-
PDF
- Split View
-
Views
-
Cite
Cite
Robert H Anderson, Damian Sanchez-Quintana, Shumpei Mori, Diane E Spicer, Hein J J Wellens, Yash Lokhwandala, Jose-Angel Cabrera, Jeronimo Farre, Eduardo Back Sternick, Miniseries 2—Septal and paraseptal accessory pathways—Part I: The anatomic basis for the understanding of para-Hisian accessory atrioventricular pathways, EP Europace, Volume 24, Issue 4, April 2022, Pages 639–649, https://doi.org/10.1093/europace/euab292
Close - Share Icon Share
Abstract
Although the anatomy of the atrioventricular conduction axis was well described over a century ago, the precise arrangement in the regions surrounding its transition from the atrioventricular node to the so-called bundle of His remain uncertain. We aimed to clarify these relationships.
We have used our various datasets to examine the development and anatomical arrangement of the atrioventricular conduction axis, paying particular attention to the regions surrounding the point of penetration of the bundle of His. It is the areas directly adjacent to the transition of the atrioventricular conduction axis from the atrioventricular node to the non-branching atrioventricular bundle that constitute the para-Hisian areas. The atrioventricular conduction axis itself traverses the membranous part of the ventricular septum as it extends from the node to become the bundle, but the para-Hisian areas themselves are paraseptal. This is because they incorporate the fibrofatty tissues of the inferior pyramidal space and the superior atrioventricular groove. In this initial overarching review, we summarize the developmental and anatomical features of these areas along with the location and landmarks of the atrioventricular conduction axis. We emphasize the relationships between the inferior pyramidal space and the infero-septal recess of the subaortic outflow tract. The details are then explored in greater detail in the additional reviews provided within our miniseries.
Our anatomical findings, described here, provide the basis for our concomitant clinical review of the so-called para-Hisian arrhythmias. The findings also provide the basis for understanding the other variants of ventricular pre-excitation.
Although the atrioventricular conduction axis penetrates through the membranous part of the ventricular septum at the site of the component known as the bundle of His, the areas directly adjacent to the site of penetration are paraseptal.
It is pathways found within these paraseptal areas that provide the anatomical substrates for the so-called para-Hisian arrythmias.
In this original overarching review, we summarise the developmental and anatomical features of these para-Hisian areas, developing the concepts in greater detail in additional reviews within our miniseries.
Introduction
It is now over a century since Tawara clarified the location of the solitary pathway responsible for atrioventricular conduction in the normal heart.1 Interest in the precise location of this atrioventricular conduction axis has now been rekindled with the upsurge of use of transcatheter therapies to replace the aortic valve,2 and with the approach to direct pacing of the His bundle.3 Further interest is currently emerging in the clarification of the morphological substrates for so-called ‘Mahaim’ pre-excitation.4 The initial investigations made by Mahaim and his associates5,6 suggested that these arrhythmias would be the consequence of abnormal connections between the atrioventricular conduction axis and the crest of the muscular ventricular septum. It is now recognized that the abnormal rhythms are more usually the consequence of re-entry using an accessory pathway also described as being ‘atriofascicular’.7 When assessing the potential substrates for pre-excitation, however, the group of morphologists commissioned by the European Society of Cardiology had used the term ‘atriofascicular’ to account for direct connections between the atrial myocardium and the penetrating atrioventricular bundle,8 pathways also described as being ‘atrioHisian’. Convincing anatomic evidence for these alleged morphological substrates is hard to find.9 Pathways producing pre-excitation, nonetheless, are certainly found in the areas directly adjacent to the location of the bundle of His. These areas are located both superiorly and inferiorly relative to the bundle, which itself penetrates through the atrioventricular component of the membranous septum. It is some time now since another group of experts proposed that these areas adjacent to the bundle of His should be described using the attitudinally appropriate terms, and that the areas should correctly be described as being paraseptal rather than septal.10 The pathways found in these areas traverse the fibroadipose tissues of the atrioventricular grooves, and hence are extracavitary rather than septal entities. This constraint, however, is equally valid for a large part of the area that the aforementioned experts still considered to be ‘septal’, namely the atrial floor of the triangle of Koch. Despite the passage of time, the pathways traversing these areas are still often described by electrophysiologists using inaccurate non-attitudinal terms. The inaccuracy of such usage is now becoming increasingly obvious due to the more frequent access in the clinical setting of techniques that show the heart as it lies within the chest.11,12 With all these issues in mind, we have now reviewed the morphology of these para-Hisian areas. We have based our descriptions on our current understanding of cardiac development, using illustrations provided by our ongoing analysis of gross specimens, histological preparations, and virtual dissections of computerized tomographic datasets. In concomitant reviews, we discuss the electrophysiological correlations of the anatomical findings.13
Developmental considerations
It is now well established that the atrioventricular conduction axis itself is formed from a ring of cardiomyocytes, known as the primary ring. This ring encircles the initial embryonic interventricular communication.14 With ongoing development, there is extensive remodelling of the initial interventricular connection, and by extension remodelling of the primary ring. The remodelling permits the atrioventricular canal to expand so as to provide the right ventricle with its direct input via the tricuspid valve, while a subsequent phase of remodelling places the subaortic component of the outflow tract in direct continuity with the cavity of the left ventricle.15 These processes, however, can also occur without producing the normal arrangement of the atrioventricular conduction axis. This is shown by analysis of hearts from individuals with atrioventricular septal defect in the setting of a common atrioventricular junction.16 In this congenital lesion, the right atrium communicates with the right ventricle, albeit through a common atrioventricular junction, while the aortic root, although ‘unwedged’, arises from the left ventricle. A consequence of the differences with the normal heart is that the atrioventricular node is located inferiorly, at the so-called cardiac crux, while the ventricular bundle branches have no relationship to the unwedged aortic root. The key feature during development that ensures presence of a normal conduction axis is the growth into the heart of a structure first identified in the middle part of the nineteenth century,17 and now called the vestibular spine.18 It is this entity that binds together the atrioventricular cushions, permitting expansion of the right and left atrioventricular orifices, along with the subsequent transfer of the aortic root so that it interposes between the muscular ventricular septum and the orifice of the mitral valve. These changes, which produce the inferior pyramidal space,19,20 and the infero-septal recess of the left ventricle,21 occur after the completion of ventricular septation by formation of the membranous septum from the atrioventricular cushions.22 Muscularization of the vestibular spine, furthermore, produces the direct connections between the atrial septum and the atrial component of the initial interventricular ring that are necessary to form the atrioventricular node.23 Unlike the situation in atrioventricular septal defect with common atrioventricular junction,16 and because of the expansion of the right ventricular inlet to form the inferior pyramidal space, the newly formed node, when viewed from the right side, is positioned at the centrepoint of the cardiac mass (Figure 1A). Being formed at the apex of the inferior pyramidal space, nonetheless, it remains directly related to the extracavitary tissues. By virtue of formation of the infero-septal recess, furthermore, the node formed at the apex of the inferior pyramidal space is directly adjacent to the crest of the muscular ventricular septum (Figure 1B). The bundle of His, therefore, needs to do no more than penetrate the membranous part of the septum to reach the crest of the muscular septum.
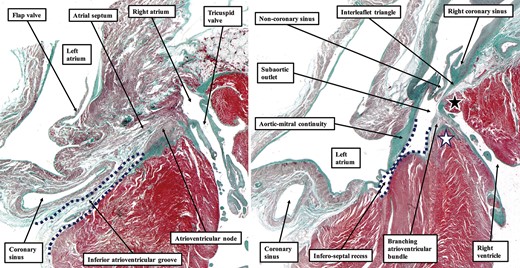
The images are serial sections taken from right to left through the septal component of a human foetal heart at 30 weeks’ gestation. In (A), the dotted lines show the inferior atrioventricular groove, which separates the basal surface of the atrial septum from the inferior component of the muscular ventricular septum. The groove, filled with fibroadipose tissue, extends superiorly to reach the inferior border of the atrioventricular node. In (B), the dotted lines show how the infero-septal recess of the subaortic outflow tract interposes between the leaflets of the mitral valve and the left ventricular aspect of the muscular ventricular septum. The branching part of the conduction axis is carried on the crest of the muscular septum (white star). The wall of the right ventricle directly cranial to the membranous part of the septum (black star) separates the ventricular cavity from the right atrioventricular groove. Note, in both panels, the location of the coronary sinus within the inferior atrioventricular groove. The sinus has its own myocardial walls, but strands of myocardium join the walls of the coronary sinus and the wall of the left atrium.
Gross anatomy of the para-Hisian and paraseptal areas
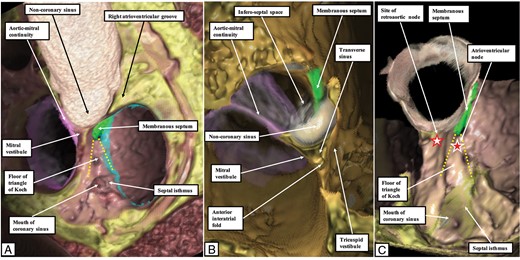
In the postnatal heart, it is the fibrous septal area, in other words the membranous septum, which is penetrated by the conduction axis, with this penetrating component usually described as the bundle of His. It is the areas directly adjacent to the location of the penetrating bundle, therefore, which constitute the para-Hisian regions, when using the prefix ‘para’ to indicate that the areas are ‘next to’ the location of the bundle. Previous understanding of the anatomy of these areas has been confused by two inaccurate suppositions. In the first place, the triangle of Koch, the recognized landmark to the site of the atrioventricular node, has usually been drawn with its apex pointing to the right. This was a consequence of the bad habit, still popular, of describing the heart as if removed from the thorax and positioned on its apex, an arrangement we have described as the Valentine heart.11 Assessment using the attitudinally appropriate position shows that the apex of the triangle points superiorly (Figure 2).
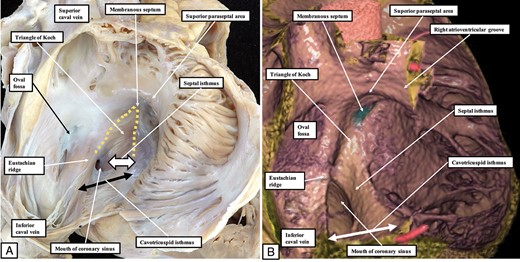
(A) The heart positioned in attitudinally appropriate position, with the right atrium opened by making a cut through the wall of the appendage, which has been reflected to show the septal surface and the annulus of the tricuspid valve. When the heart is positioned as it lies within the body, the apex of the triangle of Koch points superiorly. (B) A virtual dissection of a living dataset prepared by computed tomography. The superior paraseptal area is the atrial component of the supraventricular crest of the right ventricle. Note that the inferior paraseptal area, formed by the floor of the triangle of Koch, continues inferiorly as the septal isthmus, which is the part between the mouth of the coronary sinus and the hinge of the septal leaflet of the tricuspid valve. This area, in turn, is contiguous with the cavotricuspid isthmus, which then continues parietally as the inferior part of the right atrioventricular junction.
The second confusing factor was that, as we have already emphasized, the areas inferior and superior to the fibrous membranous septum used to be described as being septal. The atrial and ventricular walls in these areas, however, are separated by the extracavitary tissues of the atrioventricular grooves. Hence, they are paraseptal rather than septal. Within the area that is inferiorly positioned, and directly adjacent to the membranous septum, it is a superior extension of the fibroadipose tissues of the atrioventricular grooves that separates the atrial wall of the triangle of Koch from the underlying ventricular myocardium (Figure 3). The fibroadipose tissue fills the cavity of the inferior pyramidal space.19,20 The overall area inferior to the membranous septum, therefore, is paraseptal, and is now designated as being midparaseptal.20 It is particularly vulnerable during interventional electrophysiological manoeuvres. This is because the atrioventricular node is found within its atrial wall, usually at its upper third.24 Since the atrioventricular node becomes the bundle of His once it has penetrated through the fibrous septum, it follows that the area containing the atrioventricular node must not only be paraseptal but also para-Hisian. When considering the threat of inducing atrioventricular block by catheter interventions, it is the inferior third of the mid-paraseptal region that is the safest area. Interventions on the middle third carry a certain risk, since these parts contain the rightward and leftward inferior extensions from the compact node.9 The rightward extension, itself variable in size, runs parallel to the hinge of the septal leaflet of the tricuspid valve. When extensive, it continues within the vestibular myocardium of the septal isthmus. Lying between the mouth of the coronary sinus and the hinge of the septal leaflet of the tricuspid valve, this isthmus is part of the inferior third of the mid-paraseptal area. The leftward inferior extension of the node is similarly variable in size, and can be absent. If present, it extends beneath the mouth of the coronary sinus. The mid-paraseptal area itself, when traced still further inferiorly, merges with the area that is truly inferior and paraseptal.4 There is no obvious boundary between the mid and inferior paraseptal areas, but a useful landmark to differentiate the two is the level of the roof of the mouth of the coronary sinus.
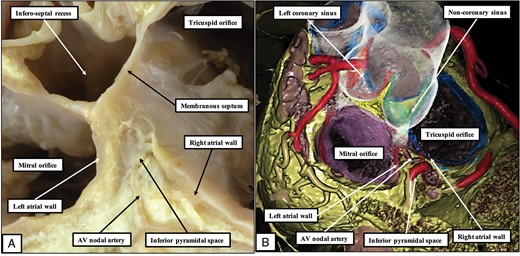
(A) A dissection made by removing the floor of the triangle of Koch, along with the non-coronary leaflet of the aortic valve. The apex of the inferior pyramidal space, which is filled with extracavitary fibro-adipose tissue, is adjacent superiorly to the inferior extent of the infero-septal recess of the left ventricle, with the fibrous base of the atrioventricular component of the membranous septum interposed between the two areas. (B) How the relationships are confirmed by virtual dissection of a computerised tomographic dataset. Note the course of the artery to the atrioventricular node through the inferior pyramidal space.
The inferior paraseptal area itself then diverges to form leftward, central, and rightward components. The leftward part, which contains the walls of the terminal part of the coronary sinus, is directly adjacent to the inferior wall of the left atrium (Figure 1). The central component includes the inferior, or middle, cardiac vein. This area constitutes the so-called crux of the heart. The right part, when viewed from the right atrial aspect, merges superiorly with the septal isthmus, and includes the paraseptal component of the cavotricuspid, or inferior, isthmus. Of these extensive paraseptal areas inferior to the membranous septum, it is only the superior component of the mid-paraseptal area, containing the atrioventricular node, which is directly para-Hisian.
The superior para-Hisian area is directly superior to the membranous septum (Figures 2 and 4). As viewed from within the right atrium, it is formed by the vestibule of the tricuspid valve, which supports the hinge of the antero-superior leaflet of the tricuspid valve (Figure 2). The atrial vestibule is then separated by the superior atrioventricular groove from the myocardial supraventricular crest of the right ventricle (Figure 4). Hence, accessory myocardial pathways traversing the insulating tissues of the atrioventricular groove within this superior paraseptal area are appropriately described as being crestal. The area is related directly to the right coronary aortic valvar sinus (Figure 4). When traced leftward, the atrial component of this central superior para-Hisian area continues as the anterior interatrial wall, with its extension becoming the superior vestibule of the mitral valve. These areas are directly related to the non-coronary sinus of the aortic root (Figure 5). The anterior interatrial wall itself is also of importance, since it is in this area of myocardium that we find the so-called retroaortic node.25 If we are then properly to relate these para-Hisian regions to the atrioventricular conduction axis, it is necessary again to consider the influence of the infero-septal recess of the left ventricle (Figure 6). This area is the space between the aortic leaflet of the mitral valve and the endocardial surface of the ventricular septum. Its rightward border is the atrioventricular component of the membranous septum. This continues as the fibrous tissues that form its roof, with these merging with the area known as the right fibrous trigone. This latter structure is the thickening of the rightward end of the area of fibrous continuity between the leaflets of the aortic and mitral valves. Together, these fibrous entities make up the central fibrous body. The leftward border of the recess is the aortic leaflet of the mitral valve itself. It is the adjacency of the inferior extent of the recess to the apex of the inferior pyramidal space that explains the very short length of the bundle of His in the human heart.
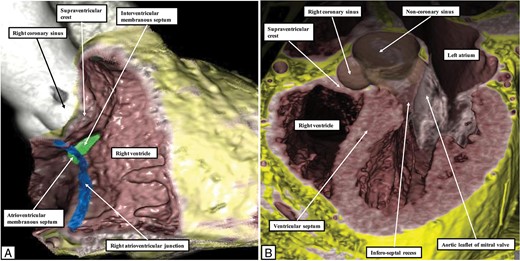
Virtual dissections of computed tomographic datasets show how the so-called ‘anterior septal area’, in reality the junction between the vestibule of the tricuspid valve and the supraventricular crest, is superior and paraseptal. It is directly adjacent to the right coronary sinus of the aortic root. (A) A cut across the inlet of the right ventricle, while (B) shows a frontal cut, emphasising that the supraventricular crest is directly related to the aortic root and hence is paraseptal rather than septal.
The images are virtual dissections of a computed tomographic dataset obtained from an individual undergoing assessment for suspected coronary arterial disease. They show the relationships of the sinuses of the aortic root to the adjacent structures. Panel A shows the view of the base of the ventricular mass as seen from above, and slightly from the right. In panel B, the larger part of the non-coronary sinus has been cut away to show the entrance to the infero-septal recess, which undermines the base of the atrial septum. Panel C then shows an oblique cut revealing the relationship of the triangle of Koch, containing the regular atrioventricular node towards its apex, to the site of the retro-aortic node, found in the base of the atrial septum.
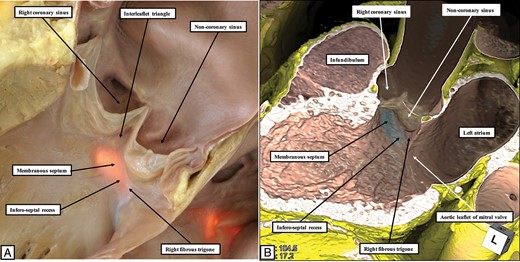
The images show the boundaries of the infero-septal recess of the left ventricle. (A) is a short-axis section of the base of the ventricular cone viewed from the apex. This shows how the attachment of the septal leaflet of the tricuspid valve separates the septum into its atrioventricular and interventricular components. (B) This in the virtual dissection, wherein the location of the membranous septum has been emphasized.
The location and relationships of the atrioventricular conduction axis
On the basis of knowledge of the relationships between the inferior pyramidal space and the infero-septal recess of the left ventricle, it now becomes an easy matter to understand the precise sites of the components of the atrioventricular conduction axis relative to the para-Hisian regions. These are well illustrated by reference to a series of sections taken from a human foetus obtained at 25 weeks of gestation. By this stage of development, the septal structures have been formed, and the septal leaflet of the tricuspid valve has delaminated from the surface of the ventricular septum. At the inferior component of the right ventricular inlet, in the region of the floor of the triangle of Koch, the fibroadipose tissues of the inferior pyramidal space are seen separating the atrial wall from the underlying ventricular myocardium (Figure 7A). Within this inferior paraseptal area, the inferior extension of the atrioventricular node extends within the vestibule of the tricuspid valve. The compact atrioventricular node itself (Figure 7B) is supported on the thickened fibrous tissue formed at the apex of the inferior pyramidal space, which is itself continuous with the base of the fibrous membranous septum. Figure 7C shows the transition to the penetrating component of the axis. The insulation of the bundle of His is seen as the conduction axis itself passes between the fibrous tissues of the central fibrous body and those formed within the inferior atrioventricular groove. We now know that there is variation in location of the compact atrioventricular node relative to the paraseptal and septal areas.10 In some individuals, the node is found within the atrial floor of the triangle, supported by fibrous thickening of the tissues of the inferior pyramidal space (Figure 8A,B). In this situation, therefore, the node itself is a component of the mid-paraseptal part of the atrioventricular junctions. In other individuals, the compact node is located within the septal area of the atrioventricular junctions, being supported on the atrioventricular component of the membranous septum (Figure 8C,D). Irrespective of the precise location of the node within the atrioventricular junctional area, the transition to become the bundle of His is found when the axis passes between the fibrous tissues of the inferior atrioventricular groove and those of the central fibrous body. The area of penetration is directly beneath the junction of the anterior walls of the right and left atrial chambers. In hearts from experimental animals, immuno-histochemical investigations show that a second nodal structure is to be found in this area.25 This structure, which is the retroaortic node, can also be recognized as being histologically distinct in the prenatal human heart (Figure 7C). It is located in superior para-Hisian position, and is directly related anteriorly to the non-coronary aortic sinus (Figure 7D).26 The atrioventricular conduction axis itself, at this level, is sandwiched between the fibrous membranous septum and the crest of the muscular ventricular septum. Fibrous tissue in this area also separates the cavity of the left ventricle from the transverse sinus of the pericardial space. Hence, the overall region is again paraseptal rather than septal (Figure 7E). Sections taken more cranially, cutting through the right coronary aortic sinus, show the relationship between the hinge of the right coronary leaflet of the aortic valve and the basal extent of the left bundle branch (Figure 7F). This distance, which is itself variable, is one of the keys to the safety of transcatheter insertion of prosthetic aortic valves.2 The histological sections confirm that it is only the area formed by the fibrous membranous septum that is truly an atrioventricular septal structure, although on occasion it is covered on its right side by a layer of atrial myocardium. The area directly cranial to the membranous septum is again both paraseptal and para-Hisian (Figure 6). It is directly related to both the right and non-coronary sinuses of the aortic root and also to the supraventricular crest of the right ventricle (Figure 9). Accessory pathways passing though this area can be considered to be crestal when their ventricular insertion is at the paraseptal area of the supraventricular crest.
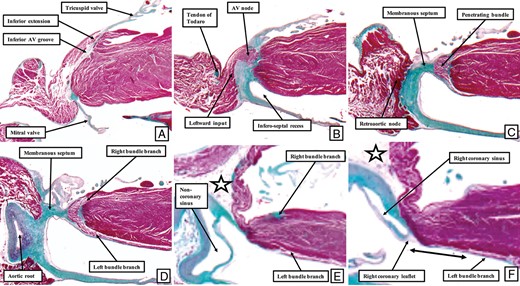
The images show a series of sections taken across the paraHisian regions from a dataset prepared from a human foetus obtained at 25 weeks of gestation. (A) The most inferior section, which is through the inferior paraseptal region. The fibroadipose of the inferior pyramidal space separates the atrial and ventricular walls. Cranial to this section, at the apex of the triangle of Koch, as seen in (B), is found the compact atrioventricular (AV) node. The inferior extent of the infero-septal recess of the left ventricle is already obvious. (C) How the axis penetrates through the membranous part of the septum to reach the crest of the muscular ventricular septum. The axis then divides into its right and left branches directly beneath the aortic root, as shown in (D). The sections taken still more cranially, as seen in (E,F), show how the area is paraseptal, with the white star with black borders showing the right atrioventricular groove. As indicated by the double headed arrow in (F), the attachment of the right coronary aortic leaflet is some distance away from the superior fascicle of the left bundle branch. The star shows the transverse sinus of the pericardium, marking the location of the inner heart curvature.

The images show the different arrangements of the compact atrioventricular node. In (A,B), the node lies at the apex of the inferior pyramidal space, supported by a thickening of the fibroadipose tissue occupying the space. The location of the section shown in the (B) is indicated by the line B–B in (A). The images in (C–E) show the transition from the atrioventricular node to the penetrating atrioventricular bundle, usually known as the bundle of His. In this individual, unlike the arrangement shown in (A,B), the compact node is located within the septal area of the atrioventricular junctions. (C) The right-sided septal surface of the heart from which the serial sections shown in (D and E) were taken, the levels being shown by the lines in (C). (D) The location of the bundle of His, while (E) shows the compact atrioventricular node.
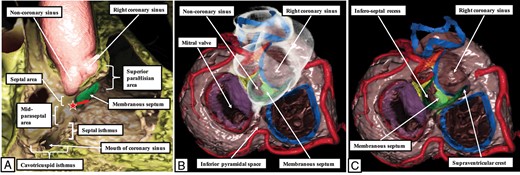
The virtual dissections show the anatomical relationships of the para-Hisian regions, which are made up of the septal component of the atrioventricular junctions together with the superior para-Hisian area and the upper third of the mid-paraseptal area. (A) A view from the right side having cut away the parietal walls of the right atrial and ventricular chambers. (B,C) Views of the atrioventricular junctions from the atrial aspect, with the right hand panel cut deeper to show the infero-septal recess of the left ventricle interposed between the aortic leaflet of the mitral valve and the muscular ventricular septum.
The location of substrates for para-Hisian arrhythmias
The anatomy of the para-Hisian regions, coupled with appreciation of the precise location of the atrioventricular conduction axis, now permits accurate inferences to be made regarding the potential anatomical substrates for the abnormal rhythms known to originate in the vicinity of the membranous septum. It used to be stated that the typical accessory muscular atrioventricular connections, producing Wolf–Parkinson–White pre-excitation, were found in the anterior and posterior ‘septal’ areas. As we have shown, because these areas incorporate the fibroadipose tissues of the atrioventricular junctions between their atrial and ventricular walls, they are more accurately described as being paraseptal (Figure 9). Abnormal accessory muscular connections can cross through the fibroadipose tissues in either area. It is also possible that such muscular accessory atrioventricular connections can cross the area of the membranous septum itself, and hence be truly septal. We have encountered two such examples in the same heart of an infant dying with a dysplastic tricuspid valve with dual orifices (Figure 10). It is appropriate, therefore, to distinguish between paraseptal and septal accessory muscular connections as potential substrates for regular Wolff–Parkinson–White syndrome. The septal connections, of necessity, will be restricted to, and cross, the area of the membranous septum. They are truly para-Hisian.
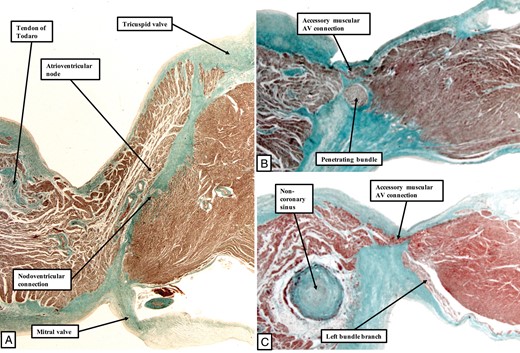
The images show the atrioventricular conduction axis in the heart from an infant dying with tricuspid valvar dysplasia. (A) The atrioventricular (AV) node, with a small nodoventricular connection. (B, C) Two muscular atrioventricular connections that crossed over the area of the membranous septum.
The question then remains as to the existence of direct atrio-Hisian connections. Such connections were postulated to provide the substrate for so-called Lown–Ganong–Levine syndrome. On this basis, the European Study Group suggested that the connections, if they existed, could be considered to be atriofascicular.8 The atriofascicular designation, however, is now usually given to the accessory connections originating from accessory atrioventricular nodes.4 The existence of accessory connections between the atrial myocardium and the penetrating component of the atrioventricular conduction axis, furthermore, remains a matter of debate. Much depends on the criterion chosen to distinguish the atrioventricular node from the bundle of His. In this regard, the definition provided initially by Tawara retains its currency. He explained how the site of insulation of the conduction axis provided the necessary landmark.1 And, once the axis has become insulated from the atrial myocardium by the fibrous tissues of the atrioventricular groove, the insulation provided is robust. We have yet to encounter a heart in which a connection exists between the atrial myocardium and the axis that itself penetrates a pre-existing fibrous sheath. We are also unaware of any previous example proven by serial histological sectioning. The so-called ‘atrio-Hisian’ tracts are no more than the ‘final’ connections between the atrial myocardium and the conduction axis prior to its insulation as the bundle of His.9 This is not to deny the existence of abnormal rhythms that have previously been explained on the basis of such pathways. We will discuss these problems further in our subsequent reviews, along with the electrophysiological characteristics of the paraseptal connections which are also para-Hisian.
Funding
Plan Estatal de Investigación Científica y Técnica y de Innovación 2013–2016 from the Ministerio de Economía, Industria y Competitividad of Spain and Fondo Europeo de Desarrollo Regional (FEDER) DPI2016-75799-R (AEI/FEDER, UE).
Conflict of interest: none declared.
References
His W (ed). Anatomie Menschlicher Embryonen, vol. 3. Position and form of the heart and great vessels. Leipzig: Zur Geschichte der Organe, Vogel; 1885. p
Author notes
Hein J.J. Wellens sadly died on 9 June 2020.



