-
PDF
- Split View
-
Views
-
Cite
Cite
Bastian Schneider, Johannes Holfeld, Michael Grimm, Ludwig Müller, Intrapericardial left-sided ectopic thyroid mass supplied by the left circumflex artery, Interactive CardioVascular and Thoracic Surgery, Volume 23, Issue 4, October 2016, Pages 671–673, https://doi.org/10.1093/icvts/ivw097
Close - Share Icon Share
Abstract
Intrapericardial left-sided ectopic thyroid tissue is a rare entity. We report a 47-year old female patient with an intrapericardial mass mounting the left atrial wall. Two prominent vessels, both originating from the left circumflex artery (LCX), supplied the tumour. Owing to the compression of the left atrium and the left upper pulmonary vein, the patient was highly symptomatic with exertional dyspnoea and ventricular extrasystoles. Histopathological examination showed regressive thyroid adenoma with no signs of malignancy. Complete resection was feasible. The evaluation of thyroid hormone levels was not indicative for diagnosis. Postoperative hormone substitution appeared to be unnecessary.
INTRODUCTION
Intrapericardial left-sided ectopic thyroid tissue is a rare finding [1]. Lingual thyroid is the most frequent form (90%) of ectopic thyroid. Aberrant migration of the thyroid gland in the early stage of embryogenesis leads to this condition, though the exact pathogenesis remains unclear. It is estimated that 15% of ectopic thyroid findings show signs of malignancy [2] and at least one case of malignant intracardiac thyroid tissue is reported [1].
CASE REPORT
A 47-year old female patient suffered from dyspnoea and angina symptoms (New York Heart Association functional class III). Routine examination was unremarkable, except for frequently occurring ventricular extrasystoles. Transthoracic and consecutive transoesophageal echo were performed, which revealed an intrapericardial mass located near the cranio-lateral left atrium. Incidentally, a haemodynamically irrelevant patent foramen ovale (PFO) was found. Magnetic resonance imaging (Fig. 1) and computed tomography (CT) showed no signs of myocardial infiltration by the mass. Routine preoperative coronary angiography revealed an unremarkable coronary anatomy; however, a direct supply of the tumour by two small branches of the left circumflex artery (LCX) was apparent.

Magnetic resonance imaging showing the localization of the cardiac mass (circle), compressing the left atrium (LA) and the left upper pulmonary vein (arrow). The view shows the right ventricle (RV), the right atrium (RA) and the left ventricle (LV).
The patient was referred to our cardiac surgery department with the diagnosis of a cardiac tumour of unknown origin. To exclude malignancy, a F18 fluorodeoxyglucose positron emission tomography scan was performed, in which the mass showed no increased metabolic activity.
Because a biopsy was not possible and to severity of symptoms, the patient underwent exploratory surgery. After complete median sternotomy and subsequent incision of the pericardium, a 5 × 4 × 4 cm mass descending from the cranio-lateral wall of the left atrium with close relation to the pulmonary artery and the left upper pulmonary vein was found (Fig. 2A). Arterial cannulation of the ascending aorta, as well as venous bicaval cannulation, was performed. After starting partial cardiopulmonary bypass (CPB), the tumour mass was dissected from the pulmonary artery. Two small branches originating from the LCX supplied the tumour, which were clipped. The mass was resected. As indicated by the CT scan, the tumour had no infiltrative growth and was surrounded by a connective tissue capsule (Fig. 2B). Malignancy was excluded by intraoperative frozen-section analysis and the diagnosis of a regressive thyroid adenoma was confirmed by a detailed histopathological analysis.
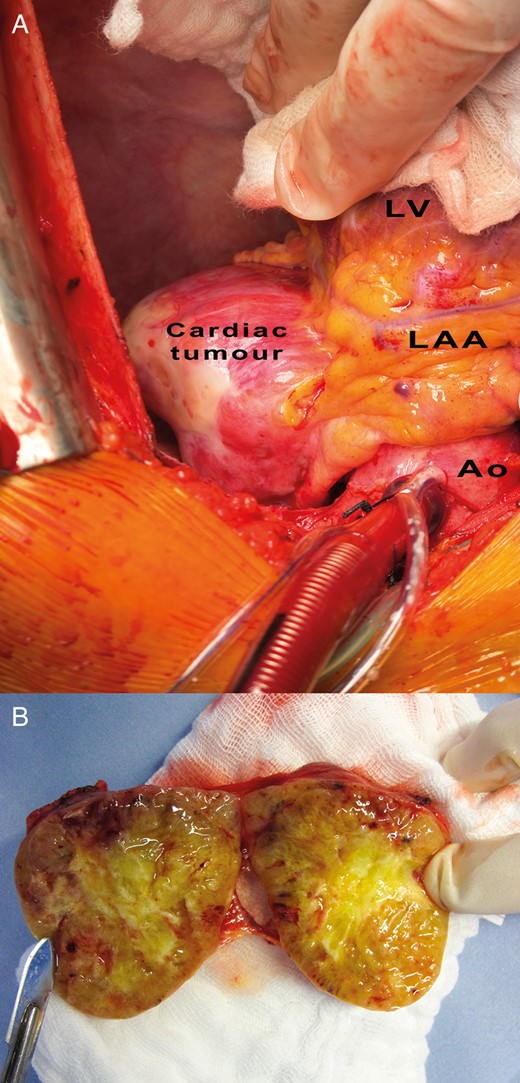
Illustration of the cardiac tumour in situ, bordering the left atrial appendage (LAA), the left ventricle (LV) and the ascending aorta (Ao). (A) Longitudinal section through the cardiac tumour shows its macroscopic inner structure. The tumour is surrounded by a connective tissue in a capsule-like fashion. The tumour parenchyma is no-dose and inhomogeneous, with a star-shaped scar and signs of haemorrhage in the centre (B).
After a full CPB was established, the aorta was clamped and St Thomas II cardioplegia was applicated antegradely. The PFO was closed through a small right atriotomy. Total CPB time was 80 min. The aortic clamping time was 12 min. After an uneventful postoperative course, the patient was discharged in a good condition on the 7th postoperative day. Postoperative echocardiography showed a normal ejection fraction and intact valve morphology. In standardized bicycle ergometry, the patient achieved 93% of age-adjusted standard value.
Eight months later, the patient was free of symptoms. Thyroid ultrasound revealed a multinodular goitre, which was further investigated by iodine-123 scintigraphy single photon emission computed tomography. The thyroid nodules appeared unsuspicious. No residual ectopic thyroid tissue could be detected inside the pericardium.
DISCUSSION
Cardiac thyroid masses appear to be predominately related to the right heart. In the majority of cases, intracardiac thyroid tissue originates from the interventricular septum and proliferates into the right ventricular outflow tract (77.7%) [1].
The patient had no history of thyroid disease and presented with normal thyroid-stimulating hormone (TSH) levels preoperatively. At the time of discharge, TSH levels showed latent hyperthyroidism, most likely due to the application of iodine-based contrast agent.
In most cases, ectopic thyroid tissue is an incidental finding. The tumour becomes clinically apparent by the compression of neighbouring structures like cardiac chambers or coronary vessels. Intracardiac thyroid tumours may cause outflow or inflow obstruction, valvular stenosis, ventricular arrhythmias, thrombus formation or embolism. The clinical manifestation is dominated mostly by the anatomical location and the size of the tumour, whereas hormonal activity is of little value. An average patient age of 55 years at the time of diagnosis supports the assumption that ectopic thyroid tissue remains clinically and endocrinologically silent [2, 3]. Females may be more susceptible than males [1].
Although preoperative imaging may enable a tentative diagnosis of the type of cardiac tumour, certainty can only be established by a surgical excision with histopathological analysis. Because of the rarity of heart-related ectopic thyroid tissue, knowledge of differential diagnosis is crucial. Cardiac metastases occur far more frequently than primary cardiac tumours (differing by the factor of 100–1000). Thus, the diagnostic evaluation for extracardiac primary tumours or further metastases is a key element in preoperative diagnostics and has a profound impact on the prognosis of the patient. Common origins of cardiac metastases are breast cancer, lymphoma, leukaemia and lung cancer. The majority of primary cardiac tumours are benign. Myxomas make up about 75% of benign cardiac tumours, typically located in the left atrium, originating from the interatrial septum. Most of them appear pediculated. In contrast, cardiac ectopic thyroid tumours generally appear to have a broad base [1, 4].
CONCLUSION
Excision of the thyroid tumour is the treatment of choice in symptomatic patients. Limited data are available on the conservative management of asymptomatic patients [1]. Our case demonstrates that this type of tumour can safely be resected in toto due to its connective tissue capsule. Hormone levels do not seem to be conclusive for diagnosis, and preoperative hormone treatment is not generally recommended. The prognosis after surgical resection, like in most benign cardiac tumours, is favourable [4, 5].
CONSENT
The written informed consent was obtained from the patient for publication of this case report and the accompanying images.
Conflicts of interest: The authors have no financial or personal interests to declare that might be potentially viewed to influence the work presented.




