-
PDF
- Split View
-
Views
-
Cite
Cite
T Oezkartal, G Conte, A Breitenstein, A Haeberlin, C Sticherling, P Ammann, C Grebmer, A D'alto, L Schoeni, J Bruno, M Bergonti, M L Caputo, C Klersy, A Auricchio, Impact of comorbidities on survival and complications in patients implanted with leadless pacemakers: a national, multicenter study, EP Europace, Volume 26, Issue Supplement_1, May 2024, euae102.402, https://doi.org/10.1093/europace/euae102.402
Close - Share Icon Share
Abstract
The number of leadless cardiac pacemaker (LCP) implantations has increased over the recent years, being more frequently performed in elderly patients with multiple comorbidities.
The aim of this study is to analyze periprocedural complications and outcome of LCP patients according to their comorbidity status.
This is a Swiss multi-centre, retrospective cohort study including all consecutive patients implanted with a LCP (Medtronic Micra VR or AV) between 2015 and 2022. Charlson Comorbidity Index (CCI) was determined and patients were divided into two groups: CCI ≤ 5 (low comorbidity) and CCI > 5 (high comorbidity). Periprocedural complications, in-hospital death, and all-cause mortality were assessed.
A total of 863 patients (median age 81 years (IQR 76 – 86), male sex 65%) were included in the study, of which 58% had a CCI ≤ 5. Baseline characteristics of the 2 groups are summarized in the table. Patients in the high comorbidity group were older male presenting more frequently with ischemic cardiomyopathy, diabetes, chronic obstructive pulmonary disease, moderate to severe chronic kidney disease and malignancies. Urgent implantations were more frequent in the high comorbidity than in the low comorbidity group (65% vs. 50%, p<0.001). Overall periprocedural complication rate was 2.9% (n = 25) without significant differences between the two groups (2.9% in both groups, p = 1.0). Pericardial effusion requiring pericardiocentesis was the most frequent periprocedural complication (n = 8, 0.9%). Median hospitalization was significantly longer (5 vs. 3 days, p<0.001), and in-hospital mortality significantly higher (3.6% vs. 0.6%, p=0.002) in the high comorbidity group. None of the in-hospital deaths was deemed a periprocedural complication. Median follow-up was 15.4 months. As shown in the figure, all-cause mortality was significantly higher in the high morbidity group (HR 2.9, 95%-CI 2.2-3.8, p<0.001) resulting in a mortality of 58% at 3 years.
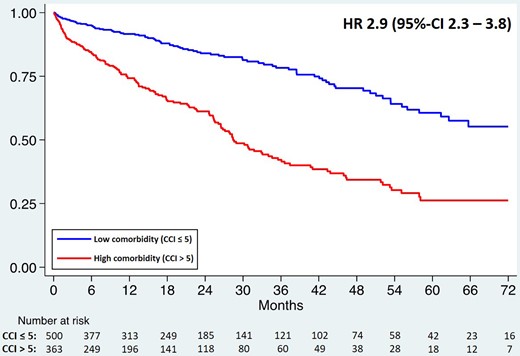
Figure - Survival estimate according CCI
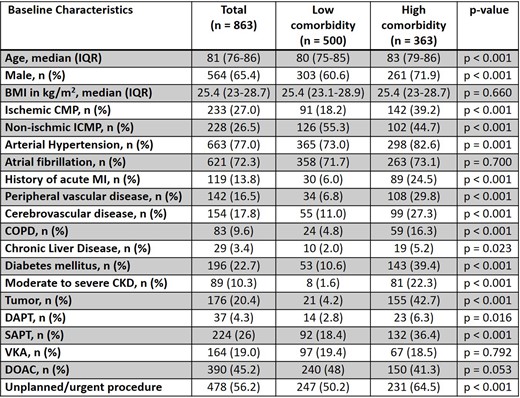
Table - Baseline characteristics
Author notes
Funding Acknowledgements: Type of funding sources: Private company. Main funding source(s): Medtronic
- artificial cardiac pacemaker
- pericardial effusion
- pericardiocentesis
- cardiac transvenous pacemaker
- diabetes mellitus
- chronic obstructive airway disease
- kidney failure, chronic
- ischemic cardiomyopathy
- diabetes mellitus, type 2
- cancer
- comorbidity
- follow-up
- hospital mortality
- life expectancy
- heart
- morbidity
- mortality
- older adult
- cost-effectiveness analysis
- implantation procedure



