-
PDF
- Split View
-
Views
-
Cite
Cite
Corstiaan A. den Uil, Suzanne D.A. Valk, Jin M. Cheng, Arie P. Kappetein, Ad J.J.C. Bogers, Ron T. van Domburg, Maarten L. Simoons, Prognosis of patients undergoing cardiac surgery and treated with intra-aortic balloon pump counterpulsation prior to surgery: a long-term follow-up study, Interactive CardioVascular and Thoracic Surgery, Volume 9, Issue 2, August 2009, Pages 227–231, https://doi.org/10.1510/icvts.2009.207027
Close - Share Icon Share
Abstract
The aim of this study was to evaluate short- and long-term outcome in patients undergoing coronary artery bypass grafting (CABG), who received an intra-aortic balloon pump (IABP) prior to surgery. Between January 1990 and June 2004, all patients (n=154) who received an IABP prior to on-pump CABG in our center were included. Patients received the IABP for vital indications (i.e. either unstable angina refractory to medical therapy or cardiogenic shock; group 1: n=99) or for prophylactic reasons (group 2: n=55). A Cox proportional hazards model was used to identify predictors of long-term all-cause mortality. Compared with the EuroSCORE predictive model, observed 30-day mortality in group 1 (15.2%) was slightly higher than predicted (10.3%). A decrease in 30-day mortality occurred in group 2 (median predicted mortality was 7.2% and observed was 0%). Cumulative 1-, 5-, and 6-year survival was 82.8±3.8%, 70.1±4.9%, and 67.3±5.1% for group 1 vs. 98.2±1.8%, 84.0±5.6% and 84.0±5.6% for group 2 (Log-rank: P=0.02). Logistic EuroSCORE (HR 1.03 [1.01–1.05], P=0.007) was an independent predictor of long-term all-cause mortality.
1. Introduction
The main effects of intra-aortic balloon pump (IABP) counterpulsation are reduction of ventricular afterload, improvement in coronary perfusion, and enhancement of subendocardial perfusion [1]. Several studies have supported insertion of an IABP prior to high-risk cardiac surgery [2–4]. In addition, preoperative insertion has been associated with lower in-hospital mortality rates compared to intra-operative or postoperative insertion [5]. However, data are lacking on long-term prognosis of patients undergoing high-risk coronary artery bypass grafting (CABG), who were treated with IABP assist preoperatively. We performed a cohort study to address short- and long-term mortality in these patients.
2. Materials and methods
2.1. Patient inclusion and data collection
Between January 1990 and June 2004, all patients (n= 154) who received an IABP prior to CABG in our center were included. Data were acquired from patient medical records and from the local hospital database. Retrospectively, the logistic European system for cardiac operative risk evaluation (EuroSCORE) was calculated for each patient [6]. A priori, we made the decision to analyze the data separately dependent on the indication for IABP counterpulsation. Ninety-nine patients (64%) received an IABP for vital indications (cardiogenic shock or unstable angina refractory to pharmacological therapy; group 1). The remaining 55 patients (36%) received the IABP for prophylactic reasons (LVEF below 40%, redo surgery, or complex coronary artery lesions; group 2).
2.2. IABP
All IABPs were inserted at the catheterization laboratory or intensive cardiac care unit. In all patients, the IABP was introduced using the Seldinger technique. Between 1990 and 1995, Datascope (datascope Corp, Fairfield, NJ, USA) 10.5 and 9.5 French catheters were used. From 1995 through 2000, Arrow (Arrow Corp, Reading, PA, USA) 9 French catheters, and between 2000 and 2004, Arrow (Arrow Corp, Reading, PA, USA) 8 French catheters were used.
2.3. Study definitions
Left ventricular function was estimated with echocardiography performed by trained cardiologists. Impaired left ventricular function was defined as an ejection fraction <40% measured by echocardiography. Cardiogenic shock was defined as systolic blood pressure below 90 mmHg with clinical signs of hypoperfusion, i.e. cold extremities, oliguria or altered mental state. Inotropic agents used were catecholamines (dobutamine, dopamine, and/or norepinephrine) and phosphodiesterase inhibitors (enoximone). The following complications of IABP counterpulsation were registered: leg ischemia requiring IABP removal, IABP-related femoral artery thrombosis, need for vascular surgery, infection, and access site bleeding requiring blood transfusion. Leg ischemia was defined as a novel absence of peripheral pulsations together with a white coloration of the leg.
2.4. Management of surgery
In all patients, non-pulsatile cardiopulmonary bypass was established through standard median sternotomy with aortic root and right atrial cannulation. Surgery was performed under mild hypothermia (32 °C).
2.5. Follow-up
Follow-up started at the day of surgery (baseline). In 2005, vital status of all patients was acquired from the Registry of Deaths. Median follow-up duration was 5.7 years (range: 0–6 years). Follow-up duration was cut-off at six years, because, after six years, the number of patients at risk decreased significantly and the risk estimates became unstable.
2.6. Statistical analysis
Continuous variables were expressed as mean±S.D. Non-normally distributed variables were presented as median and interquartile range. Discrete variables were noted as numbers and proportions. Differences between groups were tested with one-way analysis of variance (ANOVA), Mann–Whitney, or χ2-test, when appropriate. Cumulative incidence of survival was determined by Kaplan–Meier analysis with survival expressed as calculated probability±standard error. Kaplan–Meier survival curves were compared by the log-rank test. The Cox proportional hazards model was used to identify predictors of long-term all-cause mortality. Multivariate Cox proportional hazards model analysis was done by entering the clinical characteristics that were significantly different between both groups and that showed the best correlation with long-term mortality in univariate analysis. Hazard ratios (HR) were presented together with their 95% confidence intervals. A two-tailed P-value <0.05 was considered statistically significant.
3. Results
3.1. Clinical characteristics of the study population
Between January 1990 and June 2004, 154 consecutive patients were included in this study. Table 1 demonstrates the clinical characteristics of the patients, divided into indication for IABP therapy (group 1: ‘vital indication’; group 2: ‘prophylactic’ reasons). Mean age of the patients was 64±9 years in group 1 and 66±8 years in group 2. Seventy-six percent of them were male. In 26 cases (17%), CABG was combined with surgery for other sequelae of coronary obstruction. Logistic EuroSCORE was significantly higher in group 1 relative to group 2 (10.3 [4.7–18.8]% vs. 7.2 [3.8–10.3]% in group 2, P=0.002).
| Group 1 | Group 2 | P-value | |
| ‘Vital indication’ | ‘Prophylactic’ | ||
| n=99 | n=55 | ||
| Age, years (mean±S.D.) | 64±9 | 66±8 | 0.18 |
| Gender, male | 75 (76%) | 42 (76%) | 0.99 |
| Logistic EuroSCORE, % (median and IQR) | 10.3 [4.7–18.8] | 7.2 [3.8–10.3] | 0.002 |
| Preoperative CV risk factors | |||
| Hypertension | 37 (37%) | 29 (53%) | 0.09 |
| Current smoking | 36 (36%) | 13 (24%) | 0.15 |
| Dyslipidemia | 42 (42%) | 26 (47%) | 0.61 |
| Diabetes mellitus | 27 (27%) | 13 (24%) | 0.70 |
| History | |||
| Previous MI | 67 (68%) | 36 (69%) | 0.99 |
| Prior CABG | 17 (17%) | 8 (15%) | 0.82 |
| Impaired LV function (EF<40%) | 39 (39%) | 16 (29%) | 0.22 |
| Clinical parameters | |||
| Body mass index, kg/m2 (mean±S.D.) | 26±3 | 26±3 | 0.75 |
| Heart rate, bpm (mean±S.D.) | 84±22 | 78±15 | 0.08 |
| Diagnosis | |||
| Acute myocardial infarction | 55 (56%) | 19 (35%) | 0.02 |
| Mechanical complication of (A)MI | 12 (12%) | 0 (0%) | 0.005 |
| Cardiac angiography | |||
| Three-vessel coronary disease or left main stem | 65 (66%) | 46 (84%) | 0.02 |
| stenosis >70% | |||
| Preoperative treatment | |||
| Inotropic agents for cardiogenic shock | 20 (20%) | 0 (0%) | <0.001 |
| Type of surgery | |||
| Isolated CABG procedure | 76 (77%) | 52 (95%) | 0.006 |
| CABG plus mitral valve surgery | 17 (18%) | 2 (4%) | 0.01 |
| CABG plus LV reconstruction | 2 (2%) | 2 (4%) | 0.62 |
| CABG plus VSR repair | 5 (5%) | 0 (0%) | 0.16 |
| Anastomoses | |||
| >3 anastomoses | 50 (53%) | 42 (79%) | 0.001 |
| Complications from IABP counterpulsation | |||
| Leg ischemia requiring IABP removal | 2 (2%) | 3 (6%) | 0.35 |
| Arterial thrombosis requiring vascular surgery | 1 (1%) | 2 (4%) | 0.29 |
| Thrombocytopenia | 1 (1%) | 0 (0%) | 0.99 |
| Group 1 | Group 2 | P-value | |
| ‘Vital indication’ | ‘Prophylactic’ | ||
| n=99 | n=55 | ||
| Age, years (mean±S.D.) | 64±9 | 66±8 | 0.18 |
| Gender, male | 75 (76%) | 42 (76%) | 0.99 |
| Logistic EuroSCORE, % (median and IQR) | 10.3 [4.7–18.8] | 7.2 [3.8–10.3] | 0.002 |
| Preoperative CV risk factors | |||
| Hypertension | 37 (37%) | 29 (53%) | 0.09 |
| Current smoking | 36 (36%) | 13 (24%) | 0.15 |
| Dyslipidemia | 42 (42%) | 26 (47%) | 0.61 |
| Diabetes mellitus | 27 (27%) | 13 (24%) | 0.70 |
| History | |||
| Previous MI | 67 (68%) | 36 (69%) | 0.99 |
| Prior CABG | 17 (17%) | 8 (15%) | 0.82 |
| Impaired LV function (EF<40%) | 39 (39%) | 16 (29%) | 0.22 |
| Clinical parameters | |||
| Body mass index, kg/m2 (mean±S.D.) | 26±3 | 26±3 | 0.75 |
| Heart rate, bpm (mean±S.D.) | 84±22 | 78±15 | 0.08 |
| Diagnosis | |||
| Acute myocardial infarction | 55 (56%) | 19 (35%) | 0.02 |
| Mechanical complication of (A)MI | 12 (12%) | 0 (0%) | 0.005 |
| Cardiac angiography | |||
| Three-vessel coronary disease or left main stem | 65 (66%) | 46 (84%) | 0.02 |
| stenosis >70% | |||
| Preoperative treatment | |||
| Inotropic agents for cardiogenic shock | 20 (20%) | 0 (0%) | <0.001 |
| Type of surgery | |||
| Isolated CABG procedure | 76 (77%) | 52 (95%) | 0.006 |
| CABG plus mitral valve surgery | 17 (18%) | 2 (4%) | 0.01 |
| CABG plus LV reconstruction | 2 (2%) | 2 (4%) | 0.62 |
| CABG plus VSR repair | 5 (5%) | 0 (0%) | 0.16 |
| Anastomoses | |||
| >3 anastomoses | 50 (53%) | 42 (79%) | 0.001 |
| Complications from IABP counterpulsation | |||
| Leg ischemia requiring IABP removal | 2 (2%) | 3 (6%) | 0.35 |
| Arterial thrombosis requiring vascular surgery | 1 (1%) | 2 (4%) | 0.29 |
| Thrombocytopenia | 1 (1%) | 0 (0%) | 0.99 |
Data represent numbers (%) unless otherwise indicated.
S.D., standard deviation; EuroSCORE, European system for cardiac operative risk evaluation; IQR, interquartile range; CV, cardiovascular; (A)MI, acute myocardial infarction; CABG, coronary artery bypass grafting; LV, left ventricular; EF, ejection fraction, VSR, ventricular septal rupture.
| Group 1 | Group 2 | P-value | |
| ‘Vital indication’ | ‘Prophylactic’ | ||
| n=99 | n=55 | ||
| Age, years (mean±S.D.) | 64±9 | 66±8 | 0.18 |
| Gender, male | 75 (76%) | 42 (76%) | 0.99 |
| Logistic EuroSCORE, % (median and IQR) | 10.3 [4.7–18.8] | 7.2 [3.8–10.3] | 0.002 |
| Preoperative CV risk factors | |||
| Hypertension | 37 (37%) | 29 (53%) | 0.09 |
| Current smoking | 36 (36%) | 13 (24%) | 0.15 |
| Dyslipidemia | 42 (42%) | 26 (47%) | 0.61 |
| Diabetes mellitus | 27 (27%) | 13 (24%) | 0.70 |
| History | |||
| Previous MI | 67 (68%) | 36 (69%) | 0.99 |
| Prior CABG | 17 (17%) | 8 (15%) | 0.82 |
| Impaired LV function (EF<40%) | 39 (39%) | 16 (29%) | 0.22 |
| Clinical parameters | |||
| Body mass index, kg/m2 (mean±S.D.) | 26±3 | 26±3 | 0.75 |
| Heart rate, bpm (mean±S.D.) | 84±22 | 78±15 | 0.08 |
| Diagnosis | |||
| Acute myocardial infarction | 55 (56%) | 19 (35%) | 0.02 |
| Mechanical complication of (A)MI | 12 (12%) | 0 (0%) | 0.005 |
| Cardiac angiography | |||
| Three-vessel coronary disease or left main stem | 65 (66%) | 46 (84%) | 0.02 |
| stenosis >70% | |||
| Preoperative treatment | |||
| Inotropic agents for cardiogenic shock | 20 (20%) | 0 (0%) | <0.001 |
| Type of surgery | |||
| Isolated CABG procedure | 76 (77%) | 52 (95%) | 0.006 |
| CABG plus mitral valve surgery | 17 (18%) | 2 (4%) | 0.01 |
| CABG plus LV reconstruction | 2 (2%) | 2 (4%) | 0.62 |
| CABG plus VSR repair | 5 (5%) | 0 (0%) | 0.16 |
| Anastomoses | |||
| >3 anastomoses | 50 (53%) | 42 (79%) | 0.001 |
| Complications from IABP counterpulsation | |||
| Leg ischemia requiring IABP removal | 2 (2%) | 3 (6%) | 0.35 |
| Arterial thrombosis requiring vascular surgery | 1 (1%) | 2 (4%) | 0.29 |
| Thrombocytopenia | 1 (1%) | 0 (0%) | 0.99 |
| Group 1 | Group 2 | P-value | |
| ‘Vital indication’ | ‘Prophylactic’ | ||
| n=99 | n=55 | ||
| Age, years (mean±S.D.) | 64±9 | 66±8 | 0.18 |
| Gender, male | 75 (76%) | 42 (76%) | 0.99 |
| Logistic EuroSCORE, % (median and IQR) | 10.3 [4.7–18.8] | 7.2 [3.8–10.3] | 0.002 |
| Preoperative CV risk factors | |||
| Hypertension | 37 (37%) | 29 (53%) | 0.09 |
| Current smoking | 36 (36%) | 13 (24%) | 0.15 |
| Dyslipidemia | 42 (42%) | 26 (47%) | 0.61 |
| Diabetes mellitus | 27 (27%) | 13 (24%) | 0.70 |
| History | |||
| Previous MI | 67 (68%) | 36 (69%) | 0.99 |
| Prior CABG | 17 (17%) | 8 (15%) | 0.82 |
| Impaired LV function (EF<40%) | 39 (39%) | 16 (29%) | 0.22 |
| Clinical parameters | |||
| Body mass index, kg/m2 (mean±S.D.) | 26±3 | 26±3 | 0.75 |
| Heart rate, bpm (mean±S.D.) | 84±22 | 78±15 | 0.08 |
| Diagnosis | |||
| Acute myocardial infarction | 55 (56%) | 19 (35%) | 0.02 |
| Mechanical complication of (A)MI | 12 (12%) | 0 (0%) | 0.005 |
| Cardiac angiography | |||
| Three-vessel coronary disease or left main stem | 65 (66%) | 46 (84%) | 0.02 |
| stenosis >70% | |||
| Preoperative treatment | |||
| Inotropic agents for cardiogenic shock | 20 (20%) | 0 (0%) | <0.001 |
| Type of surgery | |||
| Isolated CABG procedure | 76 (77%) | 52 (95%) | 0.006 |
| CABG plus mitral valve surgery | 17 (18%) | 2 (4%) | 0.01 |
| CABG plus LV reconstruction | 2 (2%) | 2 (4%) | 0.62 |
| CABG plus VSR repair | 5 (5%) | 0 (0%) | 0.16 |
| Anastomoses | |||
| >3 anastomoses | 50 (53%) | 42 (79%) | 0.001 |
| Complications from IABP counterpulsation | |||
| Leg ischemia requiring IABP removal | 2 (2%) | 3 (6%) | 0.35 |
| Arterial thrombosis requiring vascular surgery | 1 (1%) | 2 (4%) | 0.29 |
| Thrombocytopenia | 1 (1%) | 0 (0%) | 0.99 |
Data represent numbers (%) unless otherwise indicated.
S.D., standard deviation; EuroSCORE, European system for cardiac operative risk evaluation; IQR, interquartile range; CV, cardiovascular; (A)MI, acute myocardial infarction; CABG, coronary artery bypass grafting; LV, left ventricular; EF, ejection fraction, VSR, ventricular septal rupture.
3.2. Thirty-day outcome
Fifteen patients (15.2%) in group 1 and no patients (0.0%) in group 2 died in the 30 days following surgery (group 1 vs. group 2: P=0.001). Observed mortality in group 1 was slightly higher than predicted by EuroSCORE (Fig. 1 ). However, a decrease in mortality occurred in group 2: median predicted mortality was 7.2% and observed was 0% (Fig. 1).
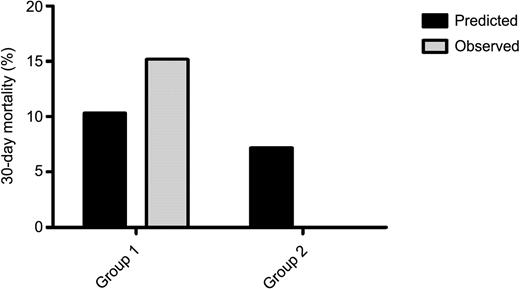
Short-term prognosis. Observed mortality (light gray) compared with mortality predicted by the European System for Cardiac Operative Risk Evaluation (EuroSCORE; black). Group 1: ‘vital indication’, group 2: ‘prophylactic indication’ for intra-aortic balloon pump counterpulsation.
3.3. Long-term outcome
After six years of follow-up, 3% of the patients were lost. The endpoint (all-cause mortality) occurred in 29 (29%) patients in group 1 and in 7 (13%) patients in group 2. Kaplan–Meier estimated 6-year survival was 67.3±5.1% for group 1 and 84.0±5.6% for group 2, P=0.02 (Fig. 2 ). Logistic EuroSCORE (HR 1.03 [1.01–1.05], P=0.007) was the best independent predictor of long-term all-cause mortality (Table 2 ).
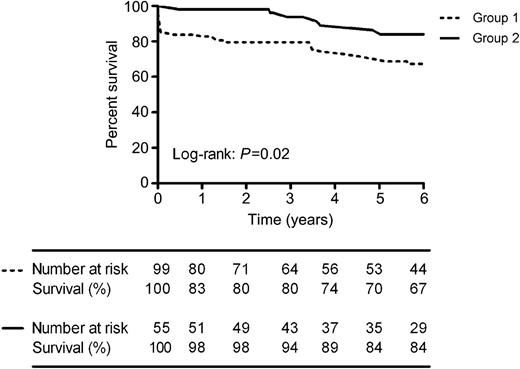
Kaplan–Meier plot of long-term survival. Long-term survival of the study population stratified to the indication for intra-aortic balloon pump counterpulsation (group 1: ‘vital indication’, group 2: ‘prophylactic indication’).
| Univariate | P-value | Multivariate | P-value | |
| HR [95% CI] | HR [95% CI] | |||
| Age, years | 0.99 [0.96–1.03] | 0.65 | 1.00 [0.96–1.04] | 0.98 |
| Gender, male | 1.47 [0.64–3.36] | 0.36 | 1.51 [0.62–3.66] | 0.37 |
| Logistic EuroSCORE, % | 1.05 [1.03–1.06] | <0.001 | 1.03 [1.01–1.05] | 0.007 |
| Inotropic agents for cardiogenic shock | 3.46 [1.66–7.18] | 0.001 | 1.17 [0.46–2.97] | 0.74 |
| CABG plus other type of surgery | 3.55 [1.80–7.02] | <0.001 | 2.30 [0.97–5.49] | 0.06 |
| Indication of IABP (‘prophylactic’ | 0.38 [0.17–0.87] | 0.02 | 0.58 [0.24–1.41] | 0.23 |
| relative to ‘vital indication’) |
| Univariate | P-value | Multivariate | P-value | |
| HR [95% CI] | HR [95% CI] | |||
| Age, years | 0.99 [0.96–1.03] | 0.65 | 1.00 [0.96–1.04] | 0.98 |
| Gender, male | 1.47 [0.64–3.36] | 0.36 | 1.51 [0.62–3.66] | 0.37 |
| Logistic EuroSCORE, % | 1.05 [1.03–1.06] | <0.001 | 1.03 [1.01–1.05] | 0.007 |
| Inotropic agents for cardiogenic shock | 3.46 [1.66–7.18] | 0.001 | 1.17 [0.46–2.97] | 0.74 |
| CABG plus other type of surgery | 3.55 [1.80–7.02] | <0.001 | 2.30 [0.97–5.49] | 0.06 |
| Indication of IABP (‘prophylactic’ | 0.38 [0.17–0.87] | 0.02 | 0.58 [0.24–1.41] | 0.23 |
| relative to ‘vital indication’) |
HR, hazard ratio; EuroSCORE, European system for cardiac operative risk evaluation; CABG, coronary artery bypass grafting.
| Univariate | P-value | Multivariate | P-value | |
| HR [95% CI] | HR [95% CI] | |||
| Age, years | 0.99 [0.96–1.03] | 0.65 | 1.00 [0.96–1.04] | 0.98 |
| Gender, male | 1.47 [0.64–3.36] | 0.36 | 1.51 [0.62–3.66] | 0.37 |
| Logistic EuroSCORE, % | 1.05 [1.03–1.06] | <0.001 | 1.03 [1.01–1.05] | 0.007 |
| Inotropic agents for cardiogenic shock | 3.46 [1.66–7.18] | 0.001 | 1.17 [0.46–2.97] | 0.74 |
| CABG plus other type of surgery | 3.55 [1.80–7.02] | <0.001 | 2.30 [0.97–5.49] | 0.06 |
| Indication of IABP (‘prophylactic’ | 0.38 [0.17–0.87] | 0.02 | 0.58 [0.24–1.41] | 0.23 |
| relative to ‘vital indication’) |
| Univariate | P-value | Multivariate | P-value | |
| HR [95% CI] | HR [95% CI] | |||
| Age, years | 0.99 [0.96–1.03] | 0.65 | 1.00 [0.96–1.04] | 0.98 |
| Gender, male | 1.47 [0.64–3.36] | 0.36 | 1.51 [0.62–3.66] | 0.37 |
| Logistic EuroSCORE, % | 1.05 [1.03–1.06] | <0.001 | 1.03 [1.01–1.05] | 0.007 |
| Inotropic agents for cardiogenic shock | 3.46 [1.66–7.18] | 0.001 | 1.17 [0.46–2.97] | 0.74 |
| CABG plus other type of surgery | 3.55 [1.80–7.02] | <0.001 | 2.30 [0.97–5.49] | 0.06 |
| Indication of IABP (‘prophylactic’ | 0.38 [0.17–0.87] | 0.02 | 0.58 [0.24–1.41] | 0.23 |
| relative to ‘vital indication’) |
HR, hazard ratio; EuroSCORE, European system for cardiac operative risk evaluation; CABG, coronary artery bypass grafting.
3.4. Complications of IABP counterpulsation
Overall, six patients (3.9%) developed IABP-related complications. Complications occurred in both groups of patients (Table 1). Five patients (3%) had symptoms of leg ischemia at the side where the IABP was inserted. In two of these cases, IABP removal before initiation of surgery was necessary. The other three patients (2%) developed signs of leg ischemia after postoperative removal of the IABP. This was due to common femoral artery thrombosis, requiring vascular surgery. In two patients, embolectomy was performed and in the third patient a iliaco-femoro-popliteal Goretex bypass was made. These three cases of arterial thrombosis following IABP occurred in the time period 1991–1994. Finally, one patient experienced an episode of thrombocytopenia (lowest thrombocyte count 43*109/l) without signs of hemorrhage. There were no IABP-related access site bleedings requiring red blood cell transfusion. If performed, IABP tip cultures were all negative. All six patients with complications survived the first 30 days following surgery.
4. Discussion
This is the first study reporting long-term outcome of a unique group of patients who underwent CABG with the use of preoperative IABP, reflecting a 15-year experience in our center. Compared with the EuroSCORE predictive model, we demonstrated that prophylactic IABP counterpulsation allowed a reduction in 30-day mortality. In both groups, a considerable number of patients survived until six years of follow-up following surgery. Logistic EuroSCORE, used as a continuous variable, was an independent predictor of long-term outcome.
Several studies suggested that preoperative introduction of an IABP may have beneficial effects on mortality in specific patient groups undergoing CABG [4,7]. The low short-term event rate in our subgroup of patients treated prophylactically with IABP, suggests a beneficial effect of counterpulsation as well. Data on long-term survival of patients treated with preoperative IABP are still lacking in the current literature. In our study, consisting of a considerable number of high-risk patiens, we found that 5-year survival was 70% in unstable patients and 84% in patients treated prophylactically with IABP. Based on large databases of isolated, mainly low risk, CABG patients, recent studies have reported a 5-year probability of survival of approximately 80–90% [8,9], which suggests that long-term survival in our study population was relatively favorable. Notably, the difference in long-term survival rates between group 1 and group 2 was determined by the high 30-day mortality rate in group 1, since the Kaplan–Meier curves ran parallel after 30 days of follow-up. Interestingly, Singh et al. reported recently that among survivors of STEMI complicated by cardiogenic shock, annual long-term mortality rates approximate those of STEMI patients without shock [10]. Our findings point out a similar principle in a different cohort of patients.
We used the logistic EuroSCORE, which is known to be more accurate in relatively high-risk patients than the simple additive EuroSCORE model [11]. Other investigators have demonstrated the predictive value of the additive EuroSCORE model as well as the logistic EuroSCORE model for long-term all-cause mortality [12,13]. We confirmed the independent association of logistic EuroSCORE and long-term outcome in patients treated with preoperative IABP.
Overall IABP-related complication rate was 3.9%, which is in line with other reports [4,14]. The complications included arterial thrombosis, occurring in the years that larger catheters were used than nowadays. No IABP-related deaths occurred, indicating a specific area of indication for these devices before moving on to more powerful left ventricular assist devices with a higher mortality [15].
Our study has its limitations. First, we investigated a relatively small number of heterogeneous patients. However, we divided our population into two groups of unstable patients, who had a vital indication for IABP therapy and patients who were treated prophylactically. A second limitation is the retrospective nature of our study. However, main data could be retrieved from surgeon's reports and discharge letters in our local computer database. The remaining missing data were all acquired from patient medical records. Third, we compared short-term mortality with logistic EuroSCORE, which may actually overestimate the operative risk.
In conclusion, a considerable number of patients undergoing on-pump cardiac surgery with preoperative IABP, survived at the long-term. Logistic EuroSCORE was an independent predictor of long-term outcome. Further improving outcome in those patients who are hemodynamically compromised prior to surgery remains a challenge for the future.




