-
PDF
- Split View
-
Views
-
Cite
Cite
Fangfan Ye, Qiang Fu, Jia Huang, Severe spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema precipitated by pepper spray-induced acute laryngitis: a case report, Interactive CardioVascular and Thoracic Surgery, Volume 35, Issue 2, August 2022, ivac079, https://doi.org/10.1093/icvts/ivac079
Close - Share Icon Share
Abstract
We report a patient with severe spontaneous pneumomediastinum (SPM), pneumothorax and widespread subcutaneous emphysema with acute epiglottitis after inhaling pepper spray. The effects of pepper spray, which is a lachrymatory agent, on the respiratory system have not been reported. Upper airway obstruction is not a well-described cause of SPM, with which subcutaneous emphysema and pneumothorax might coexist; thus, mechanical ventilation might be detrimental.
This research was conducted according to the Declaration of Helsinki guidelines. The research and ethics committee of The Third People’s Hospital of Shenzhen approved the study and waived the requirement for informed consent. No personal information is provided to protect the patient’s confidentiality and anonymity. A 50-year-old man presented to the emergency department with 1 h of dyspnoea associated with pharyngalgia, odynophagia and hoarseness, after being exposed to pepper spray 14 h previously. Before admission, with a round-shaped swollen epiglottis evident under the electronic laryngoscope, he was diagnosed with acute epiglottitis and treated in a local clinic with nebulized corticoids, but without any remission of his dyspnoea. He denied severe cough, chest pain, nausea, vomiting or headaches, had no history of drug abuse and barely drank alcohol or smoked.
On arrival, the physical examination revealed an agitated patient with severe respiratory distress. His SpO2 was 80%–85% on room air, which improved to 90% on a non-rebreather mask at 10 l/min. His respiratory rate was 30 breaths/min, his temperature was 36.5°C, his pulse rate was 112 bpm and his blood pressure was 145/88 mmHg. To ease his respiratory distress, an emergency tracheotomy was performed on the 2nd to 4th tracheal rings. Then he was ventilated on a pressure-controlled synchronized intermittent mandatory ventilation (P-SIMV) mode under the continuous infusion of remifentanil and propofol, with the SpO2 climbing quickly to 98%, and was subsequently transferred to the intensive care unit (ICU).
His complete blood count showed a sharp increase in white blood cells (24 x 109) with neutrophilia of 84%, but with negative results on serological tests for virus. Other laboratory test results were unremarkable. After 6 h of ventilation, an ICU therapist reported an increase in his heart rate to 100 bpm, a decrease in SpO2 to 92%, and an increase in the peak airway pressure to 25 mmHg. When we detected crepitus, percussion of hyper-resonance and auscultation of weak breath sounds on his bilateral chest walls, we strongly suspected a bilateral pneumothorax with subcutaneous emphysema. Emergency high-resolution computed tomography of the neck and chest showed that (1) the upper airway was completed blocked by a swollen epiglottis (Fig. 1a); and (2) severe pneumomediastinum (Fig. 1b), a pneumothorax (Figure 1c) and widespread subcutaneous emphysema (Figure 1d) were easily detected. Because he had no history of chest trauma, we diagnosed it as SPM, a pneumothorax and subcutaneous emphysema.
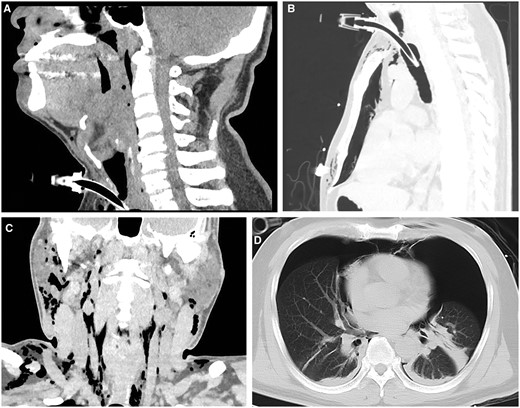
(a) Coronal high-resolution computed tomography image of the neck shows that the upper airway (from the larynx to the site just above glottis) was completely blocked with a swollen epiglottis in between; (b) severe spontaneous pneumomediastinum; (c) a large-scale subcutaneous emphysema; and (d) pneumothorax.
Bilateral chest tubes were inserted immediately; a lot of bubbles leaked out. His vital signs were then stabilized, and the bilateral lungs were re-inflated. On day 2 after admission to the ICU, with his oxygen index improved, he was weaned from mechanical ventilation. On day 3, the chest tubes were removed when no movement of the water column was observed and no signs of a pneumothorax were evident on his chest X-ray.
Pepper spray is a lachrymatory agent with a quick, short-term effect. In this patient, however, it had a delayed onset and a life-threatening effect on the respiratory system that caused acute epiglottitis. SPM usually has a benign clinical course, of which the most common triggers include emesis, cough, physical effort and other activities associated with an extreme Valsalva manoeuvre [1]. To our knowledge, this case is the first in which SPM was precipitated by pepper spray-induced acute epiglottitis.
Acute epiglottitis can cause upper airway obstruction, whereby forceful inspiration efforts against an epiglottic obstruction result in intrapleural pressures as low as –13 kPa. We postulated that the pressure gradient between the parts of the intrapleural cavity, alveola, mediastinum and soft tissue on the neck permits the gas to move among them and leads to SPM, subcutaneous emphysema and pneumothorax.
SPM is caused by the pressure gradient between the alveoli and the mediastinum. In 1944, Macklin et al. first described the pathophysiological mechanism as released air from an alveolar rupture (because of high intra-alveolar pressure caused by expiratory exertion) that centripetally dissects the pulmonary interstitium along the bronchovascular sheaths towards the pulmonary hila and into the mediastinum [2]. On the HRCT scan, it was seen as a linear collection of air contiguous with the bronchovascular sheath [3], which can also be found in our patient (Fig. 2). Localized pressure increases as the gas accumulates within the mediastinal space, generating a pressure gradient between the mediastinum and the intercommunicated soft tissue nearby, which finally causes subcutaneous emphysema. Because intrapleural pressure is the lowest airway pressure in patients with inhalational exertion, the alveoli-intrapleural and/or the mediastinum-intrapleural space pressure gradient may lead to the air flowing into the intrapleural space and may thereby cause a pneumothorax.
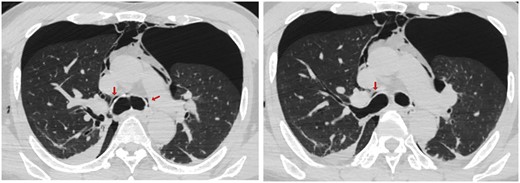
High-resolution computed tomography scan demonstrates air collected along the perivascular connective tissue, the Macklin effect (arrows), in the perihilar area, and pneumomediastinum and bilateral pneumothorax.
A pneumothorax can be a severe complication during mechanical ventilation; however, it is more common in patients with a history of a respiratory disease (i.e. COPD or pneumonitis such as severe acute respiratory syndrome coronavirus 2), or patients with high tidal volume settings. Our patient was in good health with no special history, and he was under protective ventilation. As a result, we believe that the upper airway obstruction caused by acute epiglottitis is the first inducement and the main cause of the pneumomediastinum, subcutaneous emphysema and pneumothorax, which can be easily exacerbated by mechanical ventilation, during which a tension thorax might also occur. A tension pneumothorax may lead to dislocation of and damage to major organs and arteries, thus causing instability of the vital signs, which may be life-threatening. Though with 40–70% lung compression, our patient exhibited only slight changes in his vital signs because the lateral pneumothorax managed to balance the pressure between the 2 chest cavities.
Therefore, we concluded that the pepper spray may have delayed, long-lasting respiratory effects. For patients with upper airway blockage, the probability is high that the pneumomediastinum, subcutaneous emphysema and pneumothorax are concomitant. If mechanical ventilation is inevitable, we suggest a chest X-ray or CT scan afterwards to exclude a pneumothorax or even a tension pneumothorax.




