-
PDF
- Split View
-
Views
-
Cite
Cite
Ching-Hua Lin, Feng-Chua Chen, Hung-Yu chan, Chun-Chi Hsu, Time to Rehospitalization in Patients With Schizophrenia Receiving Long-Acting Injectable Antipsychotics or Oral Antipsychotics, International Journal of Neuropsychopharmacology, Volume 22, Issue 9, September 2019, Pages 541–547, https://doi.org/10.1093/ijnp/pyz035
Close - Share Icon Share
Abstract
This study aimed to investigate and compare time to rehospitalization in patients with schizophrenia receiving long-acting injectable antipsychotics (LAIs) after discharge with those receiving oral antipsychotics. Additionally, the trend of LAIs prescription rates was investigated.
Patients with schizophrenia (n = 13 087), who were discharged from the study hospital from 2006 to 2017, were followed-up under naturalistic conditions in the year after discharge. The primary outcome was time to rehospitalization. Survival analysis was used in the comparisons between LAIs and oral antipsychotics and between FGA-LAIs and SGA-LAIs. Simple linear regression and Cochrane-Armitage trend test were used to test whether a time trend existed for LAIs prescription rates.
In the 1 year following discharge, patients in the LAIs group had a significantly lower rehospitalization rate and a significantly lengthened time to rehospitalization than those in the oral antipsychotics group. Rehospitalization rate and time to rehospitalization were not significantly different in patients receiving FGA-LAIs or SGA-LAIs. A significantly higher percentage of patients treated with FGA-LAIs received anticholinergic agents than those treated with SGA-LAIs. The LAIs prescription rate grew significantly from 2006 to 2017 by an average of 0.5% per year.
LAIs were significantly superior to oral antipsychotics in reducing rehospitalization risk, whereas SGA-LAIs were comparable with FGA-LAIs in reducing rehospitalization risk. However, use of concomitant anticholinergic agents was less frequent in the SGA-LAIs group than in the FGA-LAIs group. Increase in LAIs prescription rate may be due to growing experiences and success among clinicians in treating patients with LAIs.
Most of previous studies about the comparison between oral antipsychotics and LAIs or between different LAIs are randomized controlled studies or claim data studies. Randomized controlled studies are limited by highly selective population and poor generalizability. The disadvantage of claim data studies is that only limited variables can be collected. Therefore, we conducted a hospital-based study to investigate this issue. The main finding of this study was that patients receiving LAIs at discharge had a more favorable outcome in terms of rehospitalization. Compared with those in the oral antipsychotics group, patients in the LAIs group had a significantly lower rehospitalization rate. Another finding was that comparable rehospitalization rates and time to rehospitalization were seen in patients on FGA-LAIs and patients on SGA-LAIs. Additionally, the prescription rate of LAIs increased over time during the study period and the contribution mainly from the increasing of SGA-LAIs prescription.
Introduction
Schizophrenia is a chronic and debilitating disease, and antipsychotic medications are a cornerstone of effective treatment. However, patients’ lack of insight into their illness often results in challenges in long-term medication adherence (Lehman et al., 2004; Lieberman et al., 2005). For example, the Clinical Antipsychotic Trials of Intervention Effectiveness randomized controlled study in patients with schizophrenia found a 74% discontinuation rate of oral antipsychotics within 18 months of treatment initiation (Lieberman et al., 2005). The results of an 18-month, naturalistic study also demonstrated an oral antipsychotics discontinuation rate up to 60–90% in patients with schizophrenia (Chan et al., 2017). Another retrospective study revealed that more than 50% of patients with schizophrenia had experienced at least 1 relapse within 2 years, and 80% experienced at least 1 relapse within 5 years (Valenstein et al., 2006). Medication nonadherence often results in relapses, suicide attempts, violence, deterioration of functioning, and consequently the “revolving door” phenomenon of frequent psychiatric hospitalizations (Gilmer et al., 2004). As a result, hospitalization rate is a key driver of increasing psychiatric care costs.
Long-acting injectable antipsychotics (LAIs) have been developed to address nonadherence by eliminating the need for daily dosing through biweekly or monthly injections. However, they also have certain disadvantages, such as a limited selection of medications in this formulation, less flexibility in dosage adjustment, injection site reactions (e.g., pain, erythema, swelling, and discomfort), and delayed disappearance of adverse effects after discontinuation (Brissos et al., 2014). Since LAIs are released into the bloodstream slowly, missing an injection will not result in a fast drop in the blood drug level. They have been proved effective in schizophrenia because they assure stable blood drug levels over several weeks (Correll et al., 2016), leading to a reduced risk of treatment failure (e.g., relapse, rehospitalization, suicide, violence, or deterioration of functioning). Several clinical practice guidelines for the treatment of schizophrenia highlighted LAIs as an appropriate option for patients with a significant history of nonadherence (Lehman et al., 2004; Velligan et al., 2010).
Most of previous studies about the comparison between oral antipsychotics and LAIs or between different LAIs are randomized controlled studies or nationwide population-based claim data studies (Buckley et al., 2015; Yu et al., 2015). Randomized controlled studies are limited by highly selective population and poor generalizability. The disadvantage of claim data studies is that only limited variables can be collected with the problem of residual confounding. Under these circumstances, we conducted a hospital-based study to investigate this issue. We hypothesized that use of LAIs may facilitate continuity of treatment under real-world conditions. Therefore, LAIs would be superior to oral antipsychotics in reducing the risk of rehospitalization after patients with schizophrenia are discharged from the hospital. The primary goal of this study was to compare the effects of LAIs vs oral antipsychotics on time to rehospitalization after discharge in patients with schizophrenia. Covariates that may affect time to rehospitalization were adjusted for. LAIs were further divided into first-generation (FGA-LAIs) and second-generation (SGA-LAIs) antipsychotics, and the second goal of this study was to investigate whether SGA-LAIs were superior to FGA-LAIs in reducing rehospitalization risk. The third goal was to test whether a time trend existed for LAIs prescription rates during the study period.
Methods
Ethics
The current study was approved by the Kai-Syuan Psychiatric Hospital institutional review board and carried out in accordance with both the Declaration of Helsinki (2013) and Taiwan’s national legislation (Human Subjects Research Act, Taiwan). Informed consent was not required as all data were delinked before analysis to achieve anonymity.
Participants
This observational study with a retrospective cohort design was conducted at Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, a public, 820-bed psychiatric hospital located in southern Taiwan. The participants consisted of inpatients who met the DSM-IV-TR or DSM-5 criteria for either schizophrenia or schizoaffective disorder (APA, 2000, 2013) and were discharged on LAIs or oral antipsychotics between January 1, 2006 and December 31, 2017. The diagnoses were made by board-certified psychiatrists and supported by clinical observations and interviews during hospitalization, past medical records, and information provided by main caregivers.
Follow-up Procedures
After discharge, the patients were followed-up in the outpatient clinic at Kai-Syuan Psychiatric Hospital. The frequency of outpatient visits were based on clinical conditions and ranged from weekly, biweekly, and monthly to trimonthly. Apart from routine education and counseling, no other specialized care or therapy was provided. Rehospitalizations within 1 year of discharge were reviewed. Rehospitalization was clinically indicated for patients presenting with relapse/recurrence of significant psychotic symptoms, dangerous or violent behavior, or deteriorated functioning who were also not responding adequately to outpatient treatment (Lehman et al., 2004). Patients with no clinic visits after discharge, incomplete prescription data, as well as those who participated in clinical trials during the index hospitalization or outpatient follow-up period were all excluded.
According to Taiwan National Health Insurance Administration policy, “refill prescriptions for patients with chronic illnesses” refers to prescriptions that can be refilled for patients with stable chronic illnesses. The prescription is valid for no more than 90 days and can be filled up to 3 times. Treatment discontinuation was defined as lack of attendance to the outpatient clinic for more than 3 months during the 1-year follow-up period. Date of the last outpatient visit was recorded as the discontinuation date.
Statistical Analyses
Time to rehospitalization was used as the primary outcome measure in the comparisons of LAIs vs oral antipsychotics and FGA-LAIs vs SGA-LAIs in this study. Covariates included sex, involuntary hospitalization, discharge against medical advice, age, age at onset, duration of index hospitalization (days), and number of previous hospitalizations. All tests were 2-tailed, and significance was defined as an alpha of <0.05. Data were analyzed using the SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL), SAS 9.3 software (SAS Institute Inc, Cary, NC), and MedCalc (MedCalc Software, Belgium).
Pearson’s chi-squared test and independent t test were used to compare clinical characteristics between groups. Kaplan-Meier survival analysis was used to determine time to rehospitalization and time to discontinuation, and the significance of between-group difference was analyzed using the log-rank test. The Cox proportional hazards multivariate regression was used to adjust for covariates that may affect time to rehospitalization. Finally, simple linear regression was used to test whether a linear trend existed for LAIs prescription rates from 2006 to 2017. The dependent variable was LAIs prescription rate and the independent variable was time (measured in years) (Anderson, 2013). We also performed Cochran-Armitage trend test to evaluate the statistical significance of the time trend in LAIs prescription rates.
Results
Demographic and Clinical Characteristics
A total of 13 087 patients were discharged during the study period, and 12 169 were included in the analysis. Among the 12 169 discharged patients, 1923 (15.8%) received LAIs, and 10 246 (84.2%) received oral antipsychotics at discharge. Among the 1923 patients receiving LAIs, 1549 (80.6%) received FGA-LAIs (flupenthixol decanoate = 18.2% [n = 282], haloperidol decanoate = 81.8% [n = 1267]) and 374 (19.4%) received SGA-LAIs (risperidone LAI = 100% [n = 374]). A total of 926 (7.6%) of 12 169 patients were lost to follow-up.
Characteristics of the LAIs group and the oral antipsychotics group are shown in Table 1. There was no statistically significant difference between the 2 groups with respect to sex, discharge against medical advice, age, age at onset, duration of illness, and number of previous hospitalizations. Compared with the oral antipsychotics group, the LAIs group had a significantly higher rate of involuntary admission and shorter hospital stays during index hospitalization.
| . | Total . | LAIs . | OAPs . | . | |||
|---|---|---|---|---|---|---|---|
| . | (n = 12 169) . | (n = 1923) . | (n = 10 246) . | . | |||
| . | n . | % . | n . | % . | n . | % . | Pa . |
| Sex | |||||||
| Male | 5274 | 43.3 | 803 | 41.8 | 4471 | 43.6 | .127 |
| Female | 6895 | 56.7 | 1120 | 58.2 | 5775 | 56.4 | |
| Involuntary hospitalization | |||||||
| Yes | 705 | 5.8 | 203 | 10.6 | 502 | 4.9 | <.001 |
| No | 11 464 | 94.2 | 1720 | 89.4 | 9744 | 95.1 | |
| Discharge against medical advice | |||||||
| Yes | 1143 | 9.4 | 176 | 9.2 | 967 | 9.4 | .694 |
| No | 11 026 | 90.6 | 1747 | 90.8 | 9279 | 90.6 | |
| Mean | SD | Mean | SD | Mean | SD | Pb | |
| Age (years) | 43.1 | 11.8 | 43.3 | 11.0 | 43.1 | 12.0 | .312 |
| Age at onset (years) | 32.4 | 12.0 | 32.7 | 11.2 | 32.3 | 12.1 | .238 |
| Duration of illness (years) | 10.7 | 8.8 | 10.7 | 8.3 | 10.7 | 8.9 | .803 |
| Duration of index hospitalization (days) | 155.0 | 342.4 | 120.8 | 261.8 | 161.4 | 355.1 | <.001 |
| No. of previous hospitalization | 3.8 | 5.4 | 4.1 | 5.5 | 3.8 | 5.4 | .057 |
| . | Total . | LAIs . | OAPs . | . | |||
|---|---|---|---|---|---|---|---|
| . | (n = 12 169) . | (n = 1923) . | (n = 10 246) . | . | |||
| . | n . | % . | n . | % . | n . | % . | Pa . |
| Sex | |||||||
| Male | 5274 | 43.3 | 803 | 41.8 | 4471 | 43.6 | .127 |
| Female | 6895 | 56.7 | 1120 | 58.2 | 5775 | 56.4 | |
| Involuntary hospitalization | |||||||
| Yes | 705 | 5.8 | 203 | 10.6 | 502 | 4.9 | <.001 |
| No | 11 464 | 94.2 | 1720 | 89.4 | 9744 | 95.1 | |
| Discharge against medical advice | |||||||
| Yes | 1143 | 9.4 | 176 | 9.2 | 967 | 9.4 | .694 |
| No | 11 026 | 90.6 | 1747 | 90.8 | 9279 | 90.6 | |
| Mean | SD | Mean | SD | Mean | SD | Pb | |
| Age (years) | 43.1 | 11.8 | 43.3 | 11.0 | 43.1 | 12.0 | .312 |
| Age at onset (years) | 32.4 | 12.0 | 32.7 | 11.2 | 32.3 | 12.1 | .238 |
| Duration of illness (years) | 10.7 | 8.8 | 10.7 | 8.3 | 10.7 | 8.9 | .803 |
| Duration of index hospitalization (days) | 155.0 | 342.4 | 120.8 | 261.8 | 161.4 | 355.1 | <.001 |
| No. of previous hospitalization | 3.8 | 5.4 | 4.1 | 5.5 | 3.8 | 5.4 | .057 |
Abbreviations: LAIs, long-acting injectable antipsychotics; OAPs, oral antipsychotics.
Bold, statistically significant.
a Pearson’s χ 2 test.
b Independent t test
| . | Total . | LAIs . | OAPs . | . | |||
|---|---|---|---|---|---|---|---|
| . | (n = 12 169) . | (n = 1923) . | (n = 10 246) . | . | |||
| . | n . | % . | n . | % . | n . | % . | Pa . |
| Sex | |||||||
| Male | 5274 | 43.3 | 803 | 41.8 | 4471 | 43.6 | .127 |
| Female | 6895 | 56.7 | 1120 | 58.2 | 5775 | 56.4 | |
| Involuntary hospitalization | |||||||
| Yes | 705 | 5.8 | 203 | 10.6 | 502 | 4.9 | <.001 |
| No | 11 464 | 94.2 | 1720 | 89.4 | 9744 | 95.1 | |
| Discharge against medical advice | |||||||
| Yes | 1143 | 9.4 | 176 | 9.2 | 967 | 9.4 | .694 |
| No | 11 026 | 90.6 | 1747 | 90.8 | 9279 | 90.6 | |
| Mean | SD | Mean | SD | Mean | SD | Pb | |
| Age (years) | 43.1 | 11.8 | 43.3 | 11.0 | 43.1 | 12.0 | .312 |
| Age at onset (years) | 32.4 | 12.0 | 32.7 | 11.2 | 32.3 | 12.1 | .238 |
| Duration of illness (years) | 10.7 | 8.8 | 10.7 | 8.3 | 10.7 | 8.9 | .803 |
| Duration of index hospitalization (days) | 155.0 | 342.4 | 120.8 | 261.8 | 161.4 | 355.1 | <.001 |
| No. of previous hospitalization | 3.8 | 5.4 | 4.1 | 5.5 | 3.8 | 5.4 | .057 |
| . | Total . | LAIs . | OAPs . | . | |||
|---|---|---|---|---|---|---|---|
| . | (n = 12 169) . | (n = 1923) . | (n = 10 246) . | . | |||
| . | n . | % . | n . | % . | n . | % . | Pa . |
| Sex | |||||||
| Male | 5274 | 43.3 | 803 | 41.8 | 4471 | 43.6 | .127 |
| Female | 6895 | 56.7 | 1120 | 58.2 | 5775 | 56.4 | |
| Involuntary hospitalization | |||||||
| Yes | 705 | 5.8 | 203 | 10.6 | 502 | 4.9 | <.001 |
| No | 11 464 | 94.2 | 1720 | 89.4 | 9744 | 95.1 | |
| Discharge against medical advice | |||||||
| Yes | 1143 | 9.4 | 176 | 9.2 | 967 | 9.4 | .694 |
| No | 11 026 | 90.6 | 1747 | 90.8 | 9279 | 90.6 | |
| Mean | SD | Mean | SD | Mean | SD | Pb | |
| Age (years) | 43.1 | 11.8 | 43.3 | 11.0 | 43.1 | 12.0 | .312 |
| Age at onset (years) | 32.4 | 12.0 | 32.7 | 11.2 | 32.3 | 12.1 | .238 |
| Duration of illness (years) | 10.7 | 8.8 | 10.7 | 8.3 | 10.7 | 8.9 | .803 |
| Duration of index hospitalization (days) | 155.0 | 342.4 | 120.8 | 261.8 | 161.4 | 355.1 | <.001 |
| No. of previous hospitalization | 3.8 | 5.4 | 4.1 | 5.5 | 3.8 | 5.4 | .057 |
Abbreviations: LAIs, long-acting injectable antipsychotics; OAPs, oral antipsychotics.
Bold, statistically significant.
a Pearson’s χ 2 test.
b Independent t test
LAIs vs Oral Antipsychotics
A total 1153 (60.0%) patients in the LAIs group and 6621 (64.6%) in the oral antipsychotics group were rehospitalized within 1 year of discharge. The LAIs group had a significantly lower rehospitalization rate (χ 2 = 15.25, df = 1, P < .001) and a significantly lengthened time to rehospitalization than the oral antipsychotics group (LAIs, median time ± SE = 209.0 ± 11.0 days; oral antipsychotics, median time ± SE = 129.0 ± 3.7 days; log rank = 39.13, df = 1, P < .001) (Figure 1). In addition, the 2 groups were not significantly different with respect to discontinuation rate (LAIs = 7.5% [145/1923]; oral antipsychotics = 7.6% [781/10 246]; χ 2 = 0.02, df = 1, P = .901) or time to discontinuation (LAIs, mean follow-up time ± SE = 337.9 ± 2.2 days; oral antipsychotics, mean follow-up time ± SE = 333.5 ± 1.1 days; log rank = 2.16, df = 1, P = .141; median time to discontinuation was not reached for both groups) (Figure 2).
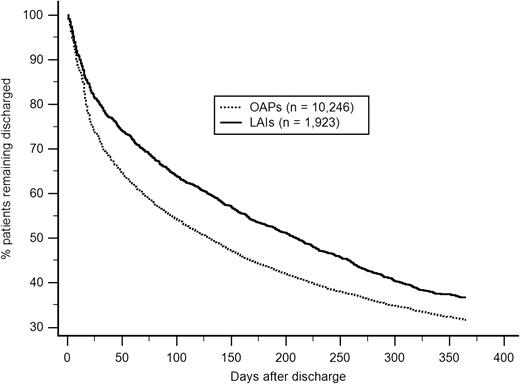
Time to rehospitalization in patients discharged on LAIs or OAPs (log rank = 39.13, df = 1, P < .001). LAIs = long-acting injectable antipsychotics, OAPs = oral antipsychotics.
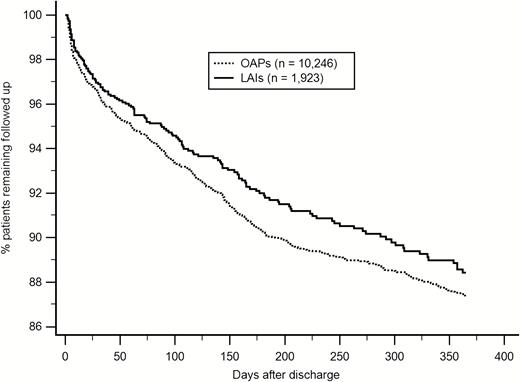
Time to treatment discontinuation in patients discharged on LAIs or OAPs (log rank = 2.16, df = 1, P = .141). LAIs = long-acting injectable antipsychotics, OAPs = oral antipsychotics.
After adjusting for covariates (i.e., sex, involuntary hospitalization, discharge against medical advice, age, age at onset, duration of index hospitalization, and number of previous hospitalizations) using Cox proportional hazards multivariate regression, treatment with LAIs was still associated with a significantly lengthened time to rehospitalization (adjusted hazard ratio [HR], 0.83; 95% confidence interval [CI], 0.78–0.88, P < .001), whereas time to discontinuation was not significantly different between the 2 groups (adjusted HR, 0.89; 95% CI, 0.74–1.06, P = .200).
FGA-LAIs vs SGA-LAIs
Between patients receiving FGA-LAIs and SGA-LAIs, there was no statistically significant difference in rehospitalization rate (FGA = 60.7% [940/1549]; SGA = 57.0% [213/374]; χ 2 = 1.75, df = 1, P = .186), time to rehospitalization (FGA, median time ± SE = 204.0 ± 12.5 days; SGA, median time ± SE = 225.0 ± 21.8 days; log rank test = 1.70, df = 1, P = .193), discontinuation rate (FGA = 7.1% [110/1549]; SGA = 9.4% [35/374]; χ 2 = 2.20, df = 1, P = .138), and time to discontinuation (FGA, mean time ± SE = 338.8 ± 2.4 days; SGA, mean time ± SE = 334.5 ± 5.2 days; log rank test = 1.55, df = 1, P = .214). After adjusting for covariates (i.e., sex, involuntary hospitalization, discharge against medical advice, age, age at onset, duration of index hospitalization, and number of previous hospitalizations) using Cox proportional hazards multivariate regression, patients receiving SGA-LAIs were similar to those receiving FGA-LAIs with respect to time to rehospitalization (adjusted HR, 0.93; 95% CI, 0.80–1.09, P = .373) and time to discontinuation (adjusted HR, 1.36; 95% CI, 0.92–2.00, P = .120).
A significantly higher percentage of patients treated with FGA-LAIs (63.1% = 997/1549) received anticholinergic agents than those treated with SGA-LAIs (46.0% = 172/374) (χ 2 = 39.56, df = 1, P < .001).
Trend of LAIs Prescription Rates
The coefficient of time (B = 0.005) was statistically significant (P = .015) in linear regression analysis. It indicated that during the study period (from 2006 to 2017), the LAIs prescription rate grew significantly by an average of 0.5% per year. Table 2 lists the LAIs prescription rates from 2006 to 2017. The results of Cochrane-Armitage trend test also showed a significant time trend of increasing LAIs prescription (Z = 4.92, P < .0001). Prescription rates of FGA-LAIs and SGA-LAIs were also obtained to determine their respective contribution to increasing LAIs prescription. The results showed that the prescription rate of FGA-LAIs did not increase (12.40% in 2006 and 11.66% in 2017), but the prescription rate of SGA-LAIs increased significantly (0.22% in 2006 and 9.84% in 2017) during the study period.
| Year . | 2006 . | 2007 . | 2008 . | 2009 . | 2010 . | 2011 . |
|---|---|---|---|---|---|---|
| Number of patients discharged . | n = 911 . | n = 963 . | n = 1011 . | n = 1047 . | n = 947 . | n = 1003 . |
| Patients receiving LAIs, n (%) | 115 (12.6%) | 125 (13.0%) | 167 (16.5%) | 167 (16.0%) | 136 (14.4%) | 146 (14.6%) |
| Patients receiving FGA-LAIs, n (%) | 113 (12.4%) | 119 (12.4%) | 158 (15.6%) | 162 (15.5%) | 131 (13.8%) | 129 (12.9%) |
| Patients receiving SGA-LAIs, n (%) | 2 (0.2%) | 6 (0.6%) | 9 (0.9%) | 5 (0.5%) | 5 (0.6%) | 17 (1.7%) |
| Year | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| Number of patients discharged | n = 1070 | n = 1029 | n = 1097 | n = 1043 | n = 1062 | n = 986 |
| Patients receiving LAIs, n (%) | 173 (16.2%) | 144 (14.0%) | 188 (17.1%) | 160 (15.3%) | 190 (17.9%) | 212 (21.5%) |
| Patients receiving FGA-LAIs, n (%) | 138 (12.9%) | 113 (11.0%) | 147 (13.4%) | 111 (10.6%) | 113 (10.6%) | 115 (11.7%) |
| Patients receiving SGA-LAIs, n (%) | 35 (3.3%) | 31 (3.0%) | 41 (3.7%) | 49 (4.7%) | 77 (7.1%) | 97 (9.8%) |
| Year . | 2006 . | 2007 . | 2008 . | 2009 . | 2010 . | 2011 . |
|---|---|---|---|---|---|---|
| Number of patients discharged . | n = 911 . | n = 963 . | n = 1011 . | n = 1047 . | n = 947 . | n = 1003 . |
| Patients receiving LAIs, n (%) | 115 (12.6%) | 125 (13.0%) | 167 (16.5%) | 167 (16.0%) | 136 (14.4%) | 146 (14.6%) |
| Patients receiving FGA-LAIs, n (%) | 113 (12.4%) | 119 (12.4%) | 158 (15.6%) | 162 (15.5%) | 131 (13.8%) | 129 (12.9%) |
| Patients receiving SGA-LAIs, n (%) | 2 (0.2%) | 6 (0.6%) | 9 (0.9%) | 5 (0.5%) | 5 (0.6%) | 17 (1.7%) |
| Year | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| Number of patients discharged | n = 1070 | n = 1029 | n = 1097 | n = 1043 | n = 1062 | n = 986 |
| Patients receiving LAIs, n (%) | 173 (16.2%) | 144 (14.0%) | 188 (17.1%) | 160 (15.3%) | 190 (17.9%) | 212 (21.5%) |
| Patients receiving FGA-LAIs, n (%) | 138 (12.9%) | 113 (11.0%) | 147 (13.4%) | 111 (10.6%) | 113 (10.6%) | 115 (11.7%) |
| Patients receiving SGA-LAIs, n (%) | 35 (3.3%) | 31 (3.0%) | 41 (3.7%) | 49 (4.7%) | 77 (7.1%) | 97 (9.8%) |
Abbreviations: FGA = first-generation antipsychotics; SGA = second-generation antipsychotics.
| Year . | 2006 . | 2007 . | 2008 . | 2009 . | 2010 . | 2011 . |
|---|---|---|---|---|---|---|
| Number of patients discharged . | n = 911 . | n = 963 . | n = 1011 . | n = 1047 . | n = 947 . | n = 1003 . |
| Patients receiving LAIs, n (%) | 115 (12.6%) | 125 (13.0%) | 167 (16.5%) | 167 (16.0%) | 136 (14.4%) | 146 (14.6%) |
| Patients receiving FGA-LAIs, n (%) | 113 (12.4%) | 119 (12.4%) | 158 (15.6%) | 162 (15.5%) | 131 (13.8%) | 129 (12.9%) |
| Patients receiving SGA-LAIs, n (%) | 2 (0.2%) | 6 (0.6%) | 9 (0.9%) | 5 (0.5%) | 5 (0.6%) | 17 (1.7%) |
| Year | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| Number of patients discharged | n = 1070 | n = 1029 | n = 1097 | n = 1043 | n = 1062 | n = 986 |
| Patients receiving LAIs, n (%) | 173 (16.2%) | 144 (14.0%) | 188 (17.1%) | 160 (15.3%) | 190 (17.9%) | 212 (21.5%) |
| Patients receiving FGA-LAIs, n (%) | 138 (12.9%) | 113 (11.0%) | 147 (13.4%) | 111 (10.6%) | 113 (10.6%) | 115 (11.7%) |
| Patients receiving SGA-LAIs, n (%) | 35 (3.3%) | 31 (3.0%) | 41 (3.7%) | 49 (4.7%) | 77 (7.1%) | 97 (9.8%) |
| Year . | 2006 . | 2007 . | 2008 . | 2009 . | 2010 . | 2011 . |
|---|---|---|---|---|---|---|
| Number of patients discharged . | n = 911 . | n = 963 . | n = 1011 . | n = 1047 . | n = 947 . | n = 1003 . |
| Patients receiving LAIs, n (%) | 115 (12.6%) | 125 (13.0%) | 167 (16.5%) | 167 (16.0%) | 136 (14.4%) | 146 (14.6%) |
| Patients receiving FGA-LAIs, n (%) | 113 (12.4%) | 119 (12.4%) | 158 (15.6%) | 162 (15.5%) | 131 (13.8%) | 129 (12.9%) |
| Patients receiving SGA-LAIs, n (%) | 2 (0.2%) | 6 (0.6%) | 9 (0.9%) | 5 (0.5%) | 5 (0.6%) | 17 (1.7%) |
| Year | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| Number of patients discharged | n = 1070 | n = 1029 | n = 1097 | n = 1043 | n = 1062 | n = 986 |
| Patients receiving LAIs, n (%) | 173 (16.2%) | 144 (14.0%) | 188 (17.1%) | 160 (15.3%) | 190 (17.9%) | 212 (21.5%) |
| Patients receiving FGA-LAIs, n (%) | 138 (12.9%) | 113 (11.0%) | 147 (13.4%) | 111 (10.6%) | 113 (10.6%) | 115 (11.7%) |
| Patients receiving SGA-LAIs, n (%) | 35 (3.3%) | 31 (3.0%) | 41 (3.7%) | 49 (4.7%) | 77 (7.1%) | 97 (9.8%) |
Abbreviations: FGA = first-generation antipsychotics; SGA = second-generation antipsychotics.
Discussion
The main finding of this study was that though patients receiving LAIs at discharge were more likely to be hospitalized involuntarily and had a shorter hospital stay during index hospitalization, they had a more favorable outcome when it came to rehospitalization. Compared with those in the oral antipsychotics group, patients in the LAIs group had a significantly lower rehospitalization rate and a significantly lengthened time between discharge and rehospitalization. This finding was in accordance with 2 Finnish nationwide cohort studies that also found LAIs to be associated with a significantly reduced risk of rehospitalization (Tiihonen et al., 2011; Taipale et al., 2018). However, with respect to discontinuation rate and time to discontinuation, no statistically significant difference was found between patients receiving LAIs and oral antipsychotics in this study. These results were consistent with the findings of Leucht and colleagues (Leucht et al., 2011).
Another finding was that comparable rehospitalization rates, time to rehospitalization, discontinuation rates, and time to discontinuation were seen in patients on FGA-LAIs and patients on SGA-LAIs (risperidone-LAI was the only available SGA-LAIs in the study). These findings were in keeping with those of a nationwide, retrospective inception cohort study that concluded risperidone-LAI was not superior to FGA-LAIs regarding time to psychiatric hospitalization and treatment discontinuation (Nielsen et al., 2015). However, compared with FGA-LAIs patients, fewer SGA-LAIs patients received concomitant anticholinergic agents. Also the prescription rate of LAIs increased over time during the study period and the contribution mainly from the increasing of SGA-LAIs prescription.
Nonadherence is one of the reasons for discontinuation (Nielsen et al., 2015). At first glance, this study’s results would seem to imply that patients in the LAIs group and the oral antipsychotics group had comparable adherence to treatment, as no significant difference in discontinuation rate and time to discontinuation between the 2 groups was seen. However, this result could have been confounded by the fact patients with poor adherence were more likely to receive LAIs (Olivares et al., 2011).
Generally, involuntarily hospitalized patients lack insight into their illness and the need for treatment (McEvoy et al., 1989). LAIs have been recommended in involuntary hospitalization to achieve the goal of improving treatment adherence (Stip et al., 2011) and avoiding future deterioration (Vaughan et al., 2000). Compared with oral antipsychotics, LAIs were associated with better medication adherence, fewer crisis referrals, and fewer relapses in patients with schizophrenia during involuntary outpatient treatment (Swartz et al., 2001; Muirhead et al., 2006; Hung et al., 2017). In the present study, time to rehospitalization was significantly longer in involuntarily hospitalized patients receiving LAIs (28.8% = 203/705, mean time ± SE = 263.9 ± 9.5 days) than those receiving oral antipsychotics (71.2% = 502/705, mean time ± SE = 222.6 ± 6.9 days) (log rank test = 6.99, df = 1, P = .008; median time to rehospitalization was not reached for the LAIs group).
In this study, SGA-LAIs were not superior to FGA-LAIs in reducing rehospitalization risk. However, compared with SGA-LAIs patients, those on FGA-LAIs were prescribed concomitant anticholinergic agents more often. Anticholinergic agents are generally used to treat extrapyramidal symptoms. It may indicate that SGA-LAIs cause fewer extrapyramidal symptoms than FGA-LAIs (Miyamoto et al., 2002).
Compared with the LAIs utilization rates in some industrialized countries, for example, 21.5% in Belgium (Hanssens et al., 2006), 23.3% in New Zealand (Humberstone et al., 2004), and 29% in the United Kingdom (Paton et al., 2003), LAIs (prescription rate = 15.8%) may have been underutilized in our hospital. This may be due to unfamiliarity with LAIs and inaccurate perceptions about safety and efficacy among psychiatrists, cost and accessibility of treatment, and negative perceptions of injections among patients and caregivers (Correll et al., 2016). The increase in LAIs use over time in this study can probably be explained by better education and psychiatrists’ growing amount of positive experiences with LAIs (Liu et al., 2018). Furthermore, the LAIs prescription rates increased over the study period are mainly from the increasing of SGA-LAIs prescription rather than FGA-LAIs. Another possible reason is that the safety and effectiveness of SGA is more acceptable by patients with schizophrenia and psychiatrists than FGA (Chan et al., 2010a, 2010b, 2018). Additionally, the increasing number of studies showing their efficacy and safety may also contribute to the continuous rise in the use of LAIs (Olivares et al., 2011). As a result, psychiatrists may hold a more favorable attitude towards prescribing LAIs than before.
Certain limitations should be considered when interpreting the results of this study. First, this was an observational retrospective study that did not include measurements of symptom severity, side effects, quality of life, medication adherence, or drug attitude. However, observational retrospective studies often allow better assessment of effectiveness under real-life conditions, as they are carried out in more naturalistic treatment settings. Second, SGA-LAIs that were unavailable for use during the study period were not included. Third, since not all clinically significant exacerbations lead to hospitalization, use of rehospitalization as an indicator of relapse may provide only a limited view on differences in the outcomes associated with use of LAIs vs oral antipsychotics (Marcus et al., 2015). Fourth, treatment allocation was not random to the 2 groups as the patients in the LAIs group may have been preselected. Fifth, owing to lack of data, some covariates that may be associated with rehospitalization risk were not adjusted for, and reasons for discontinuation were not explored. Finally, this is a single-center study from Taiwan and therefore may have limited generalizability to other facilities and countries.
Conclusions
In this study, LAIs were found to be superior to oral antipsychotics in reducing the risk of rehospitalization. Fewer patients in the SGA-LAIs group received concomitant anticholinergic agents than the FGA-LAIs group. However, SGA-LAIs were not superior to FGA-LAIs in reducing the risk of rehospitalization. A continuous increase in LAIs prescription rate can probably be explained by growing experiences and success of clinicians in treating patients with LAIs. More studies comparing the effectiveness of LAIs with random assignment, including FGA-LAIs and SGA-LAIs, and oral antipsychotics are warranted before a conclusion can be made.
Acknowledgments
This work was supported by the Ministry of Health and Welfare, Taiwan (MOHW-107–47).
Statement of Interest
None.



