-
PDF
- Split View
-
Views
-
Cite
Cite
Kai Xu, Wen Bian, Hongya Xie, Haitao Ma, Bin Ni, Single-port video-assisted thoracoscopic wedge resection: novel approaches in different genders, Interactive CardioVascular and Thoracic Surgery, Volume 23, Issue 2, August 2016, Pages 202–207, https://doi.org/10.1093/icvts/ivw119
Close - Share Icon Share
Abstract
To discuss the feasibility, safety and superiority of novel approaches in single-port video-assisted thoracoscopic wedge resection in different genders.
The clinical data of patients who underwent thoracoscopic pulmonary wedge resection were analysed. A total of 197 consecutive male patients from January 2012 to December 2014, and 72 female patients from June 2013 to December 2014 were included retrospectively. Of the males, 65 received a transareolar single-port procedure (TASP Group) and 132 received a standard two-port procedure (Standard Group A). Among the females, 18 were treated with a subxiphoid single-port procedure (SXSP Group), and 54 were treated with the standard procedure (Standard Group B). The general clinical materials and surgical outcomes were evaluated.
All patients underwent total thoracoscopic wedge resection successfully, and no severe complications were observed. In men, there were no significant differences in operation time, blood loss, postoperative drainage amount, chest drainage duration, postoperative hospital stay or pain score on the first postoperative day (P = 0.827; 0.423; 0.174; 0.440; 0.115; 0.159, respectively). The pain scores of the TASP Group on the day before and after removal of the chest tube were lower (P = 0.006; 0.023, respectively) than those of Standard Group A, and the incision-associated paraesthesia in the third and sixth month after operation was reduced (P = 0.041; 0.026, respectively). The incision satisfaction degree was significantly improved in the TASP Group (P = 0.001). In women, there were no significant differences in blood loss, drainage amount, chest drainage duration or postoperative hospital stay (P = 0.680; 0.757; 0.651; 0.608, respectively). The operation time of the SXSP Group was longer (P = 0.000), and the pain scores on the first postoperative day and the days before and after removal were all significantly lower (P = 0.000; 0.000; 0.000, respectively) than those of the Standard Group B. Furthermore, the incision paraesthesia 3 and 6 months after surgery was greatly reduced (P = 0.001; 0.001, respectively), although the patients were not very satisfied with the cosmetic results (P = 0.577).
In single-port thoracoscopic pulmonary wedge resection, we performed ‘individualized’ procedures based on gender, namely, the transareolar approach in males and the subxiphoid approach in females. These procedures were considered feasible and safe, and showed superiority in reducing postoperative pain. However, the cosmetic results of the subxiphoid approach require further improvement.
INTRODUCTION
With the development of thoracoscopic instruments and techniques, it has been proposed that the application of the single-port approach in pulmonary diseases helps to reduce postoperative pain and to improve physical aesthetics [1–7]. On this basis, we have performed further investigations to improve the procedure in recent years. We selected different incision approaches for thoracoscopic wedge resection based on gender. We performed a transareolar single-port procedure (TASP Group) in males and a subxiphoid single-port procedure (SXSP Group) in females, which achieved some therapeutic effects retrospectively. Here, we provide details of our current procedures as well as the surgical results and patient outcomes compared with those of the standard approach.
MATERIALS AND METHODS
Patients
All patients were from the First Affiliated Hospital of Soochow University and had received video-assisted thoracoscopic pulmonary wedge resection from one surgeon. Retrospectively, 197 consecutive male patients from January 2012 to December 2014 and 72 female patients from June 2013 to December 2014 were included. This study was reviewed and approved by the Institutional Review Board of the First Affiliated Hospital of Soochow University. We performed thoracoscopic wedge resection for various pulmonary diseases, particularly for spontaneous pneumothorax, peripheral nodules, bullae and metastasis. The surgical approaches were selected based on patient preference after a written informed consent was obtained. Patients who used any opiates preoperatively were excluded. If the patients had any comorbidities, such as hypertension, diabetes, nephrosis, chronic obstructive pulmonary disease, heart disease, anaemia, hypoproteinaemia or a coagulation disorder, they were also excluded from the study. According to the different surgical approaches, male patients and female patients were individually divided into two groups. Sixty-five males underwent TASP Group thoracoscopic surgery, and 132 males received the standard two-port procedure (Standard Group A). Eighteen female patients underwent SXSP Group video-assisted thoracoscopic surgery, and 54 females underwent the standard procedure (Standard Group B).
Surgical methods
Patients were under general anaesthesia with single-lung ventilation using a dual-lumen endotracheal tube. The surgeon and assistant were both positioned on the anterior side of the patient with the surgeon positioned cranially.
Transareolar single-port procedure
The patient was positioned in a 60°–75° lateral decubitus position with slight flexion of the table at the middle of the chest, which enabled slight splaying of the rib to improve exposure in the absence of rib spreading. Using a scalpel, a curved skin incision was made along the inferior areola edge with a length of less than 1/2 the areola circumference. Next, the subcutaneous tissue was incised using an electric scalpel. Steering away from the mammary gland, the dissection continued upward towards the chest wall muscle until the third intercostal space was reached, and the intercostal muscle was then dissected using an electric knife to enter the thoracic cavity. Finally, the incision was positioned in the third intercostal space. Using a lap-protector, a 10-mm, 30°endoscope and two other instruments were inserted simultaneously for operation. When we closed the incision, we performed two stitches on the muscle layer, and a chest tube was inserted between them into the thoracic cavity, which made the muscle around the tube sufficiently tight to reduce leakage of any pleural fluid. Next, the subcutaneous tissue and skin were sutured simultaneously in close proximity to the chest tube. Finally, the chest tube was fixed on to the skin knots. When the chest tube was removed, we continuously sutured the skin. (Figs 1–3).
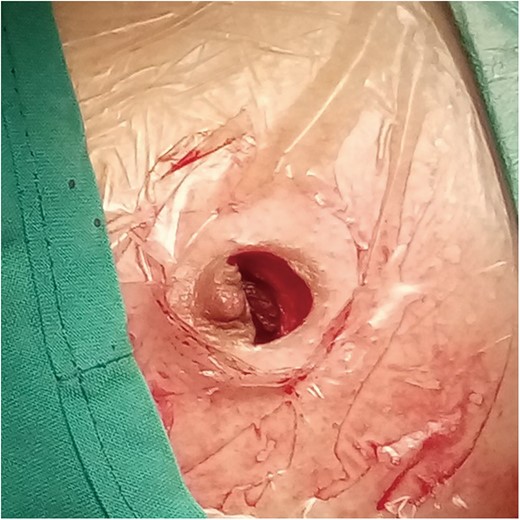
An arc incision was made along the inferior areola border in the transareolar single-port procedure Group.
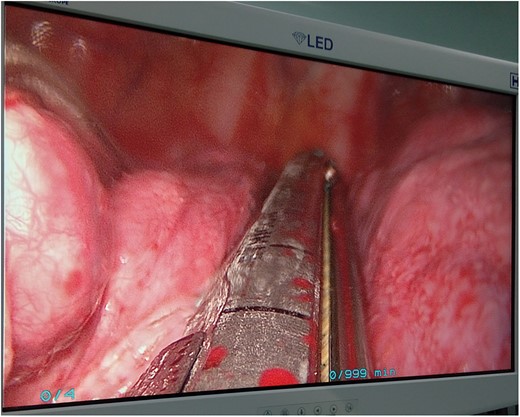
Intrathoracic view on the screen during the transareolar single-port procedure.

Transareolar bilateral scars were not obvious 6 months after surgery.
Subxiphoid single-port procedure
The patient was placed in a semidecubitus position at a 30°–45° angle to the table. A 3-cm longitudinal or transverse incision was made over the subxiphoid area, and a sub-costal tunnel was created by blunt finger dissection from the incision to the pleural cavity. A wound protector was then placed into the wound to provide optimal exposure. A 10-mm, 30° endoscope was inserted through the incision along with an endoscopic grasper and an endostapler (Fig. 4).

Bilateral chest drainages were performed through a subxiphoid incision.
Standard Group A and B
A standardized two-port video-assisted thoracoscopic procedure was performed on the patient. In the 90° lateral position, a 2.0-cm incision was made for observation in the eighth intercostal space along the posterior axillary line, and another 3.0–4.0 cm incision was positioned for operating in the fourth or fifth intercostal space at the anterior axillary line. A 15-mm trocar for the 10-mm, 30° thoracoscope was placed through the observation port, and a wound protector was routinely introduced for working instruments.
With the endoscopic grasper, exploration was initiated to identify the lesion or small bulleae. If there were adhesions, a hook electrocautery was used to provide better exposure. When the pulmonary lesion was targeted, the apex was lifted with a grasper, and an endostapler (Covidien, Norwalk, CT, USA) was positioned on the healthy tissue caudal to the lesion. After the targeted lung was resected, the specimen was placed in a protective specimen bag under thoracoscopic assistance and was removed through the wound protector. Finally, we asked an anaesthesiologist to inflate the lung, and a 28F chest tube was inserted through the incision prior to closure.
Postoperative assessment
All of the patients were extubated at the end of the surgery and were transferred to an intensive care unit. The same postoperative care with a clinical pathway was received during the hospital stay. No analgesic drug was generally given. Patients were encouraged to properly cough and expectorate, and they were encouraged to walk around their bedside on the first postoperative day. When a higher pain score (>4) was reported, pethidine hydrochloride was provided to patients at a dose of 1 mg/kg. A chest X-ray was obtained on the first postoperative day to determine the state of the lung. If there was no atelectasis, pneumonia, pneumothorax, hydrothorax, dense blood, air leakage, purulent or cloudy pleural effusion and the drainage volume was less than 300 ml/day, then the chest tube was removed. Early ambulation was encouraged in the patients, and patients were discharged if there were no serious complications after removal. Patients were followed up in the outpatient department.
Outcome measures
For each patient, the evaluated items included the following: surgical duration, blood loss, postoperative drainage amount, duration of chest drainage, duration of postoperative hospital stay, inpatient pain score, incision satisfaction degree and the number of patients who suffered from incision paraesthesia was noted. Pain scores were evaluated using an improved visual analogue scale when the patients were fully awake, and we obtained the results selectively on the first postoperative day and before and after removal of the chest tube for investigation. There were nine grades from mild to severe, as previously described by Bin et al. [8]. The process was partially blinded because all of the scores were recorded by an attending resident who was unaware of the ongoing study. The interval between the measurements was at least 12 h. The incision satisfaction degree was evaluated in the outpatient department 6 months after surgery and was described as ‘Excellent’, ‘Fair’ or ‘Poor’ in terms of the cosmetic outcome of the incision. Patients who selected ‘Excellent’ and ‘Fair’ were deemed ‘Satisfied,’ whereas a selection of ‘Poor’ was regarded as ‘Dissatisfied.’ The incision paraesthesia was assessed 3 and 6 months after operation and was described as a feeling of ‘pins and needles’, ‘numbness’, or a sensation of abnormal ‘swelling’ in the chest wall [9].
Statistical analysis
Statistical analysis was performed using SPSS version 19.0 software (IBM Corporation, Armonk, NY, USA). Continuous variables were expressed as the mean ± standard deviation, and categorical variables as a percentage. A two-independent-samples t-test was used for inter-group comparisons of continuous variables, whereas a χ2 test or Fisher’ exact test was used to compare the categorical data. All tests were two-sided, and a 5% probability of type I experimental error (P < 0.05) was considered statistically significant.
RESULTS
All of the operative procedures were successful, and in no circumstances was the procedure converted to open thoracotomy. Significant postoperative complications, such as infection, pneumothorax, haemorrhage, hydrothorax and atelectasis were not observed in any patient. The baseline characteristics and postoperative data are fully displayed in Tables 1 and 2.
| Variable . | TASP Group (n = 65) . | Standard Group A (n = 132) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 54 | 105 | χ2 = 0.349 | 0.555 |
| Lung nodules and bullae | 11 | 27 | ||
| Age (years) | 32.8 ± 8.9 | 35.5 ± 10.6 | t = −1.779 | 0.077 |
| Side involves | ||||
| Right/left/bilateral | 38/24/3 | 67/58/7 | χ2 = 1.041 | 0.594 |
| Operation time (min) | 46.1 ± 10.6 | 46.5 ± 11.7 | t = −0.219 | 0.827 |
| Blood loss (ml) | 55.3 ± 16.3 | 53.1 ± 18.9 | t = −0.804 | 0.423 |
| Postoperative drainage amount (ml) | 154.3 ± 114.1 | 181.5 ± 139.1 | t = −1.366 | 0.174 |
| Postoperative drainage time (days) | 1.5 ± 1.2 | 1.6 ± 1.3 | t = −0.773 | 0.440 |
| Postoperative hospital stay (days) | 2.7 ± 1.3 | 3.0 ± 1.4 | t = −1.581 | 0.115 |
| Pain score | ||||
| First postoperative day | 2.94 ± 1.34 | 3.27 ± 1.61 | t = −1.414 | 0.159 |
| Before removal | 3.69 ± 1.38 | 4.31 ± 1.51 | t = −2.773 | 0.006 |
| After removal | 2.54 ± 0.90 | 2.87 ± 0.98 | t = −2.292 | 0.023 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 39 | 98 | χ2 = 4.171 | 0.041 |
| 6 months after operation | 25 | 73 | χ2 = 4.941 | 0.026 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 57/8 | 85/47 | χ2 = 11.748 | 0.001 |
| Variable . | TASP Group (n = 65) . | Standard Group A (n = 132) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 54 | 105 | χ2 = 0.349 | 0.555 |
| Lung nodules and bullae | 11 | 27 | ||
| Age (years) | 32.8 ± 8.9 | 35.5 ± 10.6 | t = −1.779 | 0.077 |
| Side involves | ||||
| Right/left/bilateral | 38/24/3 | 67/58/7 | χ2 = 1.041 | 0.594 |
| Operation time (min) | 46.1 ± 10.6 | 46.5 ± 11.7 | t = −0.219 | 0.827 |
| Blood loss (ml) | 55.3 ± 16.3 | 53.1 ± 18.9 | t = −0.804 | 0.423 |
| Postoperative drainage amount (ml) | 154.3 ± 114.1 | 181.5 ± 139.1 | t = −1.366 | 0.174 |
| Postoperative drainage time (days) | 1.5 ± 1.2 | 1.6 ± 1.3 | t = −0.773 | 0.440 |
| Postoperative hospital stay (days) | 2.7 ± 1.3 | 3.0 ± 1.4 | t = −1.581 | 0.115 |
| Pain score | ||||
| First postoperative day | 2.94 ± 1.34 | 3.27 ± 1.61 | t = −1.414 | 0.159 |
| Before removal | 3.69 ± 1.38 | 4.31 ± 1.51 | t = −2.773 | 0.006 |
| After removal | 2.54 ± 0.90 | 2.87 ± 0.98 | t = −2.292 | 0.023 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 39 | 98 | χ2 = 4.171 | 0.041 |
| 6 months after operation | 25 | 73 | χ2 = 4.941 | 0.026 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 57/8 | 85/47 | χ2 = 11.748 | 0.001 |
TASP: transareolar single-port procedure.
| Variable . | TASP Group (n = 65) . | Standard Group A (n = 132) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 54 | 105 | χ2 = 0.349 | 0.555 |
| Lung nodules and bullae | 11 | 27 | ||
| Age (years) | 32.8 ± 8.9 | 35.5 ± 10.6 | t = −1.779 | 0.077 |
| Side involves | ||||
| Right/left/bilateral | 38/24/3 | 67/58/7 | χ2 = 1.041 | 0.594 |
| Operation time (min) | 46.1 ± 10.6 | 46.5 ± 11.7 | t = −0.219 | 0.827 |
| Blood loss (ml) | 55.3 ± 16.3 | 53.1 ± 18.9 | t = −0.804 | 0.423 |
| Postoperative drainage amount (ml) | 154.3 ± 114.1 | 181.5 ± 139.1 | t = −1.366 | 0.174 |
| Postoperative drainage time (days) | 1.5 ± 1.2 | 1.6 ± 1.3 | t = −0.773 | 0.440 |
| Postoperative hospital stay (days) | 2.7 ± 1.3 | 3.0 ± 1.4 | t = −1.581 | 0.115 |
| Pain score | ||||
| First postoperative day | 2.94 ± 1.34 | 3.27 ± 1.61 | t = −1.414 | 0.159 |
| Before removal | 3.69 ± 1.38 | 4.31 ± 1.51 | t = −2.773 | 0.006 |
| After removal | 2.54 ± 0.90 | 2.87 ± 0.98 | t = −2.292 | 0.023 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 39 | 98 | χ2 = 4.171 | 0.041 |
| 6 months after operation | 25 | 73 | χ2 = 4.941 | 0.026 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 57/8 | 85/47 | χ2 = 11.748 | 0.001 |
| Variable . | TASP Group (n = 65) . | Standard Group A (n = 132) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 54 | 105 | χ2 = 0.349 | 0.555 |
| Lung nodules and bullae | 11 | 27 | ||
| Age (years) | 32.8 ± 8.9 | 35.5 ± 10.6 | t = −1.779 | 0.077 |
| Side involves | ||||
| Right/left/bilateral | 38/24/3 | 67/58/7 | χ2 = 1.041 | 0.594 |
| Operation time (min) | 46.1 ± 10.6 | 46.5 ± 11.7 | t = −0.219 | 0.827 |
| Blood loss (ml) | 55.3 ± 16.3 | 53.1 ± 18.9 | t = −0.804 | 0.423 |
| Postoperative drainage amount (ml) | 154.3 ± 114.1 | 181.5 ± 139.1 | t = −1.366 | 0.174 |
| Postoperative drainage time (days) | 1.5 ± 1.2 | 1.6 ± 1.3 | t = −0.773 | 0.440 |
| Postoperative hospital stay (days) | 2.7 ± 1.3 | 3.0 ± 1.4 | t = −1.581 | 0.115 |
| Pain score | ||||
| First postoperative day | 2.94 ± 1.34 | 3.27 ± 1.61 | t = −1.414 | 0.159 |
| Before removal | 3.69 ± 1.38 | 4.31 ± 1.51 | t = −2.773 | 0.006 |
| After removal | 2.54 ± 0.90 | 2.87 ± 0.98 | t = −2.292 | 0.023 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 39 | 98 | χ2 = 4.171 | 0.041 |
| 6 months after operation | 25 | 73 | χ2 = 4.941 | 0.026 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 57/8 | 85/47 | χ2 = 11.748 | 0.001 |
TASP: transareolar single-port procedure.
| Variable . | SXSP Group (n = 18) . | Standard Group B (n = 54) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 15 | 43 | χ2 = 0.118 | 0.731 |
| Lung nodule and bulla | 3 | 11 | ||
| Age (years) | 31.8 ± 7.9 | 35.6 ± 10.8 | t = −1.377 | 0.173 |
| Side involves | ||||
| Right/left/bilateral | 8/9/1 | 27/24/3 | χ2 = 0.177 | 0.915 |
| Operation time (min) | 60.3 ± 10.2 | 47.5 ± 13.5 | t = 3.676 | 0.000 |
| Blood loss (ml) | 56.4 ± 8.7 | 54.9 ± 14.3 | t = 0.415 | 0.680 |
| Postoperative drainage amount (ml) | 166.0 ± 99.1 | 175.6 ± 104.3 | t = −0.311 | 0.757 |
| Postoperative drainage time (days) | 1.4 ± 0.9 | 1.3 ± 0.9 | t = 0.455 | 0.651 |
| Postoperative hospital stay (days) | 2.6 ± 0.9 | 2.4 ± 0.9 | t = 0.516 | 0.608 |
| Pain score | ||||
| First postoperative day | 1.94 ± 0.87 | 3.48 ± 1.62 | t = −3.827 | 0.000 |
| Before removal | 2.33 ± 0.91 | 4.67 ± 1.80 | t = −5.259 | 0.000 |
| After removal | 1.72 ± 0.67 | 2.90 ± 1.09 | t = −4.350 | 0.000 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 5 | 38 | χ2 = 10.181 | 0.001 |
| 6 months after operation | 2 | 31 | χ2 = 11.655 | 0.001 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 10/8 | 34/20 | χ2 = 0.312 | 0.577 |
| Variable . | SXSP Group (n = 18) . | Standard Group B (n = 54) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 15 | 43 | χ2 = 0.118 | 0.731 |
| Lung nodule and bulla | 3 | 11 | ||
| Age (years) | 31.8 ± 7.9 | 35.6 ± 10.8 | t = −1.377 | 0.173 |
| Side involves | ||||
| Right/left/bilateral | 8/9/1 | 27/24/3 | χ2 = 0.177 | 0.915 |
| Operation time (min) | 60.3 ± 10.2 | 47.5 ± 13.5 | t = 3.676 | 0.000 |
| Blood loss (ml) | 56.4 ± 8.7 | 54.9 ± 14.3 | t = 0.415 | 0.680 |
| Postoperative drainage amount (ml) | 166.0 ± 99.1 | 175.6 ± 104.3 | t = −0.311 | 0.757 |
| Postoperative drainage time (days) | 1.4 ± 0.9 | 1.3 ± 0.9 | t = 0.455 | 0.651 |
| Postoperative hospital stay (days) | 2.6 ± 0.9 | 2.4 ± 0.9 | t = 0.516 | 0.608 |
| Pain score | ||||
| First postoperative day | 1.94 ± 0.87 | 3.48 ± 1.62 | t = −3.827 | 0.000 |
| Before removal | 2.33 ± 0.91 | 4.67 ± 1.80 | t = −5.259 | 0.000 |
| After removal | 1.72 ± 0.67 | 2.90 ± 1.09 | t = −4.350 | 0.000 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 5 | 38 | χ2 = 10.181 | 0.001 |
| 6 months after operation | 2 | 31 | χ2 = 11.655 | 0.001 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 10/8 | 34/20 | χ2 = 0.312 | 0.577 |
SXSP: subxiphoid single-port procedure.
| Variable . | SXSP Group (n = 18) . | Standard Group B (n = 54) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 15 | 43 | χ2 = 0.118 | 0.731 |
| Lung nodule and bulla | 3 | 11 | ||
| Age (years) | 31.8 ± 7.9 | 35.6 ± 10.8 | t = −1.377 | 0.173 |
| Side involves | ||||
| Right/left/bilateral | 8/9/1 | 27/24/3 | χ2 = 0.177 | 0.915 |
| Operation time (min) | 60.3 ± 10.2 | 47.5 ± 13.5 | t = 3.676 | 0.000 |
| Blood loss (ml) | 56.4 ± 8.7 | 54.9 ± 14.3 | t = 0.415 | 0.680 |
| Postoperative drainage amount (ml) | 166.0 ± 99.1 | 175.6 ± 104.3 | t = −0.311 | 0.757 |
| Postoperative drainage time (days) | 1.4 ± 0.9 | 1.3 ± 0.9 | t = 0.455 | 0.651 |
| Postoperative hospital stay (days) | 2.6 ± 0.9 | 2.4 ± 0.9 | t = 0.516 | 0.608 |
| Pain score | ||||
| First postoperative day | 1.94 ± 0.87 | 3.48 ± 1.62 | t = −3.827 | 0.000 |
| Before removal | 2.33 ± 0.91 | 4.67 ± 1.80 | t = −5.259 | 0.000 |
| After removal | 1.72 ± 0.67 | 2.90 ± 1.09 | t = −4.350 | 0.000 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 5 | 38 | χ2 = 10.181 | 0.001 |
| 6 months after operation | 2 | 31 | χ2 = 11.655 | 0.001 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 10/8 | 34/20 | χ2 = 0.312 | 0.577 |
| Variable . | SXSP Group (n = 18) . | Standard Group B (n = 54) . | Statistics . | P-value . |
|---|---|---|---|---|
| Indications | ||||
| Spontaneous pneumothorax | 15 | 43 | χ2 = 0.118 | 0.731 |
| Lung nodule and bulla | 3 | 11 | ||
| Age (years) | 31.8 ± 7.9 | 35.6 ± 10.8 | t = −1.377 | 0.173 |
| Side involves | ||||
| Right/left/bilateral | 8/9/1 | 27/24/3 | χ2 = 0.177 | 0.915 |
| Operation time (min) | 60.3 ± 10.2 | 47.5 ± 13.5 | t = 3.676 | 0.000 |
| Blood loss (ml) | 56.4 ± 8.7 | 54.9 ± 14.3 | t = 0.415 | 0.680 |
| Postoperative drainage amount (ml) | 166.0 ± 99.1 | 175.6 ± 104.3 | t = −0.311 | 0.757 |
| Postoperative drainage time (days) | 1.4 ± 0.9 | 1.3 ± 0.9 | t = 0.455 | 0.651 |
| Postoperative hospital stay (days) | 2.6 ± 0.9 | 2.4 ± 0.9 | t = 0.516 | 0.608 |
| Pain score | ||||
| First postoperative day | 1.94 ± 0.87 | 3.48 ± 1.62 | t = −3.827 | 0.000 |
| Before removal | 2.33 ± 0.91 | 4.67 ± 1.80 | t = −5.259 | 0.000 |
| After removal | 1.72 ± 0.67 | 2.90 ± 1.09 | t = −4.350 | 0.000 |
| No. of patients suffering paraesthesia | ||||
| 3 months after operation | 5 | 38 | χ2 = 10.181 | 0.001 |
| 6 months after operation | 2 | 31 | χ2 = 11.655 | 0.001 |
| Incision satisfaction degree | ||||
| Satisfied/dissatisfied | 10/8 | 34/20 | χ2 = 0.312 | 0.577 |
SXSP: subxiphoid single-port procedure.
In males, the average age of the TASP Group and Standard Group A was 32.8 ± 8.9 years (ranging from 17 to 53 years) and 35.5 ± 10.6 years (ranging from 16 to 59 years), respectively. There were no significant differences between the two groups (P = 0.077). In the TASP Group, 54 cases of spontaneous pneumothorax and 11 cases of peripheral nodules and bullae were included. The operative side was on the right in 38, on the left in 24 and bilateral in 3 patients. In Standard Group A, 105 patients had a spontaneous pneumothorax, and another 27 showed peripheral nodules and bullae. Of the Standard Group A, 67 patients underwent the procedure on the right side, 58 on the left side and 7 cases were bilateral. There were also no significant differences in the primary indications and operative sides between the two groups (P = 0.555; 0.594, respectively). Compared with Standard Group A, the pain scores on the day before and after removal of the chest tube were lower (P = 0.006; 0.023, respectively) in the TASP Group, although it was comparable on the first operative day (P = 0.159). The incision-associated paraesthesia 3 and 6 months after operation was reduced (P = 0.041; 0.026, respectively) and the incision satisfaction degree significantly increased in the TASP Group (P = 0.001), although there were no significant differences in terms of operation time, blood loss, postoperative drainage amount, chest tube drainage duration and postoperative hospital stay.
In females, there was no significant difference in the mean age between the two groups, which was 31.8 ± 7.9 years (ranging from 19 to 47 years) in the SXSP Group and 35.6 ± 10.8 years (ranging from 16 to 62 years) in the Standard Group B. In the SXSP group, spontaneous pneumothorax was revealed in 15 patients, and peripheral nodule was observed in 3 patients. The procedure was performed on the right side in 8 cases, on the left side in 9 cases and bilateral in only 1 case. In Standard Group B, 43 cases of spontaneous pneumothorax and 11 cases of peripheral lesions were included. The surgical procedure was performed on the right side in 27 cases, on the left side in 24 cases and was bilateral in 3 cases. There were no significant differences in the primary indications and operative sides between the two groups (P = 0.731; 0.173, respectively). In addition, the blood loss, postoperative drainage amount, chest tube drainage duration and postoperative hospital stay of the two groups were comparable. Importantly, compared with Standard Group B, although the operation time of the SXSP Group was longer (P = 0.000), the pain scores on the first postoperative day and the day before and after removal were all clearly lower (P = 0.000; 0.000; 0.000, respectively). Furthermore, the incision paraesthesia in the third and sixth postoperative month were significantly reduced (P = 0.001; 0.001, respectively) in the SXSP Group. However, with regard to the cosmetic results, the patients in the SXSP Group did not show greater satisfaction than those in Standard Group B (P = 0.577).
There were no unplanned admissions to the hospital after discharge in either group. The pathological results were bullae, benign tumours and metastasis, and all patients had R0 resections retrospectively. In addition, no patient experienced significant complications or recurrences in 6 months after the operation.
COMMENT
Minimally invasive surgery is now considered a technically feasible option for many types of pulmonary surgery because of its decreased postoperative pain, reduced impairment of pulmonary function, shorter duration of chest insertion and consequently shorter hospital stays [10]. On the basis of the ‘uniportal’ approach, we proposed ‘individualized’ incisions for pulmonary wedge resection, which were considered to have improved the aesthetics and reduced postoperative pain to a degree.
In males, the transareolar approach was applied to surgical resection of peripheral pulmonary lesions due to its highly favourable cosmetic results. The surgical incision is hidden in the areola area, and the scar is relatively concealed [11, 12]. The length of the arc incision at the edge of the areola usually reaches 3–4 cm, which provides an appropriate work space and reduces instrument collision. In addition, the surgical incision is located in the third intercostal space of the front chest where the muscle layer is thinner and the intercostal space is broader than in the lateral chest; this is considered to facilitate operating flexibility. Moreover, with a broader operating space and minimized risk of intercostal nerve injury, another potential advantage of this approach is a reduction in postoperative pain and paraesthesia, which maintains the normal sensation of the nipple area. More than 50% of the patients who received conventional thoracoscopic surgery have been reported to suffer from postoperative paraesthesia related to the incision [9]. If the procedure fails upon encountering extensive dense adhesions or uncontrollable bleeding in the surgical process, it is also easy and safe to convert to a general two-port procedure by placing the patient in a 90° lateral position, adjusting the operating table and creating an extra camera port in the seventh or eighth intercostal space on the midaxillary line.
In females, a transareolar incision through the breast involves mammary gland injury. In addition, the typical single-incision approach described by Wang et al. [10] is generally situated at the edge of the mammary, which causes much discomfort when rubbed against a brassiere. In this study, we made the incision more inferior to the subxiphoid area. This approach requires only a 3-cm horizontal or vertical incision in the upper abdomen. In addition, the intercostal space is bypassed by making a single incision in the subxiphoid area and creating a tunnel into the thorax, thereby avoiding potential nerve injury and compression from operating and intubation [13]. The intercostal neuralgia is thus greatly reduced [14]. Moreover, the SXSP thoracoscopic approach has also proved feasible for the resection of bilateral lesions, such as pneumatoceles and pulmonary metastases, without any additional incisions [15, 16]. However, some limitations of the subxiphoid approach exist. The upper abdomen incision inevitably leaves a visible scar, and some patients are not satisfied with the cosmetic results. They prefer lateral chest incisions to a visible anterior one when given the option. Moreover, the subxiphoid approach provides limited access to the posterior anatomy [17], and thus, a standardized two-port procedure should be performed for cases in which the preoperative assessment shows that the operation would be difficult to complete using this approach. In this case, we merely applied this approach in patients who underwent bilateral lesion resections. This will potentially change when surgical equipment and the thoracoscope become more advanced.
The ‘standard’ uniportal approach has been proposed to be located in the fourth or fifth intercostal space at the anterior axillary line [6, 10], and we adopted novel incisions when performing wedge resection. The TASP procedure is generally accepted because of its superiority in reducing postoperative pain, as well as its aesthetics and operative simplicity. Considering the physiological differences of the mammary gland, we performed the SXSP approach in females in a pilot study, which turned out to be a practical idea, particularly in patients who underwent bilateral lesion resections. Hypertrophic scarring and keloids were not negligible issues in either approach, and further advancements should be made to reduce the incidence of incision-associated complications.
Both procedures were R0 resections, and positive pathological results were obtained in all cases. Significant complications and lesion recurrences in the 6 months after operation were not observed in any patients. Although the superiority of these approaches to the ‘standard’ uniportal approach remains to be determined, the present study in our institution showed that the ‘individualized’ incisions are greatly superior in reducing postoperative pain to the traditional ones, although the cosmetic results were not appreciated in the SXSP procedure. Moreover, the study was non-randomized and retrospective, and our preliminary findings are based on the results of a small sample and a short-term follow-up, no conclusions can be made in terms of long-term effectiveness. Further studies are expected to be performed to evaluate the relationship between surgical procedures, wound-related complications, acute postoperative pain and chronic pain or paraesthesia. The feasibility of these approaches in video-assisted thoracoscopic lobectomy and segmentectomy will likely also be investigated.
ACKNOWLEDGEMENTS
I am grateful to my supervisor, Bin Ni, for his helpful advice, critiques and patience during this study. He devoted a considerable portion of his time to reading the manuscript and making suggestions for further revisions. I also thank my teacher Haitao Ma and my friends and fellow classmates, Wen Bian and Hongya Xie, who teached me data collection, data analysis and translation. Finally, I am also grateful to all of the patients and volunteers in this study for their cooperation.
Conflict of interest: none declared.
REFERENCES
Author notes
The first two authors contributed equally to this study.




