-
PDF
- Split View
-
Views
-
Cite
Cite
Chuan Tian, Shiwei Pan, Congenital absence of anterior papillary muscle of the tricuspid valve and surgical repair with artificial chordae, Interactive CardioVascular and Thoracic Surgery, Volume 24, Issue 2, 1 February 2017, Pages 299–300, https://doi.org/10.1093/icvts/ivw327
Close - Share Icon Share
We report the case of a 26-year old woman who underwent successful tricuspid valve repair for the absence of the anterior papillary of the tricuspid valve. Preoperative echocardiography revealed grade IV tricuspid valve regurgitation, caused by congenital absence of the anterior papillary muscle and prolapse of the anterior leaflet. Tricuspid valve repair was performed using artificial chords consisting of two polytetrafluoroethylene sutures and a concomitant ring annuloplasty. Postoperative echocardiography revealed mild tricuspid valve regurgitation. This approach represented a safe and effective technique for tricuspid valve repair in congenital absence of papillary muscle.
CASE DESCRIPTION
A 26-year old woman with recurrent anorexia was admitted to our hospital in 2015. Physical examination revealed a woman of normal weight (height: 160 cm; weight: 52 kg). Systolic murmur (2/6) along lower right sternal border was audible. Blood test showed haemoglobin of 138 g/l and normal serum creatinine value. Echocardiography confirmed the diagnosis of severe (grade IV) tricuspid valve regurgitation with prolapsed anterior leaflet and dilatation of the annulus. Left ventricular ejection fraction and pulmonary artery pressure remained normal. The patient denied history of blunt chest trauma or recurrent fever.
Surgical inspection of regurgitation of the tricuspid valve.
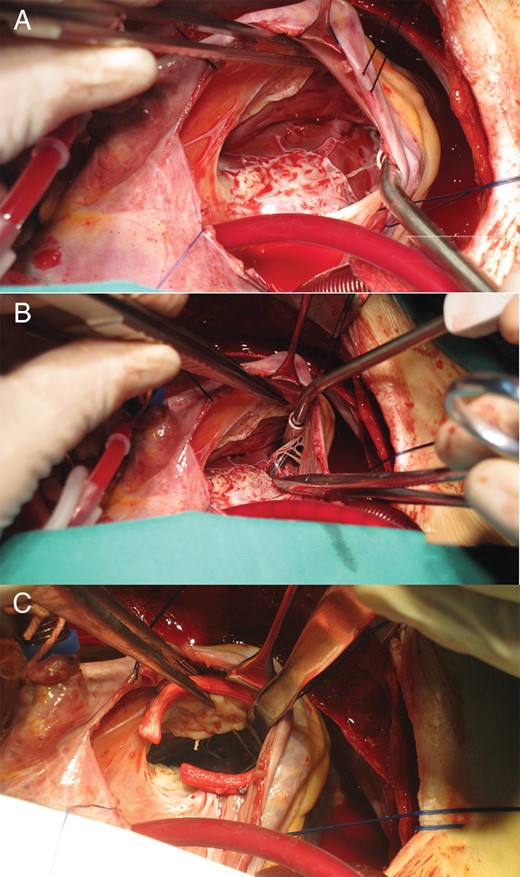
Abnormality of the tricuspid valve papillary muscle and surgical correction. (A) Absence of the anterior papillary muscle. (B) Presence of the septal papillary muscle and the posterior papillary muscle. (C) Placement of a Gore-Tex® suture on the rough edge of the anterior leaflet.
Saline test showing competence of the tricuspid valve after surgical correction.
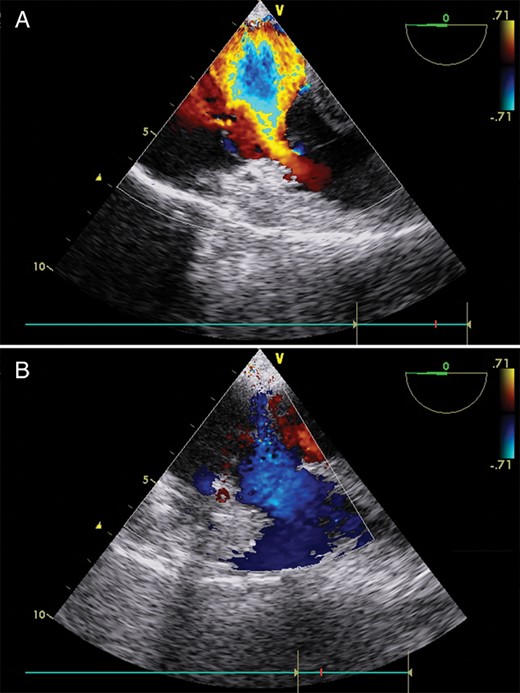
Changes of regurgitation of the tricuspid valve (TEE). (A) Preoperative TEE image confirming severe tricuspid valve regurgitation. (B) Postoperative TEE image showing satisfactory tricuspid valve competence.
The postoperative process was uneventful, and there were no complications after discharge. Follow-up TTE showed good leaflet competence with mild regurgitation. Magnetic resonance imaging (MRI) data revealed that the right ventricle end-diastolic volume restored from 296.8 to 147.4 ml after surgical correction, indicating a promising right ventricle geometry and contraction function recovery.
DISCUSSION
Absence of tricuspid valve papillary muscle is a rare congenital condition. The present case report provided intraoperative visual record of abnormal leaflet movement along with surgical correction outcome when the anterior papillary muscle was absent.
The papillary muscles contract before contraction of the ventricle so as to tighten the chordae and draw the cusps and prevent ventricular blood from regurgitation [1]. Except for the anatomical variations, congenital hypoplasia of the papillary muscles and/or the chordae could cause severe primary tricuspid regurgitation. Surgical correction for the absence of chordae or leaflet have been reported sporadically [2, 3], which indicated that tricuspid valve repair was a reasonable option for the congenital malformation.
Expanded PTFE sutures have well-recognized efficacy and durability in the mitral position, whereas the experience for replacing chordae in the tricuspid valve is limited due to different epidemic. In the present case, determination of the anchor site for the artificial chordae was a critical issue, because the anterior papillary muscle could not be located. We chose the ventricle moderate band instead of the ventricle free wall as the anchor site according to the following presumptions: (i) the length of the artificial chordae would remain proper during the right ventricle postoperative remodelling process; (ii) systolic contraction of the moderate band, where the right branch bundle located, was slightly prior to that of the ventricle free wall, generating a physiological interaction between ventricle contraction and leaflet movement. Besides placement of the artificial chordae, we also performed ring annuloplasty to achieve better outcome in terms of recurrent regurgitation.
Alfieri's description [4] of edge-to-edge leaflet approximation for severe regurgitation should be considered as an option as well. However, artificial chordae for prolapsed leaflet would provide more natural haemodynamic effect and reduce the risk of valve stenosis. Double-orifice repair could be regarded as an effective solution when the initial effort for chordae reconstruction fails.
Conflict of interest: none declared.




