-
PDF
- Split View
-
Views
-
Cite
Cite
Anna L. McGuire, William Petrcich, Donna E. Maziak, Farid M. Shamji, Sudhir R. Sundaresan, Andrew J.E. Seely, Sebastien Gilbert, Digital versus analogue pleural drainage phase 1: prospective evaluation of interobserver reliability in the assessment of pulmonary air leaks, Interactive CardioVascular and Thoracic Surgery, Volume 21, Issue 4, October 2015, Pages 403–407, https://doi.org/10.1093/icvts/ivv128
Close - Share Icon Share
Abstract
The ability to accurately characterize a pulmonary air leak is an essential skill in chest medicine and surgery. The objective was to evaluate interobserver variability in air leak assessments using analogue and digital pleural drainage systems.
Air leak severity in lung resection patients with a pulmonary air leak was prospectively evaluated by at least one thoracic surgeon, one surgical resident and one to two nurses using a standardized questionnaire. The first assessment was performed with pleural drains connected to an analogue system. Subsequently, patients were re-assessed after changing from the analogue to a digital drainage system. The thoracic surgeon's evaluation was considered the reference standard for comparison. Agreement between observers was quantified using the kappa (κ) statistic.
A total of 128 air leak evaluations were completed in 30 patients (thoracic surgeon = 30; nurses = 56; resident = 30; physiotherapists = 12). The mean time between analogue and digital assessment was 2.16 (±1.66) h. The level of observer agreement regarding air leak severity significantly increased from very slight to substantial when using the digital drainage system [analogue κ = 0.03; confidence interval (CI): 0.04–0.11; P = 0.40) (digital κ = 0.61; CI: 0.49–0.73; P < 0.01]. Similar improvements were observed in subgroups of health-care professionals using digital technology.
Digital pleural drainage technology improves the agreement level between members of the health-care team when assessing the severity of a pulmonary air leak after lung resection.
INTRODUCTION
Management of pulmonary air leak is a significant clinical challenge for all thoracic surgeons [1, 2]. Timely detection, accurate objective quantification and monitoring of pulmonary air leaks are difficult goals to achieve in a consistent manner with currently available pleural drainage systems [3–5]. The most widely used pleural drainage systems require the observer to visually detect if a pulmonary air leak is present, and at the same time determine the size of the air leak according to an analogue scale (1+ to 7+) (Figs 1A and B and 2A and B). Bedside assessment of air leak severity is an error-prone task with a significant degree of interobserver variability demonstrated between attending thoracic surgeons using analogue pleural drainage systems [6, 7]. Inherent limitations of analogue pleural drainage systems may be contributing factors to this problem.
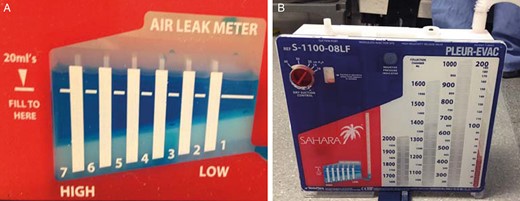
(A) Magnified view of a typical analogue air leak meter found on analogue pleural drainage systems. Air leak severity is determined by visually matching the train of air leak bubbles with the numbered columns (1+ to 7+); (B) Analogue pleural drainage system.
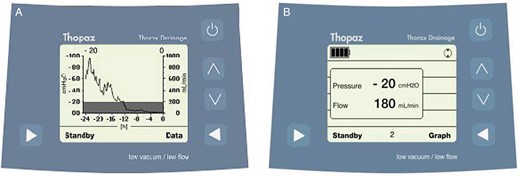
(A) The digital system in graph mode displays the air leak volume over time (ml/min; thin line) and intrapleural pressure (cmH2O; grey bars). (B) The digital system in data mode displays the pressure applied to the pleural space and current air leak flow. This model records 40 patient-days of data. (Image printed with permission from: Thopaz, Medela, Baar, Switzerland)
Previous studies have not evaluated nurses or resident physicians, nor have they examined the experience and training of health-care professionals in relation to the degree of interobserver variability in pulmonary air leak assessment. Inaccuracy or errors in the air leak assessment has the potential to lead to suboptimal patient care outcomes. The inability to accurately determine if an air leak is resolving may result in prolonged hospitalization, premature removal of chest drains and subsequent need for drain reinsertion [8, 9]. A small prospective trial involving only thoracic surgeons demonstrated that consistency in the management of pleural drains was improved with the use of commercially available digital air leak monitoring technology [6]. Quality improvement in the assessment of pulmonary air leak severity can lead to more timely removal of pleural drains and shorter hospitalization [10, 11]. Continuous monitoring over time of the volume of pulmonary air leak can help clinicians establish a trend which may lead to an earlier decision to discharge patients with an indwelling pleural catheter [11, 12]. In a multidisciplinary health-care environment where differences in training, knowledge level and experience continue to prevail, new pleural drainage technologies have the potential to overcome interobserver variability and assist in the management of patients with pulmonary air leak [6, 7].
The aim of this study was to assess interobserver variability in the bedside assessment of pulmonary air leak severity using analogue and digital pleural drainage technology. Our hypothesis was that in the multidisciplinary health-care professional environment, κ statistic levels of agreement in observation of air leak severity assessment will be higher for digital system assessments and lower for analogue chest drainage system assessments.
MATERIALS AND METHODS
Our institutional research ethics board approved the current study, protocol number 2011619-01H. Lung resection patients were prospectively evaluated for the presence of an air leak inclusion criteria by an experienced thoracic surgeon using the analogue pleural drainage system (Sahara Pleurevac, Teleflex, Research Triangle Park, NC, USA). The surgeon's assessment of air leak severity was selected as the reference standard for comparison. Each patient underwent evaluation for air leak severity by members of the health-care team using the analogue system. Within a short period of time, the analogue drainage system was replaced with the digital system (Thopaz, Medela, Baar, Switzerland), and all patients underwent a second assessment by the same observers.
Sample size estimates indicated that 30 patients, evaluated by a minimum of 3 observers, would provide sufficient statistical power using κ statistics to assess interobserver agreement with a β-error of 20% and α-error of 5%. Potential participants were enrolled preoperatively in the chest diseases clinic. On postoperative day 1, they were evaluated at the bedside by at least one experienced thoracic surgeon, one surgical resident and one to two nurses. Using a standardized data collection form, each observer was asked to assess for the presence of air leak. If an air leak was deemed present by the observer, they were asked to document the air leak quality (intermittent versus continuous) and severity (by the analogue meter or by ml/min on the digital device) using the standardized data form. Individual observers were blinded to the responses of others. The experience level of each observer was defined as the duration of time spent caring for lung resection patients. Exclusion criteria were: air leak secondary to poor seal at the pleural drain incision site or defective drainage system, tension pneumothorax or uncontrolled air leak, pneumonectomy or broncho-pleural fistula. De-identified patient and air leak data were stored in a password-protected, electronic database.
Statistical analysis
The κ statistic was used to quantify the level of agreement in air leak severity between the thoracic surgeon and the other observers for the analogue and digital chest drainage systems. Values of κ were scaled as follows: κ < 0 indicates less than chance agreement; 0.01–0.20 slight agreement; 0.21–0.40 fair agreement; 0.41–0.60 moderate agreement; 0.61–0.80 substantial agreement; and 0.81–0.99 almost perfect agreement [13]. Analysis was completed using SAS version 9.2 (SAS Institute, Inc., Cary, NC, USA). Within the analogue and digital chest drainage groups, estimates for κ were generated, followed by 95% upper and lower confidence limits. For the analogue and digital assessments, P-values generated indicate whether the κ value of agreement was significant for the respective chest drainage systems used to assess air leak severity. Following generation of κ values within the separate analogue and digital groups, a P-value was generated comparing the difference of the κ level of agreement between groups.
RESULTS
Study participants were enrolled from the Ottawa Hospital thoracic surgery clinics from January 2012 to August 2012. During the study period, a total of 136 pulmonary resections were completed (76 lobectomy, 7 segmentectomy, 46 wedge resection, 7 pneumonectomy, 2 cases aborted). A total of 129 cases were eligible for the study, of which 30 patients (23%) entered the study.
A summary of patient demographic characteristics is displayed in Table 1. For this study population, 20 participants were female (66.7%) and 10 male (33.3%). The mean age was 65 (±8) years. All participants who underwent lung resection had a diagnosis of pulmonary neoplasm. Non-small-cell lung cancer was the diagnosis in 28 (93.3%). Pulmonary carcinoid tumour was the diagnosis in 1 (3.3%) and diaphragmatic sarcoma invading lung in 1 (3.3%). A breakdown of procedure details is given in Table 2. The majority of participants underwent pulmonary lobectomy. A total of 3 (10%) underwent segmentectomy, and 1 (3.3%) underwent wedge resection. The procedure was the first thoracic operation for 29 (96.7%) of the participants, and a repeat thoracic operation for 1 (3.3%). The mean length of hospital stay was 6.70 (±4.3) days.
| Patient characteristics . | Value . |
|---|---|
| Gender, n (%) | |
| Male | 10 (33.3%) |
| Female | 20 (66.7%) |
| Mean age (years) | 64.87 (±8.36) |
| Median body mass index (BMI) | 26.03 |
| Diagnosis, n (%) | |
| Lung cancer—NSCLC | 28 (93.3%) |
| Lung cancer—carcinoid | 1 (3.3%) |
| Other cancer | 1 (3.3%) |
| Patient characteristics . | Value . |
|---|---|
| Gender, n (%) | |
| Male | 10 (33.3%) |
| Female | 20 (66.7%) |
| Mean age (years) | 64.87 (±8.36) |
| Median body mass index (BMI) | 26.03 |
| Diagnosis, n (%) | |
| Lung cancer—NSCLC | 28 (93.3%) |
| Lung cancer—carcinoid | 1 (3.3%) |
| Other cancer | 1 (3.3%) |
NSCLC: non-small-cell-lung-cancer.
| Patient characteristics . | Value . |
|---|---|
| Gender, n (%) | |
| Male | 10 (33.3%) |
| Female | 20 (66.7%) |
| Mean age (years) | 64.87 (±8.36) |
| Median body mass index (BMI) | 26.03 |
| Diagnosis, n (%) | |
| Lung cancer—NSCLC | 28 (93.3%) |
| Lung cancer—carcinoid | 1 (3.3%) |
| Other cancer | 1 (3.3%) |
| Patient characteristics . | Value . |
|---|---|
| Gender, n (%) | |
| Male | 10 (33.3%) |
| Female | 20 (66.7%) |
| Mean age (years) | 64.87 (±8.36) |
| Median body mass index (BMI) | 26.03 |
| Diagnosis, n (%) | |
| Lung cancer—NSCLC | 28 (93.3%) |
| Lung cancer—carcinoid | 1 (3.3%) |
| Other cancer | 1 (3.3%) |
NSCLC: non-small-cell-lung-cancer.
| Patient characteristic; descriptor . | Value . |
|---|---|
| Procedure details; n (%) | |
| First time thoracic operation | 29 (96.7%) |
| Re-do thoracic operation | 1 (3.3%) |
| Pleural adhesions | 9 (30.0%) |
| Lobectomy | |
| Right upper lobe | 16 (53.3%) |
| Right middle lobe | 1 (3.3%) |
| Right lower lobe | 3 (10.0%) |
| Left upper lobe | 2 (6.7%) |
| Left lower lobe | 4 (13.3%) |
| Bi-lobectomy | 0 |
| Wedge resection | 1 (3.3%) |
| Segmental resection | 3 (10.0%) |
| Use of intraoperative adjuncts | |
| Peri-Guard buttress strip | 1 (3.3%) |
| Tisseal sealant glue | 0 |
| Patient characteristic; descriptor . | Value . |
|---|---|
| Procedure details; n (%) | |
| First time thoracic operation | 29 (96.7%) |
| Re-do thoracic operation | 1 (3.3%) |
| Pleural adhesions | 9 (30.0%) |
| Lobectomy | |
| Right upper lobe | 16 (53.3%) |
| Right middle lobe | 1 (3.3%) |
| Right lower lobe | 3 (10.0%) |
| Left upper lobe | 2 (6.7%) |
| Left lower lobe | 4 (13.3%) |
| Bi-lobectomy | 0 |
| Wedge resection | 1 (3.3%) |
| Segmental resection | 3 (10.0%) |
| Use of intraoperative adjuncts | |
| Peri-Guard buttress strip | 1 (3.3%) |
| Tisseal sealant glue | 0 |
| Patient characteristic; descriptor . | Value . |
|---|---|
| Procedure details; n (%) | |
| First time thoracic operation | 29 (96.7%) |
| Re-do thoracic operation | 1 (3.3%) |
| Pleural adhesions | 9 (30.0%) |
| Lobectomy | |
| Right upper lobe | 16 (53.3%) |
| Right middle lobe | 1 (3.3%) |
| Right lower lobe | 3 (10.0%) |
| Left upper lobe | 2 (6.7%) |
| Left lower lobe | 4 (13.3%) |
| Bi-lobectomy | 0 |
| Wedge resection | 1 (3.3%) |
| Segmental resection | 3 (10.0%) |
| Use of intraoperative adjuncts | |
| Peri-Guard buttress strip | 1 (3.3%) |
| Tisseal sealant glue | 0 |
| Patient characteristic; descriptor . | Value . |
|---|---|
| Procedure details; n (%) | |
| First time thoracic operation | 29 (96.7%) |
| Re-do thoracic operation | 1 (3.3%) |
| Pleural adhesions | 9 (30.0%) |
| Lobectomy | |
| Right upper lobe | 16 (53.3%) |
| Right middle lobe | 1 (3.3%) |
| Right lower lobe | 3 (10.0%) |
| Left upper lobe | 2 (6.7%) |
| Left lower lobe | 4 (13.3%) |
| Bi-lobectomy | 0 |
| Wedge resection | 1 (3.3%) |
| Segmental resection | 3 (10.0%) |
| Use of intraoperative adjuncts | |
| Peri-Guard buttress strip | 1 (3.3%) |
| Tisseal sealant glue | 0 |
Assessment of pulmonary air leak severity
A total of 128 pulmonary air leak evaluations were completed in 30 patients (thoracic surgeon = 30; nurses = 56; resident = 30; physiotherapists = 12). The mean time between analogue and digital assessment was 2.16 (±1.66) h. Patient position during analogue and digital air leak assessment was constant in 114 (89%). The level of suction applied to the chest drainage device was also constant for 122 (95%) of analogue and digital assessments. Eighteen (13.95%) patients assessed to have an air leak present with the analogue system were subsequently found to have zero air flow (no air leak) on the digital system.
Level of interobserver agreement
The level of agreement overall and stratified for observer subgroups is summarized in Fig. 3. For pulmonary air leak severity, the level of observer agreement overall using the analogue system was slight, with a κ of 0.03 (−0.04, 0.11); P = 0.40. Agreement overall using the digital system was increased to substantial, with a κ of 0.61 (0.49, 0.73); P < 0.01.
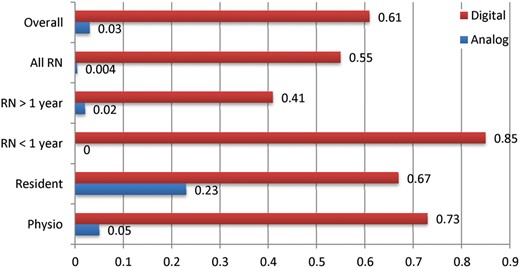
Level of interobserver agreement. κ statistic (0 = change agreement, 1 = perfect agreement). RN: registered nurse; Physio: physiotherapist.
The level of pulmonary air leak severity agreement for all nurses using the analogue system was less than due to chance, with a k of 0.004 (−0.08, 0.09); P = 0.94. The level of observer agreement increased significantly with the use of the digital device to moderate, with a k of 0.55 (0.39, 0.72); P < 0.01. Pulmonary air leak severity agreement for nurses with greater than 1 year of experience using the analogue system was slight, with a k of 0.02 (−0.10, 0.14); P = 0.79, and using the digital system was increased to moderate, with a k of 0.41 (0.20, 0.61); P < 0.01. For nurses with 1 year or less of pulmonary patient experience, level of air leak severity agreement was less than due to chance, with a k of −0.02 (−0.14, 0.09); P = 0.74. When using the analogue system, agreement was almost perfect for this same group of nurses, with a k of 0.85 (0.66, 1.00), P < 0.01, using the digital system.
The level of pulmonary air leak severity agreement for resident physicians using the analogue system was fair, with a k of 0.23 (−0.03, 0.49); P = 0.03. Using the digital system, resident agreement was increased to substantial, with a k of 0.67 (0.45, 0.88); P < 0.01. The level of agreement for physiotherapists using the analogue system was slight, with a k of 0.05 (−0.12, 0.23); P = 0.61, and using the digital system was increased to substantial , with a k of 0.73 (0.40, 1.00); P < 0.01.
Difference in agreement of air leak severity
The difference between values of overall κ for the digital and analogue systems was 0.58; this difference is significant, with P < 0.01. The differences for nurses, residents and physiotherapists separately were also significant at 0.55 (P < 0.01), 0.43 (P = 0.01) and 0.67 (P < 0.01), respectively.
DISCUSSION
The results reveal consistently overall, and separately across multidisciplinary healthcare professional groups assessing pulmonary air leaks, increased levels of agreement in air leak severity assessment using the digital compared with the analogue chest drainage system. This increase in agreement occurred regardless of level of experience in caring for patients with pulmonary air leaks. In particular, the air leak severity assessment of the surgical resident trainees and nurses with less than 1 year of experience with thoracic surgery patients were brought closer to that of the experienced attending thoracic surgeon by the digital system.
The consistently increased level of agreement in air leak assessment with digital chest drainage may overcome several shortcomings of the analogue systems. The means by which this is achieved is through decreased clinical variability [6, 11]. From decreased variability follows facilitation of team understanding and cooperation in execution of pulmonary air leak management algorithms, and avoidance in significant morbidity associated with small or occult air leaks. Each shortcoming of analogue pleural drainage overcome by digital air leak assessment is addressed individually below.
The serious risks associated with provocative chest tube clamping to rule out the presence of occult small air leaks can be avoided with digital chest drainage [6, 14]. The most serious risk of provocative chest tube clamping is tension pneumothorax; however, there is also potential morbidity associated with the uncertain presence of a small, occult air leak on the analogue system. Analogue air leak uncertainty may lead to removal of chest tubes with occult small leaks too early, with resultant recurrent pneumothorax requiring chest tube reinsertion [11]. Alternatively, this uncertainty regarding the presence of a small air leak may lead to delayed chest tube removal with associated morbidity of pain, atelectasis and risk of infection from prolonged chest tube placement [6, 14].
Increased agreement with digital air leak severity assessment may translate to increased cooperation of the multidisciplinary pulmonary care team. The importance of pulmonary care team cooperation and communication in the execution of air leak management patient care algorithms cannot be overemphasized [11]. Conflict usually arises from poor or inconsistent communication. Decreased variability in air leak management clinical practice can give the pulmonary team and the patient consistent peace of mind in knowing who can have chest tubes safely removed, who can plan to be safely discharged from hospital with a Heimlich valve and who requires ongoing in-hospital care [6, 11]. In this way, digital technology decreases variability to streamline communication in the patient care setting, to decrease errors and optimize use of limited health-care resource dollars [6, 15].
Digital chest drainage technology may also be used to streamline communication and agreement in the clinical research setting. In particular, digital air leak monitoring may prove useful in assessing change in air leak severity following placement of an endobronchial valve or application of a fibrin-based sealant [16].
Despite the ability of digital chest drainage to overcome potential shortcomings of analogue systems, there remain important unanswered questions with respect to how to best apply this new technology in patient care. These questions pertain primarily to financial cost of the system and measured air leak thresholds.
A single digital chest drainage system does have an increased unit financial cost compared with a single analogue system. Questions remain as to whether the digital drainage system is financially advantageous following uncomplicated pulmonary resection without air leak [7]. It may be that digital chest drainage is best suited only for patients with air leak, to allow continuous monitoring to inform management. Future clinical research should focus on the topic of utility of digital chest drainage in patients without air leak as well as the safe minimum air flow threshold at which a pleural drain may be removed.
Discussion of study limitations
Potential limitations with the current study arise from fundamental attributes of the κ statistic for assessment of agreement in addition to the study sample size. Although κ is commonly used in assessments of reliability between observers, the validity of the correction for random agreement built into its calculation has been questioned [13]. While random chance agreement may not be the ideal baseline from which to rate observer agreement, any baseline assuming otherwise would require more complicated unnecessary assumptions about observer behaviour. Thus, despite being potentially less than ideal because of underestimation of the probability of random agreement, κ is an easily interpretable statistic.
A lower probability of random agreement will result in a higher κ value, and this potential bias should be considered when reviewing results. However, only a large difference between random guessing and one's ideal probability model would create important differences in calculated κ values.
Comparison of κ values may be somewhat more problematic. The comparisons presented here assume that κ is normally distributed. The reliability of this methodology depends on the sample size. For small samples, it is reasonable to argue that the methodology attributes undue precision to the estimates (narrower confidence intervals), which may lead to findings of significant differences, whereas a more conservative approach correcting for the small sample size would not. As with any exploratory work, the potential lack of precision inherent in any κ analysis should be considered in the interpretation of results.
CONCLUSION
With analogue chest drainage systems, there was lack of interobserver reliability in quantifying pulmonary air leak severity overall following pulmonary resection. Digital pleural drainage technology improved multidisciplinary consistency in the bedside evaluation of pulmonary air leak severity.
ACKNOWLEDGEMENTS
We acknowledge the contributions of the Ottawa Hospital Division of Thoracic Surgery Research Office staff in the execution of this study. We especially express gratitude to Anna Fazakas, Kaitlyn Chambers and Caitlin Anstee for their administrative support.
Conflict of interest: The Thopaz chest drainage devices used in this study were provided on loan to The Ottawa Hospital for the purpose of this study only by the Medela Corporation (Baar, Switzerland). They also provided the pleural drainage tubing and replacement drainage canisters at a discounted rate for the study.
REFERENCES
Author notes
Presented at the CHEST meeting, American College of Chest Physicians, 2013, Chicago, IL, USA.





Comments
© The Author 2015. Published by Oxford University Press on behalf of the European Association for Cardio-Thoracic Surgery. All rights reserved
We read with interest the article by McGuire et al. [1] on the concordance of airleak assessment using digital devices and the analogue system. We think this is a very interesting topic, first of all for its implications on patient management including chest drain stay, hospitalization and air leak management. It also has important implications in terms of cost effectiveness [2].
In the literature, it is noted that digital devices may help clinical practice and reduce chest tube duration, hospitalization and mistakes when used in high volume centres with adequate staff experience [3]. Furthermore, digital systems allow an easier recognition of air leaks compared to analogue devices. It is interesting to note that there is a high variability how young doctors (residents) and non-medical staff recognize air leaks. Therefore, it should be useful to know whether this reflects a different level of experience or a lack of training among staff members. In such a case, an intensive training is warranted for all medical and non-medical staff operating in the thoracic surgical ward. Perhaps, this may allow an unique and standardized way to look at the analogue system and also improve the competencies with the use of digital device. Another point of interest is how one assesses air leaks. Indeed, the analogue device usually allows only an "instant assessment", whereas a digital device enables one to obtain a historical curve and register the precedent hours in order to obtain more information on the air leak trend. In this way, we think this allows for a more objective evaluation of the air leak and is better than a subjective interpretation. The next decision should be taken with sure and undisputable data in order to avoid mistakes in chest tube management.
Based on the data reported, we would really appreciate the Authors' reflections and reaction on the aspects debated.
References
[1] McGuire AL, Petrcich W, Maziak DE, Shamji FM, Sundaresan SR, Seely AJE et al. Digital versus analogue pleural drainage phase 1: prospectiveevaluation of interobserver reliability in the assessment of pulmonary air leaks. Interact CardioVasc Thorac Surg 2015;doi:10.1093/icvts/ivv128.
[2] Varela G, Jimenez MF, Novoa N, Aranda JL. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg 2005;27:329-33.
[3] Pompili C, Detterbeck F, Papagiannopoulos K, Sihoe A, Vachlas K, Maxfield MW et al. Multicenter International Randomized Comparison of Objective and Subjective Outcomes Between Electronic and Traditional Chest Drainage Systems. Ann Thorac Surg 2014;98:490-7
Conflict of Interest:
None declared
© The Author 2015. Published by Oxford University Press on behalf of the European Association for Cardio-Thoracic Surgery. All rights reserved
In recent times, significant resources have been spent - both human and financial - on developing marvellous surgical techniques or innovative technologies, such as robot-assisted or uniportal thoracoscopic surgery [1]. However, if the goal is simply faster patient recovery, then perhaps the most important arena for improvement should not be in the operating room, but on the ward after surgery.
The commonest caused for prolonged hospitalization following pulmonary surgery today is air leakage. Of course, there are many options for managing air leak - ranging from intra-operative sealant use to post-operative chemical pleurodesis. However, all of these techniques have one common final pathway: their success or failure is gauged by the observation of air bubbling through the ubiquitous water seal - one of the crudest assessments in thoracic surgery.
Many confounding variables can influence the observation of bubbling. These include: size of the air leak; tidaling of the water column during breathing (especially with a large residual air space); adequacy of pain control; experience of the observer; and so on. These result in considerable disagreements between observers on whether or not an air leak is present [2]. When considering removal of a chest tube, the clinician is stumped if another observer (say, a night shift nurse or resident) had documented that bubbling a few hours or even minutes earlier. In the real world, many clinicians may err on the side of caution and postpone the removal. In this way, inconsistency in the observation of air leak can lead to hesitancy in drain management, and in turn to prolongation of hospital stay.
In this issue, McGuire et al. report that use of a digital chest drainage system significantly improved inter-observer agreement when assessing air leak compared to a conventional water seal system [3]. This is perhaps intuitive: instead of looking for bubbling (subject to all the above confounding variables), observers read a single number on the digital system - the same number for everybody. This study not only confirms a similar earlier report by Varela et al. [2], but potentially offers an explanation for another important observation about digital chest drainage systems. In 2008, Cerfolio et al. reported that using a digital system may reduce chest drain durations and lengths of stay [4]. More recently, in a randomized trial, Pompili et al. demonstrated that a more modern portable digital system could further reduce durations of air leak, chest drainage, and postoperative stay - all by the same margin of around one day [5]. In other words, earlier determination of air leak cessation seemed to be directly responsible for shorter drainage and hospitalization by the same degree. The reduced air leak duration may be related to the regulated pleural pressure with the digital system. However, an alternative viewpoint suggested by Cerfolio et al. was that improved inter-observer consistency with a digital system may simply allow an earlier agreement on when the air leak had ceased [4]. The current study by McGuire et al. certainly gives further credence to this latter view. The direct causal relationship between improved inter-observer consistency and reduced durations of air leak, chest drainage, and lengths of stay has not yet been proven, but should not be hard to investigate.
Whilst that is eagerly awaited, clinicians should still be reminded of the need for consistency in assessing air leaks. A simple investment of more careful clinical observation may reap greater rewards for expedited patient recovery than spending lavishly on intra-operative extravagance.
References
[1] Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014; 6:S604-S617.
[2] Varela G, Jimenez MF, Novoa NM, Aranda JL. Postoperative chest tube management: measuring air leak using an electronic device decreases variability in the clinical practice. Eur J Cardiothorac Surg 2009; 35:28-31.
[3] McGuire AL, Petrcich W, Maziak DE, Shamji FM, Sundaresan SR, Seely AJE et al. . Digital versus analog pleural drainage phase 1: prospective evaluation of inter-observer reliability in the assessment of pulmonary air leaks. Interactive CardioVasc Thorac Surg 2015; doi: 10.1093/icvts/ivv128.
[4] Cerfolio RJ, Bryant AS. The benefits of continuous and digital air leak assessment after elective pulmonary resection: a prospective study. Ann Thorac Surg 2008; 86:396-401.
[5] Pompili C, Detterbeck F, Papagiannopoulos K, Sihoe AD, Vachlas K, Maxfield MW et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg 2014; 98:490-497.
Conflict of interest:
none declared