-
PDF
- Split View
-
Views
-
Cite
Cite
M Proietti, GYH Lip, 674
Relation of Nonsteroidal Anti-Inflammatory Drugs and Time in Therapeutic Range in Bleeding Risk in Atrial Fibrillation: the SPORTIF Trials, EP Europace, Volume 20, Issue suppl_1, March 2018, Page i112, https://doi.org/10.1093/europace/euy015.320Close - Share Icon Share
Background: Use of nonsteroidal anti-inflammatory drugs (NSAIDs) in atrial fibrillation (AF) patients is associated with an increased risk of major bleeding. Time in therapeutic range (TTR) is a main determinant of major adverse outcomes in AF, both thromboembolic and major bleeding events.
Objective: To evaluate if the use of NSAIDs in association with poor quality of anticoagulation control (assessed by TTR), is associated with a higher risk of bleeding in AF patients.
Methods: All patients assigned to the warfarin arm of the SPORTIF III and V trials with data available about NSAIDs and TTR. TTR ≤65% was used to define poor quality of anticoagulation control.
Results: A total of 3624 patients were available for this analysis. Of these 1540 (42.0%) did not use NSAIDs and reported a TTR >65% [Group I]; 1108 (30.2%) did not use NSAIDs and had a TTR ≤65% [Group II]; 552 (15.1%) were NSAIDs users with a TTR >65% [Group III]; and 424 (11.6%) were both NSAIDs users and had a TTR ≤65% [Group IV]. At baseline, the prevalence of HAS-BLED ≥3 was progressively higher across the four groups (51.1% vs. 83.7% vs. 83.0% vs. 99.0%; p<0.001). After a mean (SD) follow-up of 1.55 (0.38) years, 128 (3.5%) major bleeding, 163 (4.5%) major/clinically-relevant non-major (CRNM) bleeding and 1471 (40.6%) any bleeding event were reported. Event rates according to the four groups were reported in the Figure. For all the outcomes patients in Group IV (i.e. NSAIDs users with TTR ≤65%) reported the higher adverse events. Kaplan-Meier curves confirmed that patients in Group IV had the highest risk for bleeding events (all p<0.001). A Cox regression model, adjusted for age, sex, creatinine clearance, type of AF and HAS-BLED score showed that Group II and Group IV had an independently higher risk for major bleeding (hazard ratio [HR]: 1.75, 95% confidence interval [CI]: 1.12-2.74 and HR: 3.19, 95% CI: 1.96-5.20, respectively) and major/CRNM bleeding (HR: 1.61, 95% CI: 1.09-2.37 and HR: 2.74, 95% CI: 1.79-4.20, respectively). For the occurrence of any bleeding both patients in Group III and Group IV were independently at higher risk (HR: 1.22, 95% CI: 1.05-1.42 and HR: 1.35, 95% CI: 1.13-1.61, respectively).
Conclusions: In a cohort of anticoagulated AF patients, use of NSAIDs together with a poor quality of anticoagulation control was associated an increased risk of all bleeding outcomes.
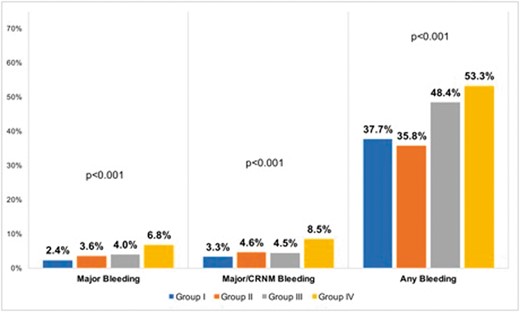
Abstract 674 Figure. Bleeding Event Rates



