-
PDF
- Split View
-
Views
-
Cite
Cite
M Proietti, KEJ Airaksinen, A Rubboli, A Schlitt, T Kiviniemi, P P Karjalainen, GYH Lip, P1177
Impact of incomplete revascularization in atrial fibrillation patients undergoing percutaneous coronary intervention: the afcas registry, EP Europace, Volume 20, Issue suppl_1, March 2018, Page i227, https://doi.org/10.1093/europace/euy015.662Close - Share Icon Share
On behalf of: AFCAS Study Group
Funding Acknowledgements: None related to this analysis.
Background: Patients with atrial fibrillation (AF) often have associated coronary artery disease (CAD) and undergo percutaneous coronary intervention and stent (PCI-S) procedures. When performing PCI-S in patients with CAD, use of an incomplete revascularization (IR) vs. complete revascularization (CR) strategy has been debated, but limited data on AF patients are available. We aimed to describe clinical factors associated with use of an IR strategy and the relationship to clinical outcomes in a prospective cohort of AF patients undergoing PCI-S.
Methods: Sub-group analysis from the AFCAS registry. All patients with complete data about revascularization strategy were considered for this analysis.
Results: From the overall AFCAS cohort of 975 patients, 950(97.4%) were eligible for this analysis. Of these, 445(46.8%) were managed with a IR strategy, while the remaining 505(53.2%) were managed with a CR strategy. Patients with a IR strategy were older compared to those treated with CR (median age 75 [IQR 70-79] vs. 73 [67-77], p<0.001) and more commonly had non-paroxysmal AF (65.7% vs. 58.4%, p=0.023). IR patients had a higher thromboembolic risk profile (Median CHA2DS2-VASc score 4 [3-5] vs. 3 [2-4], p<0.001). Multivariate logistic regression analysis found that age (odds ratio [OR]: 1.03, 95% confidence interval [CI]: 1.01-1.05 per year), non-paroxysmal AF (OR: 1.53, 95% CI: 1.14-2.07), history of coronary artery disease (OR: 2.20, 95% CI: 1.63-2.98) and history of stroke/transient ischemic attack (OR: 1.57, 95% CI: 1.06-2.33) were associated with IR. At 1-year follow-up, IR patients had a higher rate of the composite outcome of acute myocardial infarction (AMI)/ stent thrombosis (ST)/Revascularization, compared to patients with CR (13.9% vs. 9.4%, p=0.003). No differences were found for thromboembolic events, major bleeding and cardiovascular or all-cause death rates. Kaplan-Meier analysis shows that patients with IR (black line) approach had a higher risk for AMI/ST/Revascularization outcome (Log-rank: 4.430, p=0.035) [Figure]. A Cox regression analysis, adjusted for age, gender, creatinine clearance (as Cockroft-Gault equation), type of AF, CHA2DS2-VASc score and antithrombotic therapy, shows that only creatinine clearance (hazard ratio [HR]: 0.99, 95% CI: 0.99-1.00, p=0.031) and IR were independently associated with a higher risk of AMI/ST/Revascularization (hazard ratio: 1.66, 95% CI: 1.10-2.50, p=0.013).
Conclusions: Use of an IR approach in AF was associated with older age, non-paroxysmal AF and more clinically severe cardiovascular or cerebrovascular disease. Use of an IR approach was independently associated with a higher risk for cardiac-related adverse outcomes.
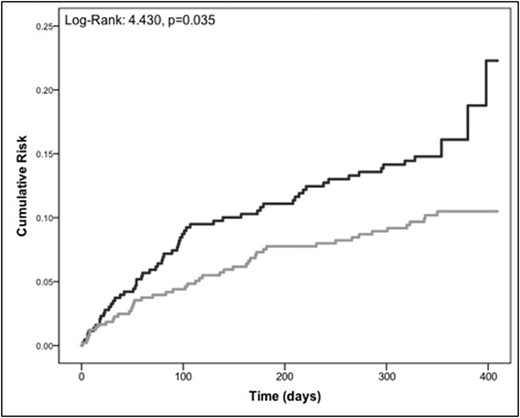
Abstract P1177 Figure. Kaplan-Meier Curves



