-
PDF
- Split View
-
Views
-
Cite
Cite
Tomokuni Furukawa, Naomichi Uchida, Yoshitaka Yamane, Kazunori Yamada, A pitfall of false lumen embolization in chronic aortic dissection: intimal injury caused by the embolization device edge, Interactive CardioVascular and Thoracic Surgery, Volume 24, Issue 1, January 2017, Pages 153–155, https://doi.org/10.1093/icvts/ivw279
Close - Share Icon Share
We report a case of intimal injury caused by the occluder device in the false lumen (FL) after treatment of refractory chronic aortic dissection with FL embolization. We speculate that the intimal injury was due to the disproportionate stress from the FL. We covered the new entry by an additional stent graft in the true lumen. The deployment of a stent device in both lumens at the level of embolization might be indispensable for FL embolization.
INTRODUCTION
False lumen (FL) embolization is a useful, minimally invasive treatment for chronic aortic dissection. However, reintervention is required in some patients due to the residual retrograde flow in the FL [1]. We present a rare case that underwent reintervention to close a new intimal entry at the location of the occluder device in the FL.
CASE
A 72-year old woman who had persistent abdominal pain was admitted to our hospital. She had a long history of aortic dissection. Eight years prior, she underwent total aortic arch replacement to repair acute type A aortic dissection. Two years earlier, she underwent thoracic endovascular repair (TEVAR) to treat thoracic aortic aneurysm induced by chronic dissection. Within the next 6 months, we performed TEVAR with FL embolization (the candy-plug technique [2]) to treat a thoracoabdominal aortic aneurysm that was caused by retrograde massive blood flow from the distal re-entry. Because of her severe dementia and at the request of her family, we treated the aneurysm using FL embolization.

Preoperative CTA revealed a new intimal entry at the location of the FL embolization device edge and recurrent blood flow in the FL (arrows). CA: celiac artery; RA: renal artery; CTA: computed tomography angiogram; FL: false lumen; TL: true lumen; SMA: superior mesenteric artery.
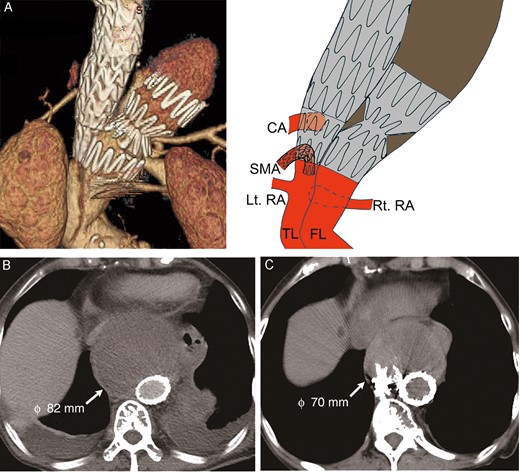
(A) Postoperative CTA demonstrated complete closure of the new entry. (B) CTA at discharge; (C) 1-year follow-up CT. CTA: computed tomography angiogram; RA: renal artery; CA: celiac artery; FL: false lumen; TL: true lumen; SMA: superior mesenteric artery.
DISCUSSION
FL embolization is a useful technique to treat refractory chronic aortic dissection [1, 4]. In these previous reports, the occluder device was deployed in the FL at the level of the distal end of the stent graft in the TL. However, we think that it may be impossible to perform complete FL occlusion in some cases like this one. If the occluder device cannot be deployed at the level of the stent graft in the TL, an extension stent graft should be added in the TL at the level of the distal end of the occluder device in the FL. If we cannot protect visceral perfusion by stenting to deploy the stent graft in the TL at the level of the FL embolization, bare-metal aortic stenting might be useful to stabilize the intimal flap and protect visceral perfusion [5].
According to the experience of this case, we think that the intimal flap is barely stabilized by being sandwiched between the embolized FL and stented TL. The treatment of both lumens at the level of embolization might be indispensable for complete FL embolization.
We think that the prevention of chronic aortic dissection repair is most important because sometimes it is very complex and difficult. More complete distal aortic remodelling at the time of acute aortic dissection might be necessary for preferable aortic outcome. Distal FL obliteration could have been successfully achieved using bare-metal stenting and balloon-induced intimal flap disruption at the time of primary intervention for acute aortic dissection.
CONCLUSIONS
We presented a case of intimal injury caused by disproportionate stress from the occluder device after TEVAR of chronic aortic dissection with FL embolization. Stenting reinforcement of the TL at the level of embolization could be essential for complete FL embolization.
Conflict of interest: none declared.




