-
PDF
- Split View
-
Views
-
Cite
Cite
Massimo Grimaldi, Federico Quadrini, Nicola Caporusso, Federica Troisi, Nicola Vitulano, Vito Delmonte, Antonio Di Monaco, Deep sedation protocol during atrial fibrillation ablation using a novel variable-loop biphasic pulsed field ablation catheter, EP Europace, Volume 25, Issue 9, September 2023, euad222, https://doi.org/10.1093/europace/euad222
Close - Share Icon Share
Abstract
Pulsed field ablation (PFA) is a novel, largely nonthermal ablative modality that, by virtue of its putative preferential action on myocardial tissue through the process of irreversible electroporation (IRE), may replace conventional thermal ablation for atrial fibrillation (AF). The recent inspIRE study confirmed safety and effectiveness of a fully integrated biphasic PFA system with a variable loop circular catheter for the treatment of paroxysmal AF. The majority of PFA procedures were performed using general anesthesia. However, due to the risks of general anesthesia we report the data regarding our sedation protocol used during inspIRE study.
A total of 29 patients (mean age 55±9 years; 72% male) were enrolled as part of this analysis within the inspIRE trial. The sedation protocol is reported in the manuscript. The Richmond Agitation-Sedation Scale (RASS), the Visual Analogue Scale (VAS) and the Patient State Index were collected during sedation. Each patient was monitored using the Masimo Sedline. At the end of ablation, the Likert Scale Questionnaire (LSQ) was used to assess the patients' satisfaction with intraoperative analgesia-sedation.
No procedural complications were documented. Sufficient oxygen saturation was maintained in all patients during procedure. Non-invasive ventilation or tracheal intubation were not required for any patient. The RAAS score between -1 to -5 was obtained in 27 patients (93%) while the value 0 was obtained in 2 patients (7%). The VAS score between 0 to 2 was obtained in 24 patients (83%); the VAS score 3 in 3 patients (10%) and the VAS score 4 in 2 patients (7%). The PSI score <50 was achieved in 16 patients (55%) while the PSI between 50 and 70 was achieved in 9 patients (31%). Positive answers to LSQ were obtained in most patients.
During PFA ablation procedures with the variable-loop circular catheter and its accompanying biphasic pulse, our deep sedation protocol is a valid alternative to general anesthesia.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and catheter ablation in recommended in symptomatic patients.1 One of the procedure goals is to achieve optimal ablation accuracy with minimal pain or complications for patient, and therefore, the sedation technique is crucial. Currently, ablation procedures are conducted in three settings: general anaesthesia with endotracheal intubation (EI), deep sedation, or conscious sedation.2,3 However, there is no standardized clinical guidelines for sedation.
Pulsed field ablation (PFA) is a novel ablative modality that by virtue of its putative preferential action on myocardial tissue will reduce the risk of serious procedural complications.4–10
The majority of PFA procedures was performed using general anaesthesia with EI.4,8 In this article, we report the data concerning our deep sedation protocol used in patients enrolled in the inspIRE study.10
Methods
Study population
We enrolled 29 patients included in the inspiRE trial and subjected to pulmonary vein isolation for symptomatic paroxysmal AF.
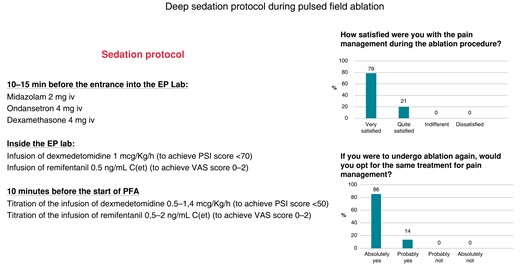
Arterial blood pressure, cardiac rhythm, and digital pulse oximetry were monitored continuously during the procedure. The deep sedation protocol started using midazolam 2 mg iv, ondansetron 4 mg iv, and dexamethasone 4 mg iv administered 10–15 min before the entrance into the electrophysiology (EP) lab. Afterwards, infusion of dexmedetomidine 1 µg/Kg/h [to achieve patient state index (PSI) score <70] and remifentanil 0.5 ng/mL C(et) [to achieve visual analogue scale (VAS) score 0–2] was started inside the EP lab. Finally, infusion of dexmedetomidine was titrated to achieve PSI score <50 (dose 0.5–1.4 µg/Kg/h), and infusion of remifentanil was titrated to achieve VAS score 0–2 [dose 0.5–2 ng/mL C(et)] 10 min before the start of PFA energy delivery. Propofol was not used due to the risk of respiratory depression.
Patients were monitored using the Masimo Sedline (Masimo Corporation, Irvine, CA), and the degree of sedation was evaluated using the Richmond agitation-sedation scale (RASS), the VAS, and PSI.11–14 At the end of ablation, the Likert scale questionnaire (LSQ) was used to assess the patients’ satisfaction.14 All the staff was trained in management of sedation, and an anaesthetic consultant was available.
Masimo Sedline
The Masimo Sedline is an electroencephalogram-based monitoring system which determines the depth of sedation or anaesthesia using the PSI, which is a clinically validated measure of the effect of sedation.12
Richmond agitation-sedation scale
The RASS is a 10-point scale, with four levels of anxiety or agitation [+1 to +4 (combative)], one level to denote a calm and alert state (0), and five levels of sedation (−1 to −5) culminating in unarousable. It uses the duration of eye contact following verbal stimulation as the principal means of titrating sedation.11
Visual analogue scale
The VAS consists of a 10 cm line with two end points of pain, usually ‘no pain’ and ‘unbearable pain’. The patient is asked to make a vertical mark through the line corresponding to the intensity of pain. The scale is scored by measuring the distance in mm from ‘no pain’ to the patient’s mark.13,14
Likert scale questionnaire
The LSQ consists of several declarative items that express a viewpoint on a topic. Respondents can indicate the degree to which they agree or disagree with the opinion expressed by the statement.14
Statistical analysis
Descriptive statistics are summarized as mean ± standard deviations for continuous variables and counts and percentages for categorical variables. All statistical analyses were carried-out with STATA statistical software version 14 (Stata, College Station, TX, USA).
Results
The clinical characteristics of patients are reported in Table 1. Mean procedural time was 68 ± 22 min. The deep sedation protocol was used in all patients without side effects. The high-flow nasal cannula oxygenation was used in all patients obtaining a sufficient oxygen saturation (>95%) during the procedure. In two patients, a Guedel airway tube was used, and EI was never required. No patient had a significant sedation-related hypotension. Naloxone was not used. No patient had muscular fasciculations or cough during PFA. Three patients underwent electrical cardioversion of AF at the end of the procedure, and the anaesthetic consultant used a low dose of propofol (0.4–0.5 mg/Kg).
| Male sex, n (%) | 21 (72) |
| Mean age (years) | 55 ± 9 |
| Left atrial antero-posterior diameter | 38 ± 4 |
| CHA2DS2-VASc, n (%) | |
| 0 | 11 (38) |
| 1 | 8 (27) |
| 2 | 5 (17) |
| 3 | 4 (14) |
| 4 | 1 (4) |
| Diabetes mellitus, n (%) | 1 (4) |
| Hypertension, n (%) | 16 (55) |
| Family history of coronary artery disease, n (%) | 7 (24) |
| Hypercholesterolaemia, n (%) | 8 (27) |
| Hypertriglyceridaemia, n (%) | 5 (17) |
| Active smoking, n (%) | 10 (34) |
| Body mass index (Kg/m2) | 26 ± 5 |
| Heart failure (EF < 35%), n (%) | 0 (0) |
| Coronary artery disease, n (%) | 2 (7) |
| Previous ischaemic stroke, n (%) | 0 (0) |
| Transient ischaemic attack, n (%) | 0 (0) |
| Chronic renal failure, n (%) | 2 (7) |
| Left ventricular ejection fraction, mean ± SD | 60 ± 5 |
| Medical therapy, n (%) | |
| Beta blockers, n (%) | 14 (48) |
| Flecainide, n (%) | 20 (69) |
| Propafenon, n (%) | 2 (7) |
| Amiodaron, n (%) | 5 (17) |
| Sotalol, n (%) | 2 (7) |
| Direct oral anticoagulant, n (%) | 29 (100) |
| Male sex, n (%) | 21 (72) |
| Mean age (years) | 55 ± 9 |
| Left atrial antero-posterior diameter | 38 ± 4 |
| CHA2DS2-VASc, n (%) | |
| 0 | 11 (38) |
| 1 | 8 (27) |
| 2 | 5 (17) |
| 3 | 4 (14) |
| 4 | 1 (4) |
| Diabetes mellitus, n (%) | 1 (4) |
| Hypertension, n (%) | 16 (55) |
| Family history of coronary artery disease, n (%) | 7 (24) |
| Hypercholesterolaemia, n (%) | 8 (27) |
| Hypertriglyceridaemia, n (%) | 5 (17) |
| Active smoking, n (%) | 10 (34) |
| Body mass index (Kg/m2) | 26 ± 5 |
| Heart failure (EF < 35%), n (%) | 0 (0) |
| Coronary artery disease, n (%) | 2 (7) |
| Previous ischaemic stroke, n (%) | 0 (0) |
| Transient ischaemic attack, n (%) | 0 (0) |
| Chronic renal failure, n (%) | 2 (7) |
| Left ventricular ejection fraction, mean ± SD | 60 ± 5 |
| Medical therapy, n (%) | |
| Beta blockers, n (%) | 14 (48) |
| Flecainide, n (%) | 20 (69) |
| Propafenon, n (%) | 2 (7) |
| Amiodaron, n (%) | 5 (17) |
| Sotalol, n (%) | 2 (7) |
| Direct oral anticoagulant, n (%) | 29 (100) |
EF, ejection fraction.
| Male sex, n (%) | 21 (72) |
| Mean age (years) | 55 ± 9 |
| Left atrial antero-posterior diameter | 38 ± 4 |
| CHA2DS2-VASc, n (%) | |
| 0 | 11 (38) |
| 1 | 8 (27) |
| 2 | 5 (17) |
| 3 | 4 (14) |
| 4 | 1 (4) |
| Diabetes mellitus, n (%) | 1 (4) |
| Hypertension, n (%) | 16 (55) |
| Family history of coronary artery disease, n (%) | 7 (24) |
| Hypercholesterolaemia, n (%) | 8 (27) |
| Hypertriglyceridaemia, n (%) | 5 (17) |
| Active smoking, n (%) | 10 (34) |
| Body mass index (Kg/m2) | 26 ± 5 |
| Heart failure (EF < 35%), n (%) | 0 (0) |
| Coronary artery disease, n (%) | 2 (7) |
| Previous ischaemic stroke, n (%) | 0 (0) |
| Transient ischaemic attack, n (%) | 0 (0) |
| Chronic renal failure, n (%) | 2 (7) |
| Left ventricular ejection fraction, mean ± SD | 60 ± 5 |
| Medical therapy, n (%) | |
| Beta blockers, n (%) | 14 (48) |
| Flecainide, n (%) | 20 (69) |
| Propafenon, n (%) | 2 (7) |
| Amiodaron, n (%) | 5 (17) |
| Sotalol, n (%) | 2 (7) |
| Direct oral anticoagulant, n (%) | 29 (100) |
| Male sex, n (%) | 21 (72) |
| Mean age (years) | 55 ± 9 |
| Left atrial antero-posterior diameter | 38 ± 4 |
| CHA2DS2-VASc, n (%) | |
| 0 | 11 (38) |
| 1 | 8 (27) |
| 2 | 5 (17) |
| 3 | 4 (14) |
| 4 | 1 (4) |
| Diabetes mellitus, n (%) | 1 (4) |
| Hypertension, n (%) | 16 (55) |
| Family history of coronary artery disease, n (%) | 7 (24) |
| Hypercholesterolaemia, n (%) | 8 (27) |
| Hypertriglyceridaemia, n (%) | 5 (17) |
| Active smoking, n (%) | 10 (34) |
| Body mass index (Kg/m2) | 26 ± 5 |
| Heart failure (EF < 35%), n (%) | 0 (0) |
| Coronary artery disease, n (%) | 2 (7) |
| Previous ischaemic stroke, n (%) | 0 (0) |
| Transient ischaemic attack, n (%) | 0 (0) |
| Chronic renal failure, n (%) | 2 (7) |
| Left ventricular ejection fraction, mean ± SD | 60 ± 5 |
| Medical therapy, n (%) | |
| Beta blockers, n (%) | 14 (48) |
| Flecainide, n (%) | 20 (69) |
| Propafenon, n (%) | 2 (7) |
| Amiodaron, n (%) | 5 (17) |
| Sotalol, n (%) | 2 (7) |
| Direct oral anticoagulant, n (%) | 29 (100) |
EF, ejection fraction.
Ten minutes before the start of PFA, the median dose of dexmedetomidine was 0.9 µg/Kg/h (range 0.5–1.4), while the median dose of remifentanil was 1.2 ng/mL C(et) (range 0.5–2).
The results regarding the RASS, VAS, and PSI scores are reported in Figure 1. Positive answers to LSQ were obtained in most patients (Figure 1). Two patients had a procedure-related complication (pseudoaneurysm of right femoral artery resolved using manual compression). No patient had phrenic nerve damage.
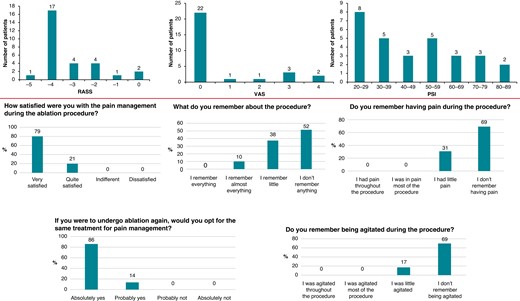
The results regarding the Richmond agitation-sedation scale (RASS), visual analogue scale (VAS), and patient state index (PSI) before starting pulsed field ablation (upper part). Answers given by patients on the Likert scale questionnaire (lower part).
Discussion
Our deep sedation protocol was safe without any side effects. It allowed us to achieve good sedation parameters as demonstrated by the positive feedback reported by patients. In order to use this sedation protocol, it is essential that the EP staff is trained for cardiac sedation and advanced cardiac life support.
There is currently no standardized strategy for sedation protocols. Previous studies reported that compared to conscious sedation with fentanyl/midazolam, deep sedation with propofol might lead to higher ablation accuracy and is more comfortable for the patients.2,3
These concepts need to be re-evaluated using PFA. In addition to the pain, PFA may cause contraction of the diaphragm or transient cough, and for these reasons, most procedures were performed using general anaesthesia.4,8,10 The recent inspIRE trial,10 in fact, reported the use of general anaesthesia in 73% of patients.
In our study, the sedation protocol proved to be effective in pain management. The protocol was able to achieve adequate sedation scores, and it may be consider a valid alternative to general anaesthesia.
In our population, we did not observe muscle contractions or transient cough during PFA probably because this catheter delivers only bipolar energy with a short electrodes distance. Furthermore, PFA use trains of high-voltage very short duration pulses greatly shortening the stability time necessary to obtain an effective lesion in a given point.15 For all these reasons, the benefit of general anaesthesia (catheter stability) may be no longer needed, and an optimal sedation protocol could reduce the risks of complications mainly due to EI.
Finally, the anaesthetic consultant is not always present in many EP labs, and our protocol, if used by expert operators, could be a valid strategy for pain management.
The study limitations are as follows: low number of patients, no randomization to another form of sedation or general anaesthesia, data only related to paroxysmal AF, and finally, sedation protocol used for only one PFA system.
Funding
None declared.
Data availability
Data are available on request.
References
Author notes
Conflict of interest: M.G. holds an agreement with Biosense Webster on new technologies development. The other authors have no conflicts of interest to declare.



