-
PDF
- Split View
-
Views
-
Cite
Cite
Anna Krokovay, Martin Schweiger, Oliver Kretschmar, René Prêtre, Reimplantation of the left coronary artery with aortic intramural course in an ALCAPA patient, Interactive CardioVascular and Thoracic Surgery, Volume 34, Issue 6, June 2022, Pages 1171–1173, https://doi.org/10.1093/icvts/ivab299
Close - Share Icon Share
Abstract
We present a case of an anomalous origin of the left coronary artery from the pulmonary artery, with a proximal intramural course in the aortic wall. We describe the technique of its reimplantation at the site of the transverse aortotomy, using autologous pericardial patch enlargement of the newly created coronary ostium.
INTRODUCTION
Anomalous origin of the left coronary artery (LCA) from the pulmonary artery is a rare congenital anomaly [1]. Various surgical therapy options re-establish myocardial blood supply by 2 coronary artery systems. Direct reimplantation of the anomalous coronary artery to the aorta has become the method of choice [2, 3].
PATIENTS AND METHODS
A 2-month-old female patient was admitted to our emergency unit due to dilated cardiomyopathy of unclear origin. Transthoracic echocardiography showed severely reduced left ventricular ejection fraction (<20%), minimal mitral regurgitation, slightly reduced right ventricular function and a secundum atrial septal defect. Coronary angiography revealed an anomalous origin of the LCA from the main pulmonary artery.
Surgical technique
After establishing normothermic cardiopulmonary bypass between both venae cavae and the ascending aorta, cold blood cardioplegia was administered into the aortic and the pulmonary root.
Intraoperative findings revealed the LCA arising at the branching point of the right pulmonary artery, just above the right pulmonary sinus, the left main stem passing interarterial between the main pulmonary artery and the aortic root.
The main pulmonary artery was transected and the LCA ostium was excised with a button of the surrounding pulmonary artery wall. Its proximal segment was coursing horizontally under the adventitia of the aorta, running from the facing commissure over the left coronary sinus. Approaching the commissure between the left and non-coronary cusps, it also shared a layer of media with the aorta, without entering its lumen (Figs 1A and 2A). In order to facilitate dissection of the LCA beyond its bifurcation, the aorta was divided transversally, a few millimetres above the aortic sinus (Figs 1A and 2B).
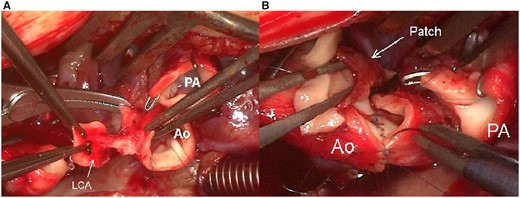
(A) Aortic intramural course of the LCA. (B) Anastomosis between LCA and aorta after patch plasty on the inferior surface of the LCA with native autologous pericardium. Ao: aorta; LCA: left coronary artery; PA: pulmonary artery.
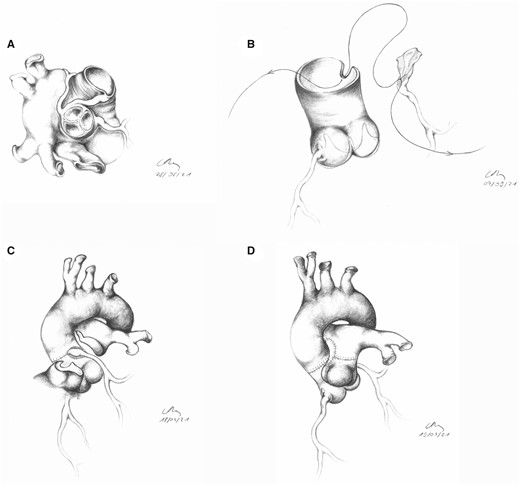
(A) Aortic intramural course of the left coronary artery (LCA). (B) Anastomosis between LCA and aorta after patch plasty of the proximal LCA. The patch had to be inserted on the “intramural” part of the coronary artery wall, in this case, inferiorly. (C) Completed neo-ostium of the LCA. (D) Reconstruction of the pulmonary artery with autologous native pericardial patch.
As it was too long for direct reimplantation, the LCA needed to be shortened proximally in order to avoid any torsion or kinking. To accomplish an anastomosis free from stenosis, the inferior, previously ‘intramural’ surface was enlarged with an autologous native pericardial patch (Fig. 1B). A longitudinal incision was made along the middle line of the patch (Figs 1B and 2B). A small vertical incision was performed in the aortic root above the posterior sinus, starting at the aortotomy (Fig. 2B). The free edges of the patch were anastomosed to the aorta, starting at the base of the vertical incision and continuing at the edges of the transverse aortotomy. In this way, the anastomosis became integrated into the closing suture of the aorta (Fig. 2B and C and Video 1), the LCA presenting a harmonious course. The pulmonary artery was reconstructed with autologous native pericardial patch (Fig. 2D). Finally, the secundum atrial septal defect was closed with running suture.
Translocation of the anomalous origin of the left coronary artery from the pulmonary artery into the aorta.
Due to severely reduced left ventricular function postoperative extracorporeal life support was established. Weaning off extracorporeal life support and respirator could be accomplished 10 and 15 days after surgery, respectively.
RESULTS
One-month follow-up invasive angiography showed normal perfusion of the coronary arteries, free from stenosis (Supplementary Material, Fig. S1).
DISCUSSION
Due to its favourably adjacent position to the aortic root, transfer of an anomalous LCA originating from the right pulmonary sinus to the aorta can be convenient. In our case, however, after arising from above the right pulmonary sinus, the proximal LCA took an interarterial course between the pulmonary and the aortic root, with an intramural segment embedded in the lateral aortic wall.
In the case of anomalous origin of the LCA from the pulmonary artery with interarterial course, which is difficult to depict precisely preoperatively, surgical treatment can be technically challenging. Care should be taken when mobilizing the proximal LCA between the great arteries, anticipating the possibility of an intramural course within the aortic wall. We recommend transecting the ascending aorta for safe mobilization and precise reimplantation of the ectopic artery. For stenosis free anastomosis at the site of the aortotomy, native autologous pericardium can be safely used for ostial patch plasty.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Julie Cleuziou, Katrien Francois and the other anonymous reviewers for their contribution to the peer review process of this article.




