-
PDF
- Split View
-
Views
-
Cite
Cite
Marcello Carlo Ambrogi, Carmelina Cristina Zirafa, Federico Davini, Silvia Giarratana, Marco Lucchi, Olivia Fanucchi, Franca Melfi, Alfredo Mussi, Transcollation® technique in the thoracoscopic treatment of primary spontaneous pneumothorax, Interactive CardioVascular and Thoracic Surgery, Volume 20, Issue 4, April 2015, Pages 445–448, https://doi.org/10.1093/icvts/ivu431
Close - Share Icon Share
Abstract
The already low invasiveness of the thoracoscopic treatment of spontaneous pneumothorax may be further reduced by the transcollation® technique. Herein, we report our further experience with a new device, to coagulate blebs and bullae, compared with contrast to endostapler resection.
Data of patients with recurrent or persistent spontaneous pneumothorax, who underwent thoracoscopic treatment, were prospectively collected and reviewed. Those with blebs or bullae (Stages III and IV in accordance with Vanderschueren's classification) were treated with a new device, based on coupling saline solution perfusion with radiofrequency energy. The combination of fluid with radiofrequency allows the sealing of tissue, avoiding charring or burning. Most operations were performed through two 1-cm incisions only.
From 2005 to 2010, 73 patients were treated. These were 59 males (80.8%) and 14 females (19.2%), with a mean age of 27.9 years [standard deviation (SD): 11.7]. Forty-three patients underwent general anaesthesia with selective intubation, 9 awake epidural anaesthesia and 21 spontaneous breathing anaesthesia with laryngeal mask. The mean operation time was 31 min (SD: 10.2). The median postoperative drainage period and hospital stay were 2 days (range of 1–11) and 3 days (range of 2–11), respectively. Prolonged air leak occurred in 1 patient (1.4%). Over a mean follow-up period of 60 months (SD: 22.5), two recurrences (2.7%) were reported.
The transcollation® technique by cold coagulation of blebs and bullae seems to be effective in the treatment of primary spontaneous pneumothorax. Owing to its potential advantages, it appears to be particularly suitable to be associated with awake epidural and LMA anaesthesia.
INTRODUCTION
The main goals of any surgical research should be to increase the efficacy of surgical procedures and to reduce their invasiveness. In the past two decades, video-assisted thoracic surgery (VATS) has clearly achieved both goals in a variety of thoracic procedures, often expanding indications for surgical treatment. One of these paradigmatic cases is the treatment of primary spontaneous pneumothorax (PSP).
There is now a general consensus to treat persistent or recurrent PSP by VATS and, in case of blebs or bullae, to perform stapled bullectomy [1–4].
To further reduce the invasiveness and, above all, the costs of VATS, recent papers have reported on the use of electrosurgical or laser-ablation methods for treatment of spontaneous pneumothorax, in opposition to endostapler resection [5–8]. We also reported, in a previous paper, our preliminary experience with transcollation® technology (previously called ‘cold coagulation’), showing encouraging results [9].
Herein, we report our further experience with this technique, as well as its long-term results.
MATERIALS AND METHODS
We prospectively collected the data of all patients with PSP admitted to our division. The selection criteria of patients treated with the transcollation® technique were as follows: persistent Stage I occurrence or repeated PSP; Stage III/IV blebs or bullae according to Vanderschueren's classification. The first 10 cases were excluded in order to avoid interference in the learning curve. The primary aims of the study were to confirm the feasibility, safety and operative advantages of the procedure. The secondary objective was to assess its efficacy over the long term; thus, only patients with a minimum follow-up of 24 months were included.
Device
The device we utilized to perform the transcollation® technique is a 5-mm endoscopic instrument called EndoFB 3.0 Floating Ball (Salient Surgical Technologies Corporate, Portsmouth, NH). It is widely utilized for liver resections and allows coagulation of blebs and bullae without charring or scar formation when placed into contact with tissue (Fig. 1). This is a saline-cooled radiofrequency-powered device that is connected to a standard operating theatre electrosurgical generator. The coagulation power is typically set to 80–90 W. A sterile 0.9% saline solution bag is connected to the irrigation tubing and adjusted for a drip rate of 4–8 cc/min. The device conducts radiofrequency energy from the generator to the electrode tip, where continuous low-volume saline irrigation cools the contact interface with the lung tissue, keeping surface temperature at 100°C. This avoids the eschar and char formation that occurs with standard electrocautery devices. The thermal energy results in heat denaturation of protein in the wall of blebs and bullae, thereby shrinking these blebs and bullae at their bases, and welding their walls to the underlying lung parenchyma. This phenomenon is called transcollation®. Moreover, vessels and bronchioli afferent to the bulla may be sealed.

Technique
The procedure starts out like a standard thoracoscopic procedure, and is performed under general anaesthesia and single lung ventilation, awake epidural anaesthesia or spontaneously breathing laryngeal mask anaesthesia (LMA), based on the experience of the anaesthesiologist. During LMA anaesthesia, after induction by intravenous infusion of propofol, a laryngeal mask was positioned. Then general inhalatory anaesthesia was performed with sevoflurane. No muscle relaxants were used throughout the procedure, thereby allowing the patient to maintain spontaneous breathing [10].
Two small incisions are made in the axillary triangle: one for the 5-mm thoracoscopic camera, and the other for a 5-mm thoracoscopic instrument. In most cases, if the patients had already a pleural drainage, the chest tube wound was used as one of the two surgical incisions. After exploration, patients with blebs or small bullae, ranging from 5 to 30 mm (Stage III/IV according to Vanderschueren's classification), undergo treatment with the transcollation® technique. It consists of ablation with the Floating Ball, for a few seconds, over the bulla until the bulla's walls shrink over its base and then a little bit around the base itself (Fig. 2). Then, after instillation of saline solution in the pleural space, the lung was inflated to test for air leak.
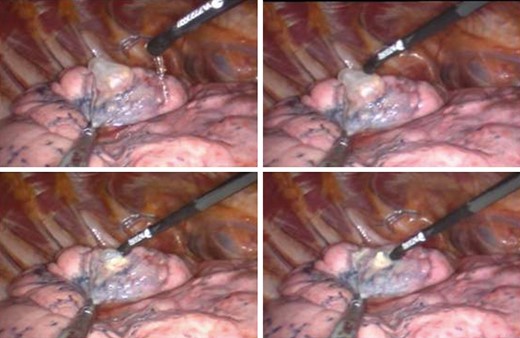
Transcollation technique: setting of perfusion, the tip in contact with the bulla, and coagulation of the bulla and around its base.
With the same device, using the spray mode in order to block saline solution perfusion, it is then possible to perform pleural scarring of the upper hemithorax, as we generally do in the standard technique, after staple bullectomy (Fig. 3). At the end of the procedure, two pleural drainages are inserted through the same operative incisions.
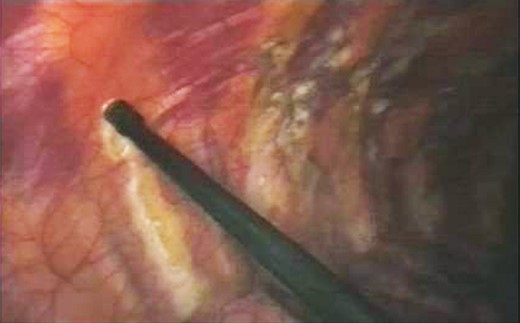
Pleurodesis procedure by hot coagulation (without perfusion) of the parietal pleura over the first eight costal arches.
Data collection and follow-up
Operation time, intraoperative and postoperative complications (prolonged air leak was set over 7 days), postoperative drainage period and hospital stay were prospectively recorded. The follow-up after discharge consisted of an outpatient visit with a new chest X-ray at 30 days, 1 year and 2 years, and then it was by phone.
RESULTS
From 2005 to 2010, 73 patients were treated, these being 59 males (80.8%) and 14 females (19.2%), with a mean age of 27.9 years [standard deviation (SD): 11.7]. Forty-three patients underwent general anaesthesia with selective intubation, 9 awake epidural anaesthesia and 21 spontaneously breathing anaesthesia with laryngeal mask airway. At the end of the procedure, no air leak was noted. The mean operation time was 31 min (SD: 10.2). There was no conversion to thoracotomy in any of the patients. The median postoperative drainage period and hospital stay were 2 days (range of 1–11) and 3 days (range of 2–11), respectively. Prolonged air leak occurred in 1 patient (1.4%), who required reoperation by axillary thoracotomy to suture a tear in the treated area. Over a mean follow-up period of 60 months (SD: 22.5), 2 patients (2.7%) developed a recurrence, after 29 and 37 days, respectively (Table 1). One was treated with pleural drainage, while the second underwent surgical revision by VATS, during which only a few weak pleural adhesions were noted and, notwithstanding that no air leak was revealed, a stapler resection of the previously treated apical sclerotic area of the upper lobe was performed. Pathological examination revealed subpleural dystrophic bullae and fibrosis, thus suggesting an incomplete coagulation of the previous bullous dystrophic area.
| Number of patients | 73 |
| Male:female | 59:14 |
| Mean age (range) | 27.9 years (15–59) |
| Operation time (range) | 31 min (19–78) |
| Drainage period (range) | 2.3 days (1–11) |
| Hospitalization (range) | 3.1 days (2–11) |
| Prolonged air leak (rate) | 1 (1.4%) |
| Recurrence (rate) | 2 (2.7%) |
| Number of patients | 73 |
| Male:female | 59:14 |
| Mean age (range) | 27.9 years (15–59) |
| Operation time (range) | 31 min (19–78) |
| Drainage period (range) | 2.3 days (1–11) |
| Hospitalization (range) | 3.1 days (2–11) |
| Prolonged air leak (rate) | 1 (1.4%) |
| Recurrence (rate) | 2 (2.7%) |
| Number of patients | 73 |
| Male:female | 59:14 |
| Mean age (range) | 27.9 years (15–59) |
| Operation time (range) | 31 min (19–78) |
| Drainage period (range) | 2.3 days (1–11) |
| Hospitalization (range) | 3.1 days (2–11) |
| Prolonged air leak (rate) | 1 (1.4%) |
| Recurrence (rate) | 2 (2.7%) |
| Number of patients | 73 |
| Male:female | 59:14 |
| Mean age (range) | 27.9 years (15–59) |
| Operation time (range) | 31 min (19–78) |
| Drainage period (range) | 2.3 days (1–11) |
| Hospitalization (range) | 3.1 days (2–11) |
| Prolonged air leak (rate) | 1 (1.4%) |
| Recurrence (rate) | 2 (2.7%) |
DISCUSSION
Video-assisted thoracoscopy is the surgical approach of first choice for the treatment of pneumothorax. During VATS, the majority of surgeons perform resection of blebs or bullae by means of an endostapler, although in the last few years various techniques have been employed with the aim to overcome the limits of this procedure. In fact, the utilization of an endostapler may produce greater postoperative pain, because a larger intercostal incision is necessary to introduce the device into the thoracic cavity, with consequent greater trauma. Moreover, resection by stapler may be difficult in the event of a bulla positioned in the pulmonary fissure or on the mediastinal surface of the lung. After resection of bullae or blebs, about 2–9.5% of patients have presented with prolonged postoperative air leak, likely caused by the outflow of air through the suture, while ipsilateral recurrence is seen to be ∼5%, and is induced by the regrowth of bullae around the staple line [11–14].
Therefore, to treat the bullae in patients with pneumothorax, some authors have developed electro-ablation or laser-ablation (argon laser, carbon dioxide laser or Nd:YAG laser) technique, achieving in the last few years satisfactory results with regard to operation times and postoperative pain. Nevertheless, these procedures have seen higher rates of prolonged air leak and recurrence, caused by damage of pulmonary tissue during the ablation, in particular in treatment of pulmonary lesions of 2 cm or more in diameter.
One of these techniques was reported in 2005 by Sawabata et al. [15] , who used an electrosurgical unit with a ball-shaped tip of 8 mm (M-tip) connected to a standard electrosurgical unit, to coagulate residual blebs and bullae after stapler resection of the involved lesions. They reported a low rate of postoperative relapse, but a higher rate of prolonged air leak in the group of patients treated by M-tip electro-ablation, in particular in cases of lesions >2 cm in diameter, than in those patients who underwent only stapled resection of pneumocysts (9.8% vs 2.9%).
Moreover, several studies regarding laser ablation of pulmonary bullae have reported a high incidence of air leaks, resulting from the perforation of lesions when a laser was used during the surgical procedure [7–9, 11–17]. In the experience of Hazama's group, better results were obtained, probably because bullous lesions of <2 cm in size were selected for treatment by endoscopic Nd:YAG laser [8]. Further, during laser ablation it was observed that the over-abrasion of the lung is capable of causing severe bleeding.
With the transcollation® technique, we have obtained a lower percentage of patients with prolonged postoperative air leak and recurrence, because the transcollation® technology preserved continuity of the visceral pleura. In fact, the device, by the combined action of radiofrequency energy and continuous saline solution perfusion, produces the collapse of bullae walls without scarring and desiccation, because the temperature is maintained at about 100°C or below. During the surgical procedure, it is important to maintain an appropriate and continuous irrigation with saline solution to avoid damage to pulmonary tissue. In our opinion, this is the reason why EndoFB is effective in removing bullae, stopping current air leak and avoiding postoperative air leak.
Radiofrequency energy, produced by a special generator, has also been utilized by Linchevskyy et al. [18] in the treatment of patients with pneumothorax, but obtaining as a result, despite a lower operating temperature (∼65°C), a higher rate of recurrence, probably due to a lack of continuous irrigation with saline solution during coagulation.
The endoscopic instrument represented by the Floating Ball device requires only two small surgical incisions, having tiny diameters, and was a reason for our patients experiencing only minor pain in the days following the operation. This device, in addition, is extremely flexible, enabling surgeons to arrive at any area of the pulmonary parenchyma to perform bullae coagulation, as well as, by blocking saline solution perfusion, to easily carry out pleurodesis through electrocoagulation of the first eight costal arches. Moreover, owing to its facility of use, it makes it possible to perform the surgical procedure with spontaneous breathing laryngeal mask anaesthesia or under awake epidural anaesthesia [10, 19].
This study has several weaknesses, the most significant of which are the absence of a comparative group and randomization. Despite that, it seems to confirm that the technique using the EndoFB system is easy, quick and safe to perform during thoracoscopy, representing a possible alternative to pulmonary resection by conventional endostapler for the treatment of spontaneous pneumothorax. The advantages of each of these techniques must be weighed, although those of the former over the latter seem to include the following: (i) a lower level of invasiveness of the procedure, which can also be more quickly performed; (ii) a greater ease of surgical manipulation of the devices; (iii) does not involve the introduction of foreign bodies and (iv) is potentially a source of cost saving (especially in cases of multiple blebs and bullae where several staple cartridges would have to be used in the endostapler treatment).
Further experience by other surgeons in other centres and, above all, randomized controlled trials should certainly be appropriate in order to better assess its effectiveness and utility.
Conflict of interest: none declared.




