-
PDF
- Split View
-
Views
-
Cite
Cite
B Corica, G F Romiti, M Proietti, D A Mei, G Boriani, W Y Ding, B Olshansky, M V Huisman, G Y H Lip, Early rhythm control in patients with recently diagnosed atrial fibrillation: findings from the GLORIA-AF Registry Phase III, EP Europace, Volume 26, Issue Supplement_1, May 2024, euae102.066, https://doi.org/10.1093/europace/euae102.066
Close - Share Icon Share
Abstract
Early rhythm control (ERC) can improve outcomes in select patients with atrial fibrillation (AF) but real-world data are lacking.
To evaluate the effectiveness of ERC in a real-world cohort of AF patients.
From the global, prospective GLORIA-AF Phase III Registry, adult patients with recent diagnosis (< 3 months and < 4.5 months in Latin America) of AF and CHA2DS2-VASc score ≥1 were included. ERC was defined as treatment with an antiarrhythmic drug, catheter ablation, or cardioversion at the baseline. Multivariable logistic regression analysis determined the odds of receiving ERC and an oral anticoagulant [OAC] with results reported as adjusted Odds Ratio (aOR) and 95% Confidence Intervals (95%CI). Risk of major outcomes was determined using multiple Cox regression analyses. The primary outcome was a composite of all-cause death and major adverse cardiovascular events (MACE). Secondary outcomes included all-cause death, thromboembolism and major bleeding. Results were reported as adjusted Hazard Ratio (aHR) and 95%CI.
21,051 AF patients (age: 70.2±10.3, 45% female) were included. Of these, 6,932 (32.9%) received ERC, while 14,119 (67.1%) did not. Patients receiving ERC were younger with a higher prevalence of paroxysmal AF (62.8% vs. 53.2%) and heart failure (23.1% vs. 21.4%). They were less likely to have prior stroke/transient ischemic attack (TIA), chronic obstructive pulmonary disease (COPD), and they had a lower mean CHA2DS2-VASc score (3.0±1.5 vs. 3.3±1.5). Age ≥75 [aOR: 0.53; 95%CI (0.0.49-0.57)] and age 65-75 [aOR: 0.76; 95%CI (0.70-0.82)] were associated with lower odds of receiving ERC. Those with prior stroke/TIA [aOR: 0.55; 95%CI (0.50-0.61)] and COPD [aOR: 0.82; 95%CI (0.71-0.94)], as well as patients with more sustained form of AF and patients recruited in North America were less likely to receive ERC. Conversely, female sex, higher symptom burden, hypertension and coronary artery disease were associated with higher odds of receiving ERC (Figure 1). Patients who received ERC were more likely to receive OACs [aOR: 1.36; 95%CI (1.25-1.48)].
Survival curve for the primary outcome according to ERC are shown in Figure 2. During a median follow-up of 3.0 [IQR: 2.9-3.1] years, ERC was associated with lower risk of the primary composite outcome (aHR: 0.88, 95% CI:0.80-0.96, p=0.006); Similar results were observed for the secondary outcomes.
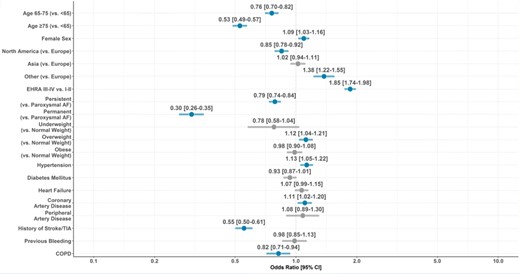
Odds Ratios to be treated with ERC.
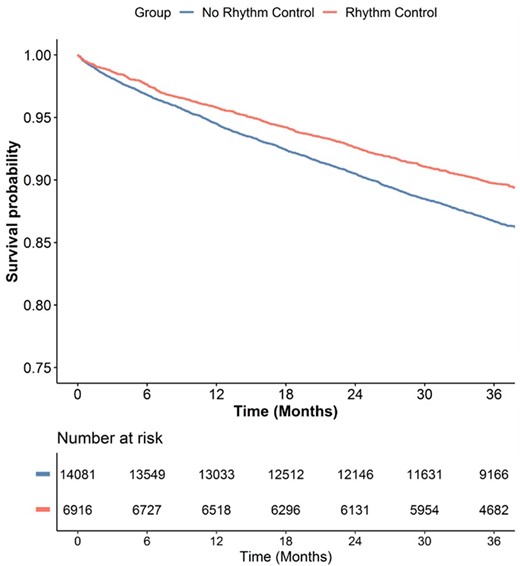
Survival curve.
Author notes
On behalf of GLORIA-AF Investigators
Funding Acknowledgements: Type of funding sources: Private company. Main funding source(s): This publication is based on research using data from data contributors Boehringer Ingelheim that has been made available through Vivli, Inc. Vivli has not contributed to or approved, and is not in any way responsible for, the contents of this publication. This study was funded by Boehringer Ingelheim. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents.
- anti-arrhythmia agents
- atrial fibrillation
- anticoagulants, oral
- hypertension
- transient ischemic attack
- coronary arteriosclerosis
- electric countershock
- thromboembolism
- chronic obstructive airway disease
- cardiac ablation
- hemorrhage
- cerebrovascular accident
- ischemic stroke
- heart failure
- adult
- follow-up
- latin america
- diagnosis
- risk reduction
- cardiovascular event
- survival curve
- cox proportional hazards models
- rhythm
- cha2ds2-vasc score
- primary outcome measure
- composite outcomes
- symptom burden



