-
PDF
- Split View
-
Views
-
Cite
Cite
Oruganti Sai Satish, Kuan-Hung Yeh, Ming-Shien Wen, Chun-Chieh Wang, Focal right ventricular tachycardia originating from the subtricuspid septum, EP Europace, Volume 7, Issue 4, 2005, Pages 348–352, https://doi.org/10.1016/j.eupc.2005.02.122
Close - Share Icon Share
Abstract
Ventricular tachycardia originating from the right ventricular septum is very uncommon. In a 54-year-old male patient with right ventricular tachycardia, the focus of the ventricular tachycardia was localized to the subtricuspid septum of the right ventricle, which could be successfully eliminated with radiofrequency catheter ablation. The patient's echocardiogram and coronary angiogram were normal. The available literature on idiopathic right ventricular tachycardia is reviewed.
Introduction
In the absence of structural heart disease, ventricular tachycardia (VT) is called idiopathic [1] . The majority of idiopathic right ventricular tachycardia (IRVT) originates in the right ventricular outflow tract (RVOT) and rarely from the inflow, free wall [2] , or apex [3] of the right ventricle (RV). IRVT originating from the RV septum is very uncommon. We present here an interesting case history of a patient who had focal VT originating from the subtricuspid septum of the RV and successful radiofrequency (RF) ablation of the VT focus. The existing literature on IRVT is discussed.
Case history
A 54-year-old male patient was admitted to this University hospital with a history of palpitations on heavy exertion for the last 10 years. The frequency and duration of the palpitations had worsened in the last 2 years. He was not a known diabetic or hypertensive. He was a chronic smoker and there was no family history suggestive of coronary artery disease.
Clinical examination was unremarkable. Twelve lead electrocardiogram (ECG) at rest showed normal sinus rhythm and premature ventricular complexes (PVCs) of left bundle branch block (LBBB) morphology. Holter recording showed that 34% of the total beats were PVCs of LBBB morphology with frequent bigeminy and trigeminy. Two-dimensional echocardiography showed normal cardiac chambers with good biventricular function. He was subjected to treadmill exercise testing using the Bruce protocol. He achieved a workload of 13.5 METs. During the first minute of recovery, he developed sustained VT of LBBB morphology with left axis, which lasted for 3 min. There were no significant ST segment or T wave changes suggestive of myocardial ischaemia. In view of his age and chronic history of smoking, he was subjected to a coronary angiogram (CAG) which showed normal epicardial coronary arteries.
Electrophysiological study (EPS) – After informed written consent, the patient was subjected to EPS and RF ablation under fentanyl and midazolam sedation. Two 6F quadripolar and one 6F decapolar electrode catheters were introduced percutaneously into the right femoral vein and advanced under fluoroscopic guidance to the right atrial appendage, the apex of the RV (quadripolar) and across the tricuspid valve for recording of the His bundle electrogram (decapolar). Programmed electrical stimulation was performed using up to three extrastimuli at two basic cycle lengths of 600 and 400 ms from RV apex and RVOT using twice diastolic pacing threshold (2 ms pulse duration). As no VT could be induced, the patient received an isoprenaline infusion 1 μg/min with increments to reach 5 μg/min. Programmed electrical stimulation was repeated at each isoprenaline dose. As no sustained VT could be induced, the patient was given atropine 1 mg intravenously, resulting in the development of spontaneous wide QRS tachycardia of LBBB morphology with a cycle length of 357 ms, axis of −110° with atrioventricular dissociation ( Fig. 1 ). This tachycardia was similar to the clinical VT. The ablation catheter (7F, distal electrode length 4 mm, Celsius, Biosense Webster, Diamond Bar, CA, USA) was introduced through the right femoral vein and the earliest endocardial activation site preceding the QRS (−56 ms) was mapped at the subtricuspid septum of the RV during VT ( Fig. 2 ). RF energy of 30–40 W with 60 °C temperature from an electrosurgical unit (OSYPKA HAT 300, Rheinfeldon–Herten, Germany) was delivered at this site ( Fig. 3 ) for 60 s. Tachycardia was terminated at 15 s but energy delivery was continued up to 60 s. During the observation period, PVCs of LBBB morphology that were similar to the clinical tachycardia were intermittently seen. Pace mapping was performed with the ablation catheter and RF energy was delivered three more times at the same site in the subtricuspid septum of the RV with exact QRS pace-map (in all 12 surface ECG leads) matched to the ectopic QRS. Programmed electrical stimulation was repeated with and without isoprenaline. No clinical VT or ectopy could be induced.
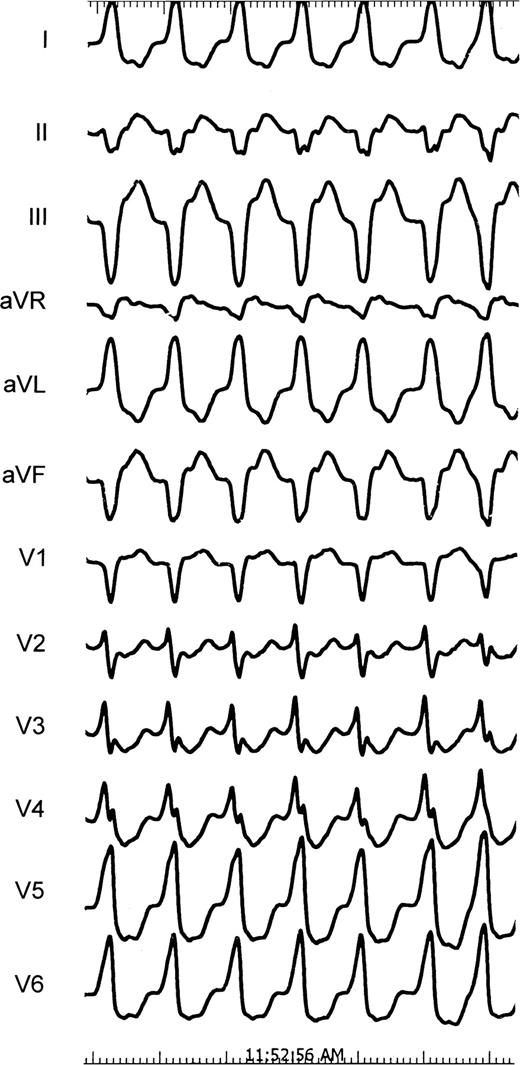
Twelve lead ECG recorded (speed 25 mm/s) during electrophysiological study showing ventricular tachycardia of left bundle block morphology with left axis deviation.
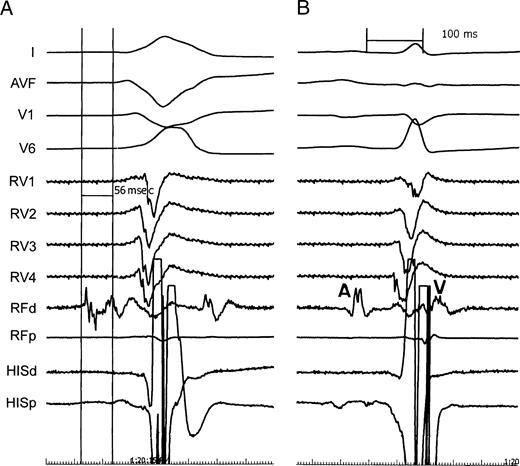
(A) Earliest endocardial activation recorded by the ablation catheter at the successful ablation site in the subtricuspid septum of the right ventricle. (B) Atrial (A) and ventricular (V) electrograms recorded by the ablation catheter at the right ventricular septum after successful radiofrequency ablation of the ventricular tachycardia focus.
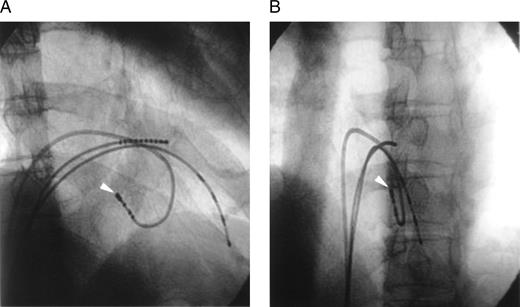
Fluoroscopic images obtained in the right anterior oblique (A) and left anterior oblique (B) projections (30°) showing the successful ablation site. The distal electrodes of the ablation catheter (arrow) are positioned at the subtricuspid septum of the right ventricle.
Holter recording following the RFA procedure showed only one PVC and occasional atrial premature complexes in the entire 24 h of ECG recording. Treadmill exercise test 3 days after the procedure did not provoke PVCs or VT. The patient was free of symptomatic palpitations at 6 months of follow-up.
Discussion
IRVT originating from RV septum is very rare. In 1981 Vetter et al. [4] described the results of EPS in seven children with idiopathic VT. Among them, an 18-year-old had VT of right bundle block morphology with an axis of −100° and the VT focus was localized to the RV mid septum. In view of normal haemodynamic and angiocardiographic studies, the VT was labelled as idiopathic. In comparison, our patient was an adult with LBBB morphology VT, which is typical of VT originating from the RV, and his echocardiogram and CAG were normal, probably also suggesting an idiopathic aetiology. The VT focus was successfully eliminated by RF ablation.
Idiopathic VT originating from the right inflow tract or apex has similar electrophysiological characteristics to that of idiopathic RVOT tachycardia [5] . Idiopathic RVOT tachycardia is present in one of two forms: repetitive monomorphic VT or paroxysmal exercise induced sustained VT. Repetitive monomorphic VT is characterised by frequent ventricular extrasystoles, couplets, and salvos of non-sustained VT interrupted by brief periods of sinus rhythm. In contrast, paroxysmal exercise induced VT, which can also be precipitated by emotional stress, is a sustained arrhythmia [6] . The data suggest that these two forms represent polar ends of the spectrum of idiopathic VT due to cyclic-AMP mediated triggered activity with considerable overlap between them [7] . Patients with paroxysmal exercise induced VT can have frequent salvos of non-sustained VT and patients with repetitive monomorphic VT may have sustained VT induced during catecholamine infusion or programmed electrical stimulation [6] . The patient in this report had overlapping features of the two forms.
Klein et al. [2] in their study of idiopathic VT in 14 patients noted a VT focus near the His bundle in three patients. ECG during VT showed LBBB morphology with normal axis. They concluded that ECG morphology during VT did not predict the successful RF ablation site.
Patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) can also present with VT of LBBB morphology, which needs to be differentiated from IRVT, as the course of the disease and prognosis are totally different in the two conditions. Echocardiography may show morphological changes in the RV in patients with ARVC/D. Our patient had a normal echocardiogram. Magnetic resonance imaging (MRI) of the heart may detect early cases of ARVC/D where echocardiography may be normal [8] . The present patient did not undergo MRI of the heart. However, the VT focus in this patient was localized to the subtricuspid septum and involvement of the RV septum by ARVC/D is very uncommon [9] . Invasive EPS can differentiate ARVC/D and idiopathic RVOT tachycardia. Arrhythmia induction with programmed electrical stimulation, fragmented electrograms, and more than one form of inducible VT favours ARVC/D as the underlying aetiology. In contrast, idiopathic RVOT tachycardia patients show induction of VT with isoprenaline, single morphology of VT and rarity of fragmented electrograms [10] . Our patient also had inducible monomorphic VT with isoprenaline and there were no fragmented electrograms, probably suggesting VT of idiopathic origin.
Antiarrhythmic drug therapy with sotalol, flecainide, and verapamil has been tried in patients with IRVT with variable success [11] . However, catheter ablation is the treatment of choice in relatively young but symptomatic patients with idiopathic VT, eliminating the drawbacks of long-term antiarrhythmic therapy even when control of the arrhythmia is achieved [12] . Early endocardial activation time at the successful ablation site, use of both activation and pace mapping for ablation has shown less recurrence during follow-up in patients with idiopathic VT [13] . Our patient also had early endocardial activation time (56 ms) at the target site and both activation and pace mapping were used for successful ablation of the VT and PVC focus. The prognosis of patients who have VT without apparent structural heart disease is believed to be good, but rare cases of sudden death have been recorded [14] .
In conclusion, we have described a case of focal VT originating from the subtricuspid septum of the RV, which is very rare and successful RFA of the VT focus.



