-
PDF
- Split View
-
Views
-
Cite
Cite
Domenico Pourmolkara, Antonio Giulio Napolitano, Eleonora Coviello, Francesco Puma, Giant intrathoracic cystic schwannoma resected by video-assisted thoracoscopic surgery, Interdisciplinary CardioVascular and Thoracic Surgery, Volume 37, Issue 5, November 2023, ivad169, https://doi.org/10.1093/icvts/ivad169
Close - Share Icon Share
Abstract
Schwannoma is a benign tumour originating from the Schwann cells. Patients can remain asymptomatic, as the onset of symptoms usually depends on the compressive effect on adjacent organs; dimensional and morphological variability increase the time for the diagnosis. We report the case of a successful surgical resection, performed by video-assisted thoracoscopic surgery, on a patient with radiological evidence of a massive cystic intrathoracic neoformation, histologically revealed to be a peculiar Schwannoma.
INTRODUCTION
Schwannoma is a benign slow-growing tumour that arises from a myelinated nerve sheath. The majority of patients have been reported to be asymptomatic. Symptoms like dyspnoea, dysphagia and superior vena cava syndrome are caused by compression of adjacent structures. Schwannomas are well-encapsulated tumours with smooth surface; there may be secondary changes such as cystic degeneration, haemorrhage and calcification. Combined degenerations occur more frequently in large schwannomas and so a totally cystic giant schwannoma is extremely rare.
CASE REPORT
A 50-year-old woman was incidentally found to have a large opacity in the left haemithorax; a chest X-ray documented a large rounded opacity in the upper field of the left lung (Fig. 1A). The complete blood count, carcinoembryonic antigen, C-reactive protein and serum creatinine value were all within the reference range. A contrast computed tomography scans (Fig. 1B) revealed 86-mm paravertebral cystic tumour extending from T4–T6, filled with a low-density fluid. The lesion was adherent to the posterior mediastinum, the posterior parietal pleura and the paravertebral space, probably occupying the apicoposterior segment of the left upper lobe. The PET–CT (positron emission tomography-computed tomography (Fig. 1C) showed a low grade of FDG (fluorodeoxyglucose) uptake. The patient underwent a three-port video-assisted thoracoscopic surgery: the lesion originated from the paravertebral space and appeared to be encapsulated with well-defined edges (Fig. 1D). After careful detachment from the chest wall, being careful to clamp any vessels connected to the mass, the tumour was finally resected (Fig. 1E).
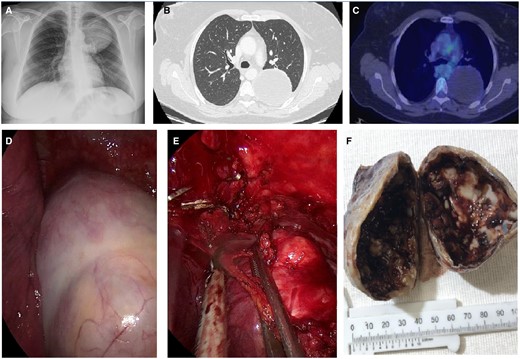
(A) Chest X-ray; (B) computed tomography; (C) FDG PET/CT; (D) tumour surface before surgical manipulation; (E) resection approach; and (F) tumour mass showing a cystic cavity partially covered with blood material.
The resected mass measured 8.5 cm × 7.5 cm × 5 cm; on cut surface, the tumour was completely cystic with an irregular and thick wall that showed haematic contents and white areas with sclerotic aspect (Fig. 1F). Immunohistochemical staining showed that tumour cells were strongly positive for S-100 protein and SOX10 and negative for cytocheratin, desmin, smooth muscle actin and CD34; the final histopathological diagnosis was benign giant cystic schwannoma.
DISCUSSION AND REVIEW OF THE LITERATURE
Several monocentric studies have been made over the last years, and one of the most recent is that of Natale et al. [1]. However, our intent was to conduct a comprehensive review of the literature to analyse this peculiar case. We searched PubMed and Embase databases for similar case reports published before December 2022. The eligibility criteria for our review are maximum diameter ≥8 cm, non-infiltration of adjacent structures (vertebrae, diaphragm, lungs, etc.) and diagnosis of cystic or partly cystic schwannoma.
To our knowledge, adding our case, 5 cases with cystic or partly cystic giant intrathoracic schwannoma arising from the intercostal nerve have been reported in literature so far. The clinical characteristics of included cases are shown in Table 1.
| Case . | Country . | Gender . | Age . | Side . | Primary symptoms . | Maximal size (cm) . | Surgical aproach . | P.A. . |
|---|---|---|---|---|---|---|---|---|
| 1 | U.S.A. | F | 52 | Right | Persistent cough | 12x15 | Thorac. | Multiple cystic mass with calcification |
| 2 | Taiwan | M | 73 | Left | Dyspnea | 17x17x5 | P-L thorac. | cystic with muddy content |
| 3 | Japan | F | 37 | Left | Back pain | 7.3x5x4.7 | L. thorac. | Necrotic and cystic |
| 4 | Romania | M | 60 | Right | Dyspnea | 20.5x12x9 | Thorac. | Partly cystic |
| 5 | Italy | F | 50 | Left | No | 8.5x7.5x5 | VATS | Full cystic |
| Case . | Country . | Gender . | Age . | Side . | Primary symptoms . | Maximal size (cm) . | Surgical aproach . | P.A. . |
|---|---|---|---|---|---|---|---|---|
| 1 | U.S.A. | F | 52 | Right | Persistent cough | 12x15 | Thorac. | Multiple cystic mass with calcification |
| 2 | Taiwan | M | 73 | Left | Dyspnea | 17x17x5 | P-L thorac. | cystic with muddy content |
| 3 | Japan | F | 37 | Left | Back pain | 7.3x5x4.7 | L. thorac. | Necrotic and cystic |
| 4 | Romania | M | 60 | Right | Dyspnea | 20.5x12x9 | Thorac. | Partly cystic |
| 5 | Italy | F | 50 | Left | No | 8.5x7.5x5 | VATS | Full cystic |
Case 1 was reported by Kraal [2]. Case 2 was reported by Chen et al [3]. Case 3 was reported by Morimoto et al. [1]. Case 4 was reported by Savu et al. [4]. Case 5 is the current patient.
Thorac., thoracotomy; P-L, postero-lateral; L, lateral; VATS, Video Assisted Thoracoscopic Surgery.
| Case . | Country . | Gender . | Age . | Side . | Primary symptoms . | Maximal size (cm) . | Surgical aproach . | P.A. . |
|---|---|---|---|---|---|---|---|---|
| 1 | U.S.A. | F | 52 | Right | Persistent cough | 12x15 | Thorac. | Multiple cystic mass with calcification |
| 2 | Taiwan | M | 73 | Left | Dyspnea | 17x17x5 | P-L thorac. | cystic with muddy content |
| 3 | Japan | F | 37 | Left | Back pain | 7.3x5x4.7 | L. thorac. | Necrotic and cystic |
| 4 | Romania | M | 60 | Right | Dyspnea | 20.5x12x9 | Thorac. | Partly cystic |
| 5 | Italy | F | 50 | Left | No | 8.5x7.5x5 | VATS | Full cystic |
| Case . | Country . | Gender . | Age . | Side . | Primary symptoms . | Maximal size (cm) . | Surgical aproach . | P.A. . |
|---|---|---|---|---|---|---|---|---|
| 1 | U.S.A. | F | 52 | Right | Persistent cough | 12x15 | Thorac. | Multiple cystic mass with calcification |
| 2 | Taiwan | M | 73 | Left | Dyspnea | 17x17x5 | P-L thorac. | cystic with muddy content |
| 3 | Japan | F | 37 | Left | Back pain | 7.3x5x4.7 | L. thorac. | Necrotic and cystic |
| 4 | Romania | M | 60 | Right | Dyspnea | 20.5x12x9 | Thorac. | Partly cystic |
| 5 | Italy | F | 50 | Left | No | 8.5x7.5x5 | VATS | Full cystic |
Case 1 was reported by Kraal [2]. Case 2 was reported by Chen et al [3]. Case 3 was reported by Morimoto et al. [1]. Case 4 was reported by Savu et al. [4]. Case 5 is the current patient.
Thorac., thoracotomy; P-L, postero-lateral; L, lateral; VATS, Video Assisted Thoracoscopic Surgery.
Pathological examinations revealed a cystic degeneration of these schwannomas: multiple cystic mass with calcification [2], cystic with muddy content [3], necrotic and cystic [4], partly cystic [5] and, in our case, a full cystic variant of the tumour; our case is also the only case resected by video-assisted thoracoscopic surgery technique.
CONCLUSION
Giant cystic schwannoma is a rare benign tumour that should be adequately considered a differential diagnosis when investigating patients with solitary and radiographically well-defined mass of the thorax. Most patients are not experiencing any symptoms.
Although the prognosis for these patients is good, there is a minimum percentage of patients in which there can be a malignant evolution of the tumour.
Funding
This study received no grants from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: The authors have no conflicts of interest.
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author, Domenico Pourmolkara, upon reasonable request.
Reviewer information
Interdisciplinary CardioVascular and Thoracic Surgery thanks Sara Ricciardi, Olgun Kadir ARIBAŞ and the other anonymous reviewer(s) for their contribution to the peer review process of this article.




