-
PDF
- Split View
-
Views
-
Cite
Cite
L O'Neill, S E Williams, J Whitaker, I Sim, R Mukherjee, J Harrison, J Julia, C Sugihara, S Niederer, M Wright, A Frigiola, M O'Neill, 94
Characterisation of arrhythmia triggers in atrial septal defects: Patterns of atrial ectopy on continuous holter monitoring, EP Europace, Volume 20, Issue suppl_4, October 2018, Page iv42, https://doi.org/10.1093/europace/euy205.035Close - Share Icon Share
Background: Atrial fibrillation (AF) is common in atrial septal defect patients (ASD) but little is known about the triggers for these arrhythmias.
Hypothesis: Since right atrial dilatation is well described in ASD patients we hypothesised that atrial ectopy in ASD patients would be predominantly right-sided in origin.
Objective: To determine the origin of ectopy recorded on continuous Holter monitoring in ASD patients compared to atrial fibrillation (AF) patients with structurally normal hearts (non-congenital heart disease atrial arrhythmia (NCHD-AA) patients).
To identify echo and CMR parameters associated with ectopy in an ASD population.
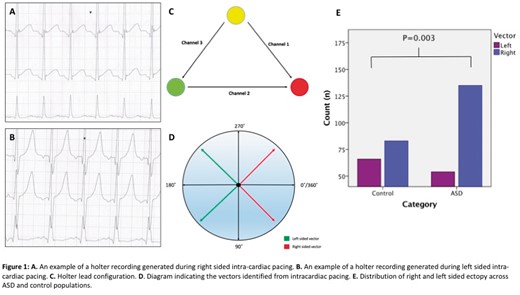
Methods: The origin of atrial ectopic beats was determined by measuring P wave amplitude in three Holter leads and calculating the axis for each ectopic beat. Invasive validation was performed by calculating P wave axes recorded on Holter monitoring during intracardiac pacing from multiple right and left atrial sites in patients with structurally normal hearts undergoing catheter ablation. Haemodyanmic parameters from echo/MRI and invasive catherisation, when available, were recorded in the ASD patients and correlated with arrhythmia occurrence and atrial ectopic burden.
Results: Analysis of Holter monitoring P wave vectors during intra-cardiac pacing across 35 sites demonstrated that a vector between 90˚ and 270˚ had a 90.5% sensitivity and 85.7% specificity for predicting an ectopic beat of left sided (vs right sided) origin. Therefore, ectopic P waves with a vector angle of 90-270˚ were considered left sided while those with an angle of 0-90˚ or 270-360˚ were considered right sided. 189 ectopic beats were analysed in 33 ASD patients (14 male, mean age 50.1 ± 16.9 years). 149 ectopic beats were analysed in 37 NCHD-AA patients (21 male, mean age 61.6 ± 10.5). Right sided ectopy accounted for 71.4% of all ectopic beats studied in the ASD population and was significantly more prevalent in ASD patients than NCHD-AA patients (p = 0.003). Qp: Qs was significantly associated with the presence of documented atrial arrhythmias in ASD patients (P = 0.04). Overall ectopic burden over 24 hours correlated significantly with LA size by 2 D echo (R = 0.464, P = 0.008).
Conclusion: Right-sided ectopy is more prevalent in ASD patients compared to NCHD-AA patients. This data suggests that arrhythmia triggers are more likely to be right-sided in origin compared to NCHD-AA patients. Further investigation is required to determine the role of right-sided ablation as an adjunct to pulmonary vein isolation in ASD patients with AF.