-
PDF
- Split View
-
Views
-
Cite
Cite
Tanina Rolf, Juan F. Iglesias, Piergiorgio Tozzi, Ludwig K. von Segesser, Acute myocardial infarction caused by coronary embolization of a papillary fibroelastoma of the thoracic ascending aorta, Interactive CardioVascular and Thoracic Surgery, Volume 11, Issue 5, November 2010, Pages 676–678, https://doi.org/10.1510/icvts.2010.244772
Close - Share Icon Share
Abstract
Papillary fibroelastomas (PFE) are benign endocardial masses and generally originate from the cardiac valves, while PFE arising from the ascending thoracic aorta are an uncommon clinical finding. We report the case of a 78-year-old female who presented to the emergency department with an acute ST segment elevation myocardial infarction. Urgent coronary angiography showed no significant coronary artery obstructive disease but left ventriculography revealed the presence of a highly mobile mass located in the proximal portion of the ascending thoracic aorta. We postulated that the clinical symptoms were caused by embolization from the aortic mass and surgical excision of the peduncle was performed. Histopathological examination revealed a PFE with thrombotic material. Nowadays, surgical excision of PFE remains, the treatment of choice for symptomatic patients with excellent short- and long-term results but recurrence of PFE following surgical excision has not been reported.
Primary tumors of the aorta are a very rare clinical entity and mostly consist of malignant tumors [1]. Papillary fibro-elastomas (PFE) are benign endocardial tumors usually arising from the cardiac valves, while PFE primary located in the aorta are extremely uncommon [1, 2]. The clinical presentation of aortic tumors is mainly related to peripheral embolization from the primary mass and includes stroke, transient ischemic attack and myocardial infarction [1]. Here, we aimed to report the unique case of an acute myocardial infarction secondary to the embolization into a coronary artery of a PFE arising from the ascending thoracic aorta that was successfully treated by surgical resection.
A 78-year-old female with no known history of coronary artery disease presented to the emergency department complaining of typical acute chest pain. The electrocardiogram showed ST segment elevation in the inferior leads and routine laboratory testing confirmed serum cardiac troponine elevation. Urgent coronary angiography showed no significant coronary artery obstructive disease. After contrast injection in the right coronary artery (RCA) a myocardial blush was noted in the distal part (Fig. 1b ), suggesting the transient occlusion and spontaneous reperfusion of the coronary artery. Left ventriculography demonstrated a moderate left ventricular systolic dysfunction with inferior hypokinesia and an unexpectedly large and highly mobile filling defect located in the proximal portion of the ascending thoracic aorta (Fig. 1a). Urgent transthoracic echocardiography confirmed global and segmental left ventricular dysfunction and the presence of a mobile element in the ascending portion of the thoracic aorta. We postulated that the clinical symptoms and signs of acute myocardial ischemia were caused by embolization into the RCA from a highly mobile aortic mass and a surgical revision was recommended.
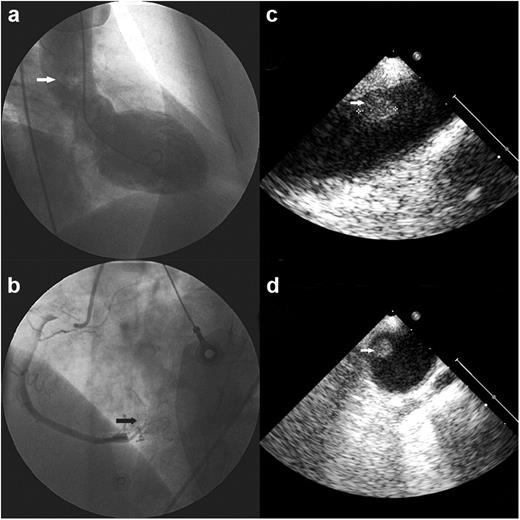
Selective angiography of the right coronary artery in a left anterior oblique angiographic view (b) demonstrates after contrast injection the presence of a myocardial blush (arrow), suggesting the transient occlusion and spontaneous reperfusion of the coronary artery. Left ventriculography in a right anterior oblique angiographic view (a) shows a moderate left ventricular systolic dysfunction with inferior hypokinesia and moderate mitral regurgitation. Visualization of the ascending thoracic aorta during ventriculography reveals an unexpectedly large filling defect (arrow) located in the proximal ascending portion of the thoracic aorta, without evidence of aortic dilatation or valvular regurgitation. Intraoperative transesophageal echocardiography in midesophageal ascending thoracic aorta long- (c) and short-axis (d) views demonstrates a circular, homogenous and echogenic mass (arrows) of ∼1 cm in diameter attached to the wall of the ascending aorta at the level of the distal aortic arch and proximal descending thoracic aorta junction.
Intraoperative transesophageal echocardiography (Fig. 1c) demonstrated a circular and echogenic mass of ∼1 cm in diameter located in the ascending aorta at the level of the distal aortic arch and proximal descending thoracic aorta junction. The patient underwent an aortotomy under cardiopulmonary bypass and intraoperative inspection of the thoracic ascending aorta demonstrated a gelatinous tissue covering the aortic wall and a small peduncle located on the posterior wall of the ascending aorta (Fig. 1d). Surgical excision of the peduncle (Fig. 2 ) was performed and histopathological examination confirmed the diagnosis of a PFE with thrombotic material. Immediate postoperative evolution was complicated by a transient left sensory and motor hemisyndrome without evidence of an acute ischemic lesion as confirmed by a cerebral CT-scan. The patient subsequently reported complete disappearance of the neurological symptoms and was discharged without any new complication two weeks later.
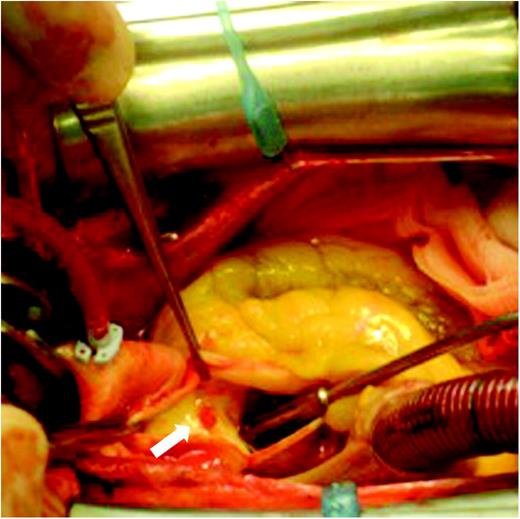
After an aortotomy under cardiopulmonary bypass, intraoperative inspection of the thoracic ascending aorta reveals a gelatinous tissue covering the aortic wall and the presence of a small peduncle located on the posterior wall of the ascending aorta (arrow).
Primary tumors of the aorta are extremely rare, mostly consisting in malignant sarcomas [1, 3, 4]. Benign aortic tumors are even more uncommon and usually correspond to myxomas [1]. PFE are the second most frequent primary tumor of the heart and usually arise from the cardiac valves, particularly the aortic valve in almost half of the cases [2]. Non-valvular locations of PFE are very infrequent, mostly originating from the endocardium of the cardiac chambers [2], while PFE arising from the thoracic ascending aorta, as described here, are extremely rare. The clinical presentation of aortic tumors depends upon the anatomical location of the aortic mass and is related to embolic events from the primary lesion [1, 3, 4]. Interestingly, for the first time to our knowledge, we reported here the unique case of an acute myocardial infarction caused by the thrombo-embolic occlusion of a coronary artery from a PFE of the thoracic ascending aorta. Further complications, such as sudden death, heart failure, syncope or systemic embolic events, have also been described [1, 3]. PFE, however, remain asymptomatic a third of the cases and identification of these masses before the initial clinical presentation is a difficult challenge. Although intra-aortic biopsy is feasible [3], nowadays, surgical exploration and excision of aortic tumors remains the treatment of choice with excellent short- and long-term results for benign masses, while malignant tumors are associated with an elevated short-term mortality usually because of a late diagnosis [4].
Presented at the 24th Annual Meeting of the European Association for Cardio-thoracic Surgery, Geneva, Switzerland, September 11–15, 2010.
References
- myocardial infarction, acute
- aorta
- st segment elevation myocardial infarction
- coronary angiography
- coronary arteriosclerosis
- cardiac papillary fibroelastoma
- heart valves
- endocardium
- ascending aorta
- embolization
- descending thoracic aorta
- emergency service, hospital
- left ventriculography
- thrombus
- excision
- histopathology tests




