-
PDF
- Split View
-
Views
-
Cite
Cite
GF Romiti, D Pastori, JM Rivera-Caravaca, WY Ding, YX Gue, D Menichelli, J Gumprecht, M Koziel, PS Yang, Y Guo, GYH Lip, M Proietti, The Atrial Fibrillation Better Care (ABC) pathway in atrial fibrillation: a systematic review and meta-analysis of 285,000 patients, EP Europace, Volume 23, Issue Supplement_3, May 2021, euab116.290, https://doi.org/10.1093/europace/euab116.290
Close - Share Icon Share
Abstract
Type of funding sources: None.
The ‘Atrial Fibrillation Better Care’ (ABC) pathway has been recently proposed as a holistic approach for the comprehensive management of patients with Atrial Fibrillation (AF), standing on three main pillars: ‘A’ Avoid stroke (with Anticoagulants); ‘B’ Better symptom management; ‘C’ Cardiovascular and Comorbidity management. The ABC pathway is now recommended in several clinical guidelines, including the recent European Society of Cardiology (ESC) AF management guidelines. We performed a systematic review of the current evidence for use of the ABC pathway on clinical outcomes.
We performed a systematic review and meta-analysis according to PRISMA Guidelines. Pubmed and EMBASE were searched for studies reporting the prevalence of ABC pathway adherent management in AF patients, and its impact on clinical outcomes (all-cause death, cardiovascular death, stroke, and major bleeding). Metanalysis of odds ratio (OR) was performed with random-effect models; subgroup analysis and meta-regression were performed to account for heterogeneity; a CHA2DS2-VASc-stratified sensitivity analysis was also performed.
Among 2862 records retrieved from the literature search, 8 studies were included. The pooled prevalence of ABC adherent management was 21% (95% confidence intervals (CI), 13-34%), with a high grade of heterogeneity; in a multivariable meta-regression model, adherence to each criteria of the ABC pathway explained most part of the heterogeneity (R2 = 98.9%). Patients treated according to the ABC pathway showed a lower risk of all-cause death (OR:0.42, 95%CI 0.31-0.56), cardiovascular death (OR:0.37, 95%CI 0.23-0.58), stroke (OR:0.55, 95%CI 0.37-0.82) and major bleeding (OR:0.69, 95%CI 0.51-0.94), with moderate heterogeneity. Meta-regressions showed that the increasing prevalence of diabetes mellitus, coronary artery disease, chronic heart failure and history of stroke were associated with a reduced effectiveness of the ABC pathway for all-cause and cardiovascular death; each comorbidity was able to explain a significant proportion of heterogeneity at univariate meta-regression. Conversely, longer follow-up time was associated with more effectiveness of the ABC pathway for all outcomes. Adherence to ABC pathway was associated with a progressively greater reduction of the all-cause death risk amongst patients with higher CHA2DS2-VASc scores; no difference in ABC pathway effectiveness was found across CHA2DS2-VASc strata for CV death and stroke occurrence.
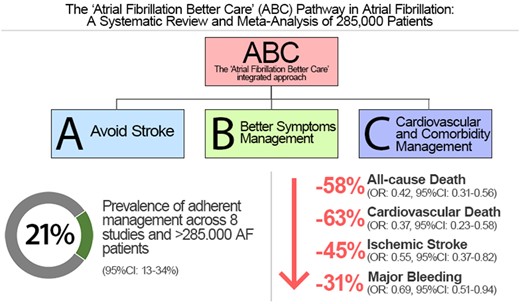
Abstract Figure.
- anticoagulants
- atrial fibrillation
- chronic heart failure
- coronary arteriosclerosis
- diabetes mellitus
- hemorrhage
- cerebrovascular accident
- ischemic stroke
- heterogeneity
- cardiovascular system
- comorbidity
- follow-up
- guidelines
- palliative care
- treatment outcome
- clinical practice guideline
- risk reduction
- cardiovascular death
- sensitivity analysis
- european society of cardiology
- cha2ds2-vasc score
- embase
- holistic approach



