-
PDF
- Split View
-
Views
-
Cite
Cite
P Brady, B Chandrasekaran, P Foley, 140
Can deviation from NICE guideline TA314 ever be justified?, EP Europace, Volume 20, Issue suppl_4, October 2018, Pages iv59–iv60, https://doi.org/10.1093/europace/euy204.030Close - Share Icon Share
Introduction: Ventricular tachycardia (VT) is a significant cause of morbidity and mortality in patients with structural heart disease.Implantable Cardioverter Defibrillators (ICDs) carry a class I indication for implantation to prevent sudden cardiac death (SCD) in patients with symptomatic Heart Failure who have a Left Ventricular Ejection Fraction (LVEF) less than 35% despite optimal medical therapy. Cardiac Resynchronisation Therapy (CRT) has an established role in the treatment of patients with severe left ventricular systolic dysfunction (LVED) and symptomatic heart failure despite optimal medical therapy (OMT).
Method: Data was collected retrospectively at Great Western Hospital from the local cardiology reporting database i.e. CVIS®, by searching for all complex pacing devices implanted form July 2011 until December 2017. All complex devices implanted during this time were identified and a total of 533 patients were included in this study. Search criteria was modified to exclude patients who had a device implanted for secondary prevention. Each case was assessed using the criteria included in NICE guideline TA314. This included NHYA functional status, QRS duration and degree of left ventricular impairment.
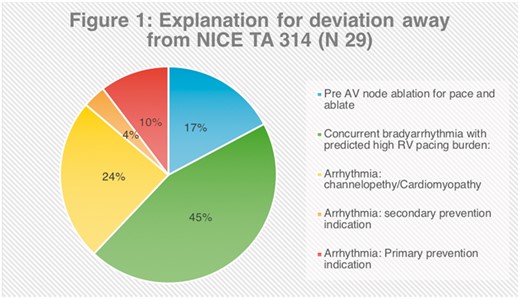
Results: Of the 533 patients included in this study, 29 cases were identified that did not fulfil the NICE TA314 criteria. Reasons for non-compliance included ejection fraction >35%, QRS <120 ms and NHYA I dyspnoea).
Discussion: Anticipated high pacing burden
According to American Heart Association Appropriate Use Criteria guidelines, de-novo CRT implantation may be considered in patients with a pre-existing or anticipated RV Pacing burden of > 40% with a clinical indication for ICD or pacemaker implantation. The European Society of Cardiology (ESC) recommend considering CRT in patients requiring permanent or frequent RV pacing for bradycardia who have symptomatic heart failure or reduced LVEF. The guideline development group points to evidence of subjective improvement, less hospitalisation and improved cardiac function as justification to upgrade from conventional pacemaker to CRT. Evidence that CRT is indicated in HF patients with LVEF <35% and high percentage of ventricular pacing who remain symptomatic despite adequate medical treatment is given a class I B status. The EHA/HRA guidelines reflect this general consensus with the caveat that the operator should be well trained in the procedure.
Arrhythmia
Due to significant crossover, it was found that many of the patients who did not meet NICE TA314 criteria for heart failure did in fact meet NICE TA314 criteria for arrhythmia. These include:
Treating people who have survived a VT or VF cardiac arrest.
Spontaneous sustained VT causing syncope or significant haemodynamic compromise.
Sustained VT without syncope or cardiac arrest but LVEF of 35% and no worse than NYHA class III heart failure.
Familial cardiac condition with a high risk of sudden death.
Conclusion: NICE Technology Appraisal 314 continues to play a critical role in the selection of patients for complex device therapy. This audit demonstrated that 95% of patient included in this audit were fully compliant with NICE TA314 criteria. On further inspection of the 5% who initially appeared to be non-compliant, the most common reason for this was concurrent bradyarrhythmia with predicted high RV pacing burden. However, AHA and ESC guidelines now support the use of CRT in this situation.
- cardiac arrhythmia
- artificial cardiac pacemaker
- cardiac arrest
- left ventricular ejection fraction
- sudden death
- syncope
- tachycardia, ventricular
- hemodynamics
- bradycardia
- sudden cardiac death
- sustained ventricular tachycardia
- cardiac pacemaker implantation
- dyspnea
- cardiology
- heart diseases
- implantable defibrillators
- heart failure
- left ventricle
- american heart association
- osteopathic manipulation
- guidelines
- heart
- morbidity
- mortality
- secondary prevention
- cardiac function
- ejection fraction
- left ventricular systolic dysfunction
- structural disorder of heart
- medical devices
- inspection
- ventricular pacing
- qrs complex duration
- functional status
- new york heart association classification
- consensus
- appropriate use
- medical management
- european society of cardiology
- fiberoptic examinations anoscopy high resolution



