-
PDF
- Split View
-
Views
-
Cite
Cite
David J. Birnbaum, Xavier Benoit D'Journo, Dominique Casanova, Pascal A. Thomas, Necrotizing fasciitis of the chest wall, Interactive CardioVascular and Thoracic Surgery, Volume 10, Issue 3, March 2010, Pages 483–484, https://doi.org/10.1510/icvts.2009.222323
Close - Share Icon Share
Abstract
Necrotizing fasciitis (NF) is an uncommon infection caused by microorganisms called ‘flesh eating bacteria’. It remains a life-threatening condition associated with high mortality rate. Its location to the chest wall is exceptional. Herein, we report the case of a 39-year-old female, without comorbidity, presenting a NF of the chest wall complicating an empyema. We describe the surgical management with a three-step procedure: antibiotherapy-debridement, vacuum-assisted closure and delayed surgical reconstruction.
1. Introduction
Necrotizing fasciitis (NF) is a bacterial derma-hypodermitis affecting the soft tissue and muscular fascia. It is an uncommon and severe infection caused by microorganisms called ‘flesh eating bacteria’, mainly represented by group A beta-haemolytic streptococcus. NF remains a life-threatening condition associated with a high mortality rate [1–3]. Its location to the chest wall is extremely rare. The few reported cases are subsequent to thoracic drainage, lung surgery or esophageal resection [1, 3]. Here, we report the case of a NF of the chest wall complicating an empyema. We describe the surgical management over several weeks based on a three-step procedure: 1) appropriate antibiotics and surgical debridement, 2) negative pressure wound therapy [vacuum-assisted closure (VAC®)] and 3) delayed surgical reconstruction.
2. Case report
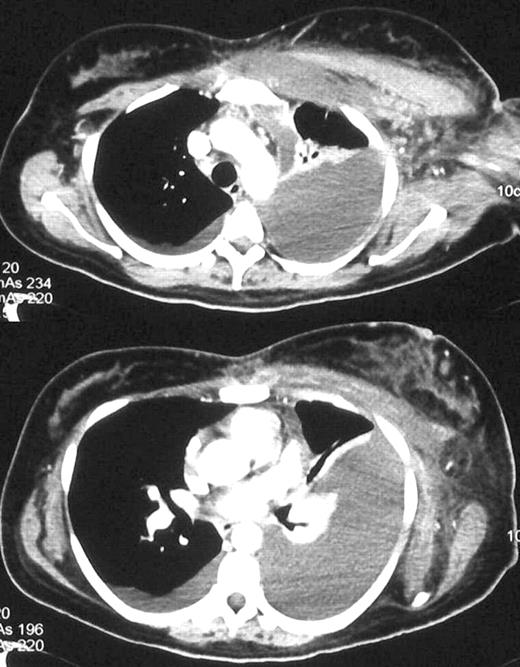
A 39-year-old lady, without comorbidity, was admitted to the intensive care unit for an acute respiratory failure and severe sepsis requiring mechanical ventilation. An antibiotic treatment was begun based on tazocilline and gentamycine. Clinical examination found a thickening of the left axillary region without subcutaneous emphysema and a left pleural effusion. A computed tomography scan confirmed the pleural effusion with a pneumonia of the left lower lobe. After a few hours, the patient developed a NF of the left axillary area. Emergency surgical debridement was required. A wide section was performed on the medio-axillary line with subcutaneous and muscular debridement. After abundant irrigation, large drainage was positioned in the subcutaneous tissue. Culture demonstrated group A beta-haemolytic streptococcus leading to a targeted bi-antibiotic treatment (tazocilline and rifadine). Within a few days, the patient felt well and was extubated. On postoperative day 15, all drains were removed and the patient was referred to a medical department with a negative pressure wound therapy (VAC®, KCI Inc, San Antonio, TX). After two weeks, despite general improvement, surgical debridement resulted in full-thickness axillary defect with a multiloculated pleural effusion (Figs. 1 and 2a ). A pleural decortication and a reconstructive surgery were decided in collaboration with plastic surgeons. The patient was operated on 35 days after her admission, when she was hemodynamically stable and apyretic without signs of infection. An active granulation tissue was achieved in the wound (Fig. 2a). With the patient in left lateral decubitus, an extensive debridement of all non-viable tissues of the antero-lateral thoracoabdominal wall (serratus anterior) was performed. The pleural cavity was opened for decortication and large chest tube drainage were inserted. A left latissimus dorsi free flap for filling and covering the defect (Figs. 2b and c) was raised. The coverage was completed with a transplant of non-pediculized skin taken from the right thigh. The postoperative outcome was uneventful and the patient was discharged home at day 50. Twenty-three months after the reconstruction the patient had no complaint and she had no recurrence of the disease (Fig. 2d).

(a) Granulation of soft tissues after two weeks of VAC® therapy. (b) Extensive debridement of all nonviable tissues (serratus anterior). Left latissimus dorsi free flap for filling and covering the defect. (c) Coverage with a transplant of non-pediculized skin. (d) Results after 23 months of the reconstruction.
3. Discussion
NF is a rare infection, seen most frequently in the immuno-compromized patients and associated with a high mortality rate [1]. The infection mostly occurs along the lowest part of the body and much more rarely to the chest wall [1, 2]. The thoracic location is most frequently reported after chest drainage or after thoracic surgery. However, contagions from empyema have been reported [1–3]. Group A beta-haemolytic Streptococcus and Clostridium perfringens are the most common pathogens found in this pathology. However, multi-microbial associations are reported [1].
Early diagnosis and treatment are the two main factors responsible for the prognosis [1]. The antibiotic treatment must be started immediately, even before the results of the microbiological analyses. Antibiotics are usually adjuvant to the surgical treatment because the local vascular thrombosis results in poor antibiotic tissue diffusion. The objective of the antibiotic treatment is to limit the progression of the infection. The recommended antibiotic treatment consists in the association of β-lactamine, imidazole±aminoside.
There is no cure without complete excision of the non-viable tissues. The additional use of a negative pressure wound therapy (VAC®) for management of NF of the chest wall has been recently reported with success [4]. Its use allows drainage of secretions, improves microcirculation development and favours tissue granulation. Delayed parietal reconstruction is justified when full-thickness defect is present. The use of latissimus dorsi free flap seems to be the reconstructive technique of choice with good esthetical and functional results [5].
To summarize, aggressive surgery and antibiotics form the basis for the treatment of NF of the chest wall. Adjuvant use of negative pressure wound therapy seems to be a promising option in order to improve tissue quality before reconstructive surgery.




