day, with some users reporting having to wait up to a week before access to professional treatment was available.
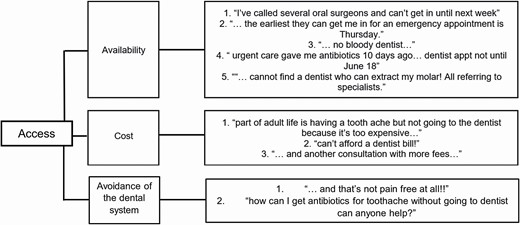
‘Access’ theme and subthemes together with illustrative quotes.
…can’t get in emergency dentist again
The desire to avoid a dental appointment was frequently expressed as a reason for seeking antibiotics, often underpinned by fear of dental treatment.
…That needle!!! Sob
Waiting times for more specialist treatment was an issue, with some people reporting suffering and pain for prolonged periods while awaiting specialist services.
…can’t do the root canal until Thursday and its been over 36 hours of pain…
There was a general expectation that all dental treatment would have a high cost and “too expensive.” Cost differences between the UK and US dental systems were identified by some.
paid $300 for treatment and $150 for antibiotics and pain relief,
no root canal treatment or crown… I love our #NHS
Quality of life
Toothache placed a significant physical, emotional, and social strain on people which subsequently impacted negatively on their quality of life (see Figure 4). More than half of all analysed posts portrayed an element of physical pain of varying severity, including ‘agony’, ‘excruciating’, and ‘unbearable.’
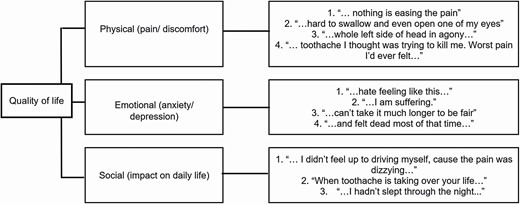
‘Quality of life’ theme and subthemes together with illustrative quotes.
Other physical symptoms reported alongside toothache included ‘dizziness’, ‘headache’, ‘numbness’, and ‘sickness’. Generally, people reported feeling ‘fed-up’ due to prolonged periods of pain and difficulty sleeping. A feeling of inability to cope and issues needing to be overcome to continue daily activities was evident, including the inability to drive, lost productivity and missed social events.
When toothache is taking over your life…
…walking the dog was taxing…
Several accounts reported people making significant changes to their daily life to deal with their toothache.
…so I booked some leave from work.
Some social media users expressed concerns that current symptoms would become worse both in the sense of pain and development of more serious (even life-threatening) conditions.
… A toothache can turn into death. All the infection!!!…
Advice and coping strategies
Advice and support on ways to deal with their pain were requested and/or provided based on the social media user’s previous experience of dental pain (Figure 5). Techniques that people used to help cope with the pain included ‘a day in the sauna’, ‘cuddle a cat’, ‘get drunk’ and ‘sleep’. The importance of attending the dentist as soon as possible was highlighted in nearly half of all posts.
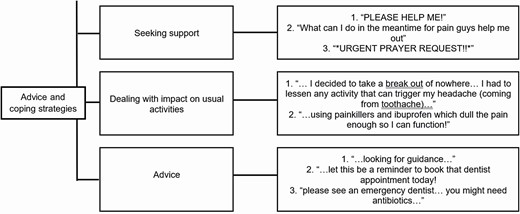
‘Advice and coping strategies’ theme and subthemes together with illustrative quotes.
go to a dentist if you can. You shouldn’t really self-administer antibiotics
Knowledge about the potential worsening of symptoms if professional treatment was not sought was frequently shared. There were also shared anecdotes warning about the risks of allowing symptoms to continue without treatment.
…Don’t eff around with your teeth friends. Get it taking care of immediately.
I never knew how serious the outcome could be…
Discussion
Social media is used extensively to seek antibiotics and provide support to people with the toothache. Antibiotic-seeking behaviour was found to be driven by the belief that antibiotics cure toothache, a desire to avoid dental treatment (often due to dental phobia/anxiety) and perceived difficulties accessing urgent dental services. Previous experience of antibiotics for the toothache was widespread, including prescribed by healthcare professionals.
An important strength of this research tool derives from the insight social media provides into peer-to-peer discussion, without the influence of an observer or interviewer.[33] A key limitation is the nature of social media and its users. Different platforms are used by different types of people for different reasons, so the results may not be representative of society.[31] Whilst Facebook had 2.5 billion users in 2019, most were aged 25–34.[34] Only posts in English were selected as the result of the study are intended to inform interventions for an English-speaking audience, although it is recognised that this limited the extent to which the results are internationally relevant. Excluding posts that included images and employing just two social media platforms may have produced a narrower range of issues identified in the results. Due to privacy settings, not all data on the platforms were available. As a result, relevant discussions may have been missed when collecting data and identifying themes. The individual bias of the researchers when interpreting post content and constructing a thematic framework is an inherent limitation on thematic review.[32] As only clinician researchers undertook the study, there is potential that themes were missed which public-patient involvement in the analysis would have identified.
Whilst antibiotics do not cure toothache [12, 35], it should be surprising that so many of the social media users had experienced taking antibiotics for toothache. However, overprescribing of antibiotics for acute dental conditions has been widely reported [4, 6] and studies report high rates of people believing that antibiotics alleviate dental pain (almost 70% in a Saudi study).[36] Whilst patient influence on dental antibiotic prescribing decisions have been widely reported in studies of dentists,[4, 13, 37–40] the extent of antibiotic-seeking by patients has been questioned by some researchers based on their finding of ‘scant evidence’ that people actually pressure clinicians for antibiotics.[41] Antibiotic-seeking behaviour has recently been described in an ethnographic study of urgent dental appointments in UK.[14] This review of social media adds important evidence from the public-patient perspective to the scant literature on antibiotic-seeking behaviour.
People were shown to seek antibiotics from a variety of sources, suggesting toothache places a burden on the healthcare system outside of dentistry. This has been previously reported in studies from around the world, with antibiotics for acute dental conditions sought from GPs and the emergency department.[15, 16, 42–44] An editorial aimed at GPs has identified novel routes to obtaining antibiotics in the UK associated with a lower threshold for prescribing and issuing of antibiotics without medical assessment.[45] The importance of controlling access to antibiotics is clearly important for efforts to tackle antibiotic resistance and must include sources outside of the healthcare sector. A study of non-prescribed antibiotic use in Low and Middle Income Countries (LMICs) also identified health-seeking behaviour as an important driver and highlighted the need for strategies aimed at tackling antibiotic resistance to address this behaviour.[46]
Antibiotics were being used as a substitute for dental procedures by some to treat toothache. Barriers to accessing urgent dental care were reported as anxiety about dental treatment, the cost of treatment, and the difficulty of taking time off work. Access to urgent dental care has been previously reported as a factor influencing antibiotic prescribing for acute dental conditions.[37, 47] The impact of severely restricted access to face-to-face dental services on antibiotic prescribing has been highlighted during the COVID-19 crisis, when dental antibiotic prescribing was found to increase by 25% in England.[48] Dental phobia is also well known to be associated with avoidance of dental care and the most recent UK national survey of adult dental health found 12% of respondents to self-report as suffering from the condition.[49] Where access to dental services is a problem, health service delivery changes to improve access to urgent dental care, including addressing issues thatdrive people to avoid care (such as dental phobia), will make an important contribution to efforts to optimise dental antibiotic use.
The severe impact toothache can have on people’s quality of life was previously reported [44] and studies have looked at the pain-relief and self-care strategies employed to reduce its impact.[50] Identifying Twitter as a potentially useful route for spreading messages about antibiotic resistance to the general population was also not a new finding.[51] However, demonstrating that people choose to use social media for advice and support about antibiotics and toothache has not been previously reported. Whilst studies have questioned the value of generalised public health campaigns about antibiotic resistance [52], the results of this review suggest that social media (and Twitter more than Facebook) may present a suitable route to engage with people about antibiotics. More users of Twitter than Facebook were found in this study to have posted about toothache and antibiotics; this may be important for future public engagement on dental antimicrobial stewardship.
As highlighted in previous studies, however, the optimum way to engage people and provide the professional support that they seek via social media requires further research.[51] This preliminary study provides evidence that more thorough data mining and sentiment analysis would be helpful to understand individual and community behaviour towards antibiotics and toothache. This may be an important way for the dental profession to contribute to delivery of the WHO global action plan’s strategic goal of improving awareness of antimicrobial resistance [2] and designing new approaches to antimicrobial stewardship.
Conclusions
Social media is used by people sharing experiences, obtaining advice and offering support about antibiotics for toothache. Some people believe antibiotics are always the appropriate treatment for toothache and are frustrated or disappointed when they are not prescribed. Antibiotic-seeking behaviour has been clearly observed. Managing this behaviour by addressing people’s expectations and desire for antibiotics to cope with toothache, should be included in the future interventions to tackle antibiotic resistance.
Access to dental care was identified as an important reason underpinning the observed antibiotic-seeking behaviour. Ensuring appropriate access to professional dental care for those with acute toothache, including for people with a dental anxiety/phobia and people on low incomes, should be integral to health services reviews of dentistry. In this way, toothache can be treated with dental procedures, and effective antibiotics conserved for when they are necessary to treat people with severe infections.
Acknowledgements
With thanks to the many users of social media around the world.
Author contributions
Conceptualization, W.T and R.E.; methodology, S.B.; formal analysis, R.E and S.B.; data curation, R.E.; writing—original draft preparation, R.E..; writing—review and editing, S.B and W.T.; visualization, R.E.; supervision, W.T and S.B.; project administration, R.E.. The work was completed whilst authors S.B. and W.T were initial National Institute for Health Research (NIHR) Doctoral Research Fellows and latterly NIHR Clinical Lecturers. All authors have read and agreed to the published version of the manuscript.
Funding
This research was undertaken as part of the lead author’s undergraduate studies and as such received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare no conflict of interest.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.



