-
PDF
- Split View
-
Views
-
Cite
Cite
Jorge O Barretta, Sofía Grinenco, Juan M Osuna, Natalia S Napoli, Novel use of reverse double switch operation in failed left ventricular recruitment pathway, Interactive CardioVascular and Thoracic Surgery, Volume 35, Issue 3, September 2022, ivac173, https://doi.org/10.1093/icvts/ivac173
Close - Share Icon Share
Abstract
In spite of great advances in staged left ventricle recruitment strategy, some patients do not achieve biventricular circulation nor are candidates for reversal to single-ventricle palliation. We present a case of a successful reverse double switch operation in a patient with failure of left ventricle recruitment and pulmonary hypertension. This strategy provided a one-and-a-half repair with a sub-pulmonary hypoplastic left ventricle that improved the patient’s clinical status, becoming a novel alternative in this particular subset of patients.
INTRODUCTION
The natural progression to hypoplastic left heart syndrome can be modified and even reversed in some patients by a staged left ventricle (LV) recruitment strategy [1]. In the most severe end of the spectrum of disease, it can be initiated prenatally with a foetal aortic valvuloplasty [2]. Nevertheless, some patients that undergo these interventions do not achieve adequate LV size and function, develop pulmonary hypertension (PH) and loose candidacy for both biventricular reconversion and univentricular palliation. The aim of this study is to report a case of a successful reverse double switch operation in a patient with failure of staged LV recruitment and PH in order to achieve a one-and-a-half ventricle repair (1.5VR) with the LV in a sub-pulmonary position.
CASE REPORT
Written informed consent was obtained for publication of the information included in this study.
A successful foetal aortic valvuloplasty was performed at 27 weeks of gestation in a foetus with critical aortic stenosis and a normal-sized hypocontractile fibroelastotic LV. The 3583 g, full-term newborn had a LV volume of 20 ml/m2 and underwent a Damus–Kaye–Stansel procedure with a 5 mm right ventricle (RV)-to-pulmonary artery (PA) polytetrafluoroethylene conduit, a 6 mm interatrial communication and the reconstruction of the aortic arch. At 6 months endocardial fibroelastosis resection, mitral splitting, a 3 mm-fenestrated atrial septum patch closure and the Glenn procedure were performed. Due to thrombosis of the innominate vein and RV-to-PA conduit, the patient required an urgent surgical thrombectomy, the replacement of the conduit and creation of a large atrial septum fenestration. Homozygosis for prothrombin 20210 mutation was detected. At 20 months of age, left heart structures’ growth was observed, with a LV volume of 27 ml/m2 with good contractility and a left ventricular end-diastolic pressure (LVEDP) of 15 mmHg, and as the prothrombin thrombophilia made the patient a poor candidate for the Fontan circulation, an aortic commissurotomy, a new 5 mm-fenestrated atrial septum patch closure and the replacement of the RV-to-PA conduit with an 8 mm polytetrafluoroethylene conduit were carried out.
At 3 years of age, the LV had a volume of 35 ml/m2, but high LVEDP (18 mmHg) revealed diastolic dysfunction, and there was PH (20 mmHg). In this scenario, a hemi-Mustard procedure, an inverted Jatene operation and the removal of the RV-to-PA conduit were performed, with the aim of achieving a 1.5VR with the LV in a sub-pulmonary position. The hemi-Mustard technique was slightly modified by not unroofing the coronary sinus, and by the inferior orientation of the constructed baffle. The neo-PA was reconstructed with 2 bovine pericardium patches, and the neoaorta reconstruction included the Damus–Kaye–Stansel take-down with coronary transfer to the posterior sinuses with trap-door technique, aortic reduction and an end-to-end anastomosis (Fig. 1). At follow-up at 5 years of age, the patient was in good clinical health status, with good systemic right ventricular function, a competent tricuspid valve and good sub-pulmonary LV contractility.
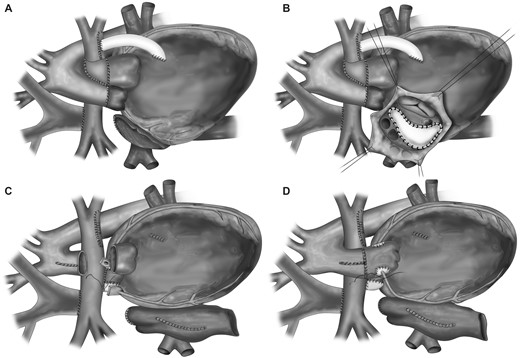
Surgical technique. (A) Initial status: Damus–Kaye–Stansel procedure and Glenn operation (pulmonary arteries connected to the Glenn anastomosis on the right, and to the Sano connection on the left). (B) Hemi-Mustard procedure without unroofing of the coronary sinus. (C) Neo-pulmonary artery reconstruction and removal of the coronary buttons. (D) Neoaorta reconstruction with coronary reimplantation and reduction of the ascending aorta.
DISCUSSION
A 1.5VR with a sub-pulmonary LV was achieved by means of a reverse double switch operation in a patient in whom staged LV recruitment failed to attain biventricular repair, and PH and a genetic coagulation disease advised against the univentricular pathway.
Some patients who undergo a LV recruitment strategy do not achieve left heart structures’ size and function needed for biventricular repair, and many of them are high-risk candidates for univentricular surgery. Heart transplantation may be considered, but at a young age there is less donor availability and a higher associated retransplantation rate. The achievement of a 1.5VR with a sub-pulmonary LV by means of a reverse double switch operation has been reported before in 4 cases [3, 4]. These patients had a small-sized restrictive LV and failure of previous strategies, but different types of congenital heart defects and previous therapeutic strategies compared with the patient presented in this report, which thus contributes to broaden the possible application scenarios for this novel surgical technique.
CONCLUSIONS
A reverse double switch operation, achieving a 1.5VR with a hypoplastic sub-pulmonary LV, is a novel therapeutic strategy for patients with failure of the LV recruitment strategy.
Funding
This research received no specific grant from any funding agency int he public, commercial, or not-for-profit sectors.
Conflict of interest: All authors declare that they have no conflicts of interest.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Sitaram Emani and the other anonymous reviewer(s) for their contribution to the peer review process of this article.




