-
PDF
- Split View
-
Views
-
Cite
Cite
Yun Seok Kim, Jae Suk Yoo, Easy surgical explantation technique for self-expanding transcatheter aortic valve: ‘lasso technique’, Interactive CardioVascular and Thoracic Surgery, Volume 34, Issue 4, April 2022, Pages 691–693, https://doi.org/10.1093/icvts/ivab304
Close - Share Icon Share
Abstract
A prosthesis with a self-expanding nitinol frame firmly incorporates into the aortic wall and thus is difficult to explant. We introduce a novel technique that simplifies explantation.
INTRODUCTION
An 80-year-old man was referred to our hospital for surgery owing to severe prosthetic aortic valve stenosis. He had undergone transcatheter aortic valve replacement (TAVR) 3 years ago and percutaneous coronary intervention 4 years ago. His medical history also included hypertension, diabetes, chronic kidney disease requiring haemodialysis, adrenal insufficiency and encephalopathy.
Preoperative transthoracic echocardiography revealed a mean transvalvular pressure gradient of 63 mmHg and a mild degree of paravalvular leakage. The left ventricular ejection fraction was 60%. After multidisciplinary team discussion, we decided to explant the TAVR prosthesis (CoreValve Evolut R; Medtronic, Minneapolis, MN, USA) and perform surgical aortic valve replacement.
After median sternotomy, cardiopulmonary bypass was instituted by cannulating the distal ascending aorta and right atrial appendage. Antegrade cold crystalloid cardioplegia (modified del Nido solution) was administered after aortic cross-clamping. Transverse aortotomy was carried out at the level on which the nitinol frame was easily palpable. Since the frame had incorporated into the intima due to endothelial tissue growth, creating a space for dissection was challenging. A 2–0 polyester purse-string suture was passed along the edge of the frame and fastened using a tourniquet (Figs 1 and 2). This manoeuvre (termed the ‘lasso technique’) allowed the production of a space for endarterectomy between the frame and the aortic wall. After exposing the widest portion of the frame, a second 2–0 polyester purse-string suture was passed along the frame and fastened using a second tourniquet. Since the frame was narrowest at its waist, the second lasso easily exposed the annulus level. The prosthesis was separated from the aortic valve by applying gentle traction, using the tourniquet as a valve holder. Although the adhesion at the native valve level was firm, separating the prosthesis from the native valve while avoiding tissue damage was not difficult (Video 1). After explanting the TAVR prosthesis, the native aortic valve was excised and debrided. Standard sutureless aortic valve replacement was performed using a Perceval S Medium prosthetic aortic valve (LivaNova, Milan, Italy). The cardiopulmonary bypass and aorta cross-clamping times were 70 and 44 min, respectively. Postoperative transthoracic echocardiography showed no aortic regurgitation and a mean transvalvular pressure gradient of 14 mmHg, with normal left ventricular function. The mechanical ventilator time was 4 h, and the patient was discharged 6 days post-surgery without complications.
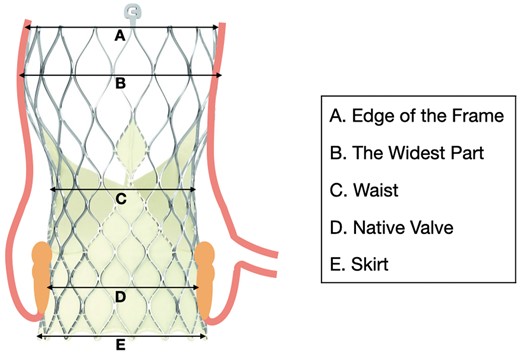
Structure of the CoreValve Evolut R. (A) Edge of the frame. (B) The widest part. (C) Waist. (D) Crushed native valve. (E) Skirt.
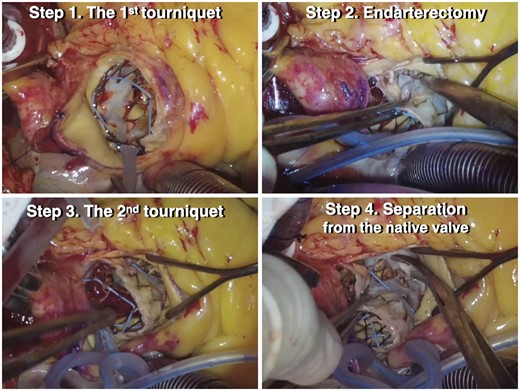
The lasso technique for explanting a prosthesis with a self-expanding frame. Step 1: Purse-string suture at the distal edge of the frame and fastening using a tourniquet. Step 2: Endarterectomy between the frame and the aortic wall. Step 3: A second purse-string suture at the widest part of the frame and fastening using a tourniquet. Step 4: Separation of the device from the native aortic valve.
Easy technique for explantation of a transcatheter prosthesis with a self-expanding nitinol frame, followed by sutureless aortic valve replacement.
This study was approved by the Institutional Review Board and ethics committee of Bucheon Sejong Hospital (Approval number, 2021-0242; Approval date, 6 May 2021), which waived the requirement for informed consent because of the retrospective nature of the study design.
All relevant data are within the manuscript and its supporting information files.
DISCUSSION
TAVR is recommended not only for patients for whom surgical aortic valve replacement is risky or prohibited but also for those with symptomatic severe aortic stenosis older than 65 years [1]. In a recent meta-analysis of >8000 patients with aortic stenosis, TAVR had lower 2-year all-cause mortality and stroke rates than did surgical aortic valve replacement, irrespective of surgical risk [2]. Therefore, the use of TAVR is expected to continue to increase in the future. The need for TAVR prosthesis explantation will also increase: deterioration of the valve is inevitable owing to its innate biologic properties, and prosthesis-related complications (e.g. infective endocarditis, paravalvular leakage) may necessitate prosthesis removal.
Previous recipients of TAVR have a high or prohibitive risk for surgery. The nitinol frame of a TAVR prosthesis is self-expanding and incorporates into the aortic wall. Therefore, cardiac surgeons should understand the innate properties of self-expanding TAVR prostheses and be prepared to explant them safely. There have been several techniques to explant TAVR prosthesis safely and effectively, avoiding aortic root injury. Hernandez-Vaquero et al. [3, 4] used an endarterectomy spatula for meticulous dissection and Valdis et al. [5] used a heavy snaring suture to collapse the prosthesis and facilitate explantation. To create a better surgical field for meticulous dissection, we used 2 consecutive 2–0 polyester snaring sutures, which were fastened by tourniquets. So we could contracted the frame step-by-step and gradually dissected between the aortic wall and the prosthesis without aortic root injury.
The lasso technique is easy to perform and has the potential to reduce bypass and cross-clamping times, which is beneficial to patients for whom surgery is risky.
ETHICS STATEMENT
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal. The study participant provided informed consent, and the study design was approved by the appropriate ethics review board. All authors have substantially contributed to all components.
Conflict of interest: none declared.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Michael W.A. Chu, Daniel Hernandez-Vaquero and the other anonymous reviewers for their contribution to the peer review process of this article.
REFERENCES
Author notes
†Present address: Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.




