-
PDF
- Split View
-
Views
-
Cite
Cite
Stefano Fumagalli, Jian Chen, Dan Dobreanu, Antonio Hernandez Madrid, Roland Tilz, Nikolaos Dagres, The role of the Arrhythmia Team, an integrated, multidisciplinary approach to treatment of patients with cardiac arrhythmias: results of the European Heart Rhythm Association survey, EP Europace, Volume 18, Issue 4, April 2016, Pages 623–627, https://doi.org/10.1093/europace/euw090
Close - Share Icon Share
Abstract
Management of patients with cardiac arrhythmias is increasingly complex because of continuous technological advance and multifaceted clinical conditions associated with ageing of the population, the presence of co-morbidities and the need for polypharmacy. The aim of this European Heart Rhythm Association Scientific Initiatives Committee survey was to provide an insight into the role of the Arrhythmia Team, an integrated, multidisciplinary approach to management of patients with cardiac arrhythmias. Forty-eight centres from 18 European countries replied to the Web-based questionnaire. The presence of an Arrhythmia Team was reported by 44% of the respondents, whereas 17% were not familiar with this term. Apart from the electrophysiologist, health professionals who should belong to such teams, according to the majority of the respondents, include a clinical cardiologist, a nurse, a cardiac surgeon, a heart failure specialist, a geneticist, and a geriatrician. Its main activity should be dedicated to the management of patients with complex clinical conditions or refractory or inherited forms of arrhythmias. When present, the Arrhythmia Team was considered helpful by 95% of respondents; the majority of centres (79%) agreed that it should be implemented. The Arrhythmia Team seems to be connected to important expectations in the management of cardiac arrhythmias. The efficacy of such an integrated and multidisciplinary approach should be encouraged and tested in clinical practice.
Introduction
The management of cardiac arrhythmias in a particular patient can extend for several years and includes a variety of treatments and procedural interventions, which are more and more complicated, mirroring technological advances.1,2 Furthermore, the clinical conditions of patients are increasingly complex because of the influence of ageing, the presence of significant co-morbidities, and polypharmacy. For these reasons, diagnostic or therapeutic procedures can produce important benefits but also complications, which are not limited to the heart. An integrated team approach including different health professionals may provide a personalized and possibly more effective treatment plan for the individual patient. Experience gained from other medical specialties have already demonstrated the benefit of such a methodology in terms of survival and reduction of disability and costs.3 The aim of this European Heart Rhythm Association (EHRA) survey is to provide an insight into the current clinical practice regarding the presence and role of such ‘arrhythmia teams’ in the European electrophysiology (EP) centres.
Methods and results
This survey was based on a questionnaire sent via Internet to the EHRAEP Research Network centres. Forty-nine centres from 18 European countries responded. University hospital represented the majority of the respondents (n = 39, 80%), the remaining centres were private non-academic centres and hospitals of other type. After quality check, we excluded from the analysis all or some of the answers from two respondents.
Structure and responsibilities of the Arrhythmia Team
The vast majority of the respondents (n = 34, 71%) believe in the importance of co-operation with other health professionals. Teamwork is considered necessary only for difficult cases by 11 respondents (23%), but collaboration rarely is considered helpful in the case of unsatisfactory results or complications of treatment, or not useful at all (n = 1, 2% in each case).
The Arrhythmia Team has been established in 21 (44%) of the centres. A further 40% (n = 19) of the respondents are aware of this model, but do not currently have such a team in their own hospital. Only a minority (n = 8, 17%) was not familiar with the term at all. The responses regarding the structure of the Arrhythmia Team are shown in Figure 1. Apart from the electrophysiologist and a non-invasive arrhythmia specialist, the majority of the respondents believe that clinical cardiologists and heart failure specialists, cardiac surgeons, and dedicated nurses should form such teams. A significant proportion of the respondents feel that the structure of the team should more frequently include a geneticist, a geriatrician, a psychologist, and a general practitioner (Figure 1).

Replies regarding the proposed composition of the Arrhythmia Team by respondents working in centres with (turquoise bars) and without (red bars) the Arrhythmia Team. Electrophysiol, invasive electrophysiologist; Arrhythmia, non-invasive arrhythmia specialist; Heart Failure, heart failure specialist; Surgeon, cardiac surgeon; Gerontologist, geriatrician; GP, general practitioner; Other HP, other health professionals.
The vast majority of respondents believe that the responsibility of the Arrhythmia Team should include management of difficult patients with refractory forms of ventricular tachycardia and atrial fibrillation (AF), or with complex clinical conditions, such as those with multiple co-morbidities, frailty, and complicated therapeutic schemes. Team members should also take care of subjects with inherited arrhythmias. Opinions are divided regarding the indications for implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) devices, whereas decisions on pacemaker implantation and the daily management of rhythm disorders (e.g. choice between rate- and rhythm-control strategy for AF, anticoagulation management, etc.) are considered the potential tasks of such teams by only a minority of the respondents (Figure 2).
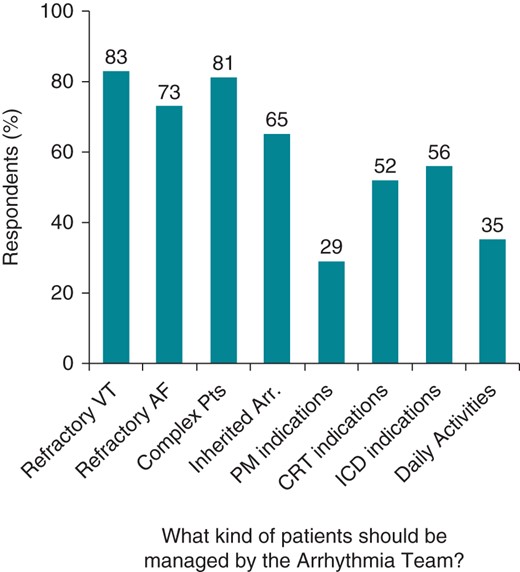
Replies regarding the tasks of the Arrhythmia Team. Refractory VT/AF, refractory forms of ventricular tachycardia/atrial fibrillation; Pts, patients; Arr., arrhythmias; PM, pacemaker; Daily Activities, activities such as rate- and rhythm-control strategy, anticoagulant management of atrial fibrillation, choice of anti-arrhythmic therapy.
The role of the Arrhythmia Team in management of patients with atrial fibrillation
For patients with AF, the decisions on invasive procedures such as catheter ablation or atrioventricular nodal ablation or surgical treatment are the two main therapeutic options considered important to be discussed within the Arrhythmia Team by 70 and 64% centres, respectively. In particular, when asked about heart surgery, approximately half the respondents replied that the cardiac surgeon should choose together with the electrophysiologist the most appropriate intervention (i.e. catheter vs. surgical ablation; n = 24, 51%), should contribute to the decision on the left atrial appendage excision or exclusion (n = 26, 55%), or the indication for a Maze procedure (n = 26, 55%), and should assist in the management of major complications of invasive AF therapy (n = 27, 57%). Only a small minority (n = 3, 6%) considers that the cardiac surgeon should decide without consulting other health professionals. A multidisciplinary approach for AF is felt necessary for the management of risk factors and lifestyle changes, psychological support, and health-related quality-of-life issues by 45 and 42% of the respondents, respectively.
In the majority of responding centres (n = 35, 74%), nurses currently do not participate in the Arrhythmia Team or direct patient follow-up. However, a significant proportion of the respondents recognize the potential role of nurses to identify barriers hampering the appropriate management of patients and to promote the interaction with physicians (n = 33, 70%), to perform regular follow-up visits (n = 35, 74%), and to facilitate the optimization of therapy (i.e. INR or risk factors control, dietary advice; n = 29, 62%).
The Arrhythmia Team in management of heart failure patients
According to the participating centres, an electrophysiologist and a clinical cardiologist should always participate in the decision on implantation of CRT devices and ICDs (Figure 3). In this context, a heart failure specialist is also considered by the majority to have a role in the Arrhythmia Team, especially when discussing the indications for CRT. One third of the respondents think that the opinion of a geriatrician is important. Regarding the ICD use, only a minority of the participants feel the need to involve a specialist in intensive care, a geneticist, a psychologist, and a specialist in palliative care in the decision-making process. Furthermore, ∼50% of the responses indicated that patients and their relatives should take an active part in the discussion about the use of such devices (Figure 3).
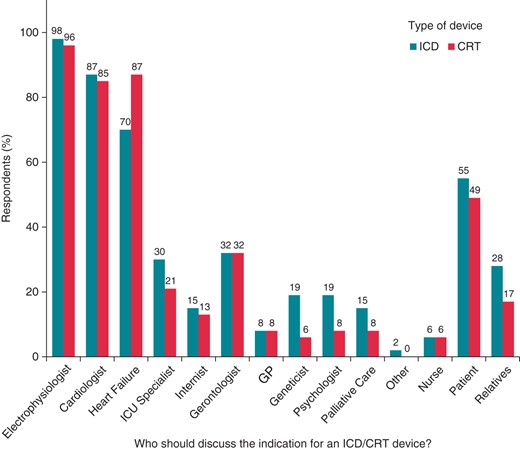
Replies regarding the proposed composition of the Arrhythmia Team when discussing the indications for ICD (turquoise bars) or CRT devices (red bars) implantation. Electrophysiologist, invasive electrophysiologist; Heart Failure, heart failure specialist; ICU Specialist, specialist in intensive care; Gerontologist, geriatrician; GP, general practitioner; Palliative Care, specialist in palliative care; Other, other specialists.
A significant proportion of the respondents agree on the role of cardiac surgeons in the planning of surgical ablation of refractory ventricular arrhythmias (n = 29, 62%), designing the strategy for device or lead explantation (n = 21, 45%), and management of major complications of invasive rhythm control therapy (n = 32, 68%). The cardiac surgeon could also be useful to identify patients suitable for implantation of a subcutaneous ICD (n = 8, 17%).
The great majority of respondents believe that the Arrhythmia Team should be implemented in every centre (n = 37, 79%; Figure 4). Only a tiny minority (n = 2; 4%) feels that it would not provide valid help in addressing the difficult situations, whereas 8 (17%) respondents consider its formal presence not necessary, because an integrated, multidisciplinary response is already achievable when needed.
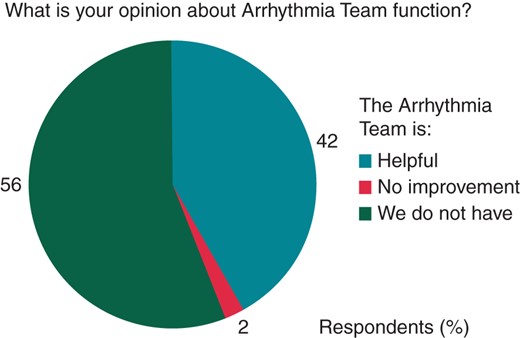
Replies regarding the responses on the effective utility of the Arrhythmia Team. No improvement, ‘I support its existence, but it has not led to a considerable improvement of patients’ management’; We do not have, ‘We do not have an arrhythmia team’.
Discussion
The responses to this EP Wire survey clearly demonstrate the acknowledgement of the importance of an integrated multidisciplinary approach to the management of patients with cardiac arrhythmias in challenging clinical situations. Despite this recognition, an Arrhythmia Team is implemented in <50% of the respondent centres, and even if many participants are aware of its existence in other hospitals or universities, the term is completely unfamiliar to a considerable number of arrhythmia specialists. The need for a multidisciplinary approach is deemed unnecessary for routine decision-making such as pacemaker implantation or routine arrhythmia management, but rather for the treatment of complex and refractory forms of the arrhythmia and for patients presenting with many co-morbidities, frail conditions, and polypharmacy.
Some evidence seems to support the existence of the Arrhythmia Team in clinical practice. It has been demonstrated that a multidisciplinary approach to AF management, covering all aspects of care, including baseline evaluation, education, therapy, and follow-up could significantly reduce the incidence of arrhythmia-related hospitalizations and of stroke.4,5 More recently, the multicentre Standard versus Atrial Fibrillation-spEcific managemenT strategY (SAFETY) study compared the effects of a nursing intervention, consisting of home visits, Holter monitoring, and a potential multidisciplinary support, with those of a standard one, in subjects with non-valvular forms of the arrhythmia. Actively treated patients spent more days alive and out of hospital during a long-term follow-up.6
The importance of a multidisciplinary approach in the ICD or CRT-D population is outlined in the multicentre INfluence of home moniToring on mortality and morbidity in heart failure patients with IMpaired lEftventricular function (IN-TIME) trial, which evaluated the incremental benefit of a multiparameter telemonitoring, reviewed by a team composed of specialized nurses and physicians vs. standard care. If necessary, the team could trigger a local response aimed at assessing patient's conditions and compliance with therapy, and at recommending follow-up visits. After 1-year, mortality was lower in the telemonitoring group than in the control one.7
Regarding the structure of the Arrhythmia Team, the majority, as expected, responded that an invasive electrophysiologist, a non-invasive arrhythmia specialist, a clinical cardiologist, a heart failure specialist, a cardiac surgeon, and a dedicated nurse should be part of such a team. Interestingly, a significant proportion replied that also other health professionals such as a geneticist, a geriatrician, a psychologist, and a specialist in palliative care should be members of the team. Several factors may explain this. The role of a geneticist is supported by technology developments that have definitely clarified how altered expression of atrial ion channels, due to genetic alterations, can predispose patients to AF and influence the response to anti-arrhythmic drugs.8 Importantly, inherited arrhythmias associated with structurally normal heart (i.e. long and short QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, etc.) can explain 10% of all sudden deaths in Europe and USA and justify specific management and ICD indications.9,10
The ageing process of the population and the related increasing burden of AF, supraventricular tachycardias, and sudden cardiac death11 may explain why the presence of a geriatrician was felt necessary by 38% of the respondents. Some important issues are tightly associated with age. Undertreatment is common in elderly individuals. The findings of the EURObservational Research Programme-Atrial Fibrillation General Pilot Registry have clearly shown that an age of ≥75 years was significantly associated with a lower use of oral anticoagulants despite a higher cardio-embolic risk12 and an evident net clinical benefit, observed also in subjects >90 years.13 Undertreatment is often motivated by the presence of several co-morbid conditions.12,14,15 Furthermore, more than one-third of the respondents recognized the importance of a geriatrician in the decision-making process leading to CRT and ICD implantation.
About 25% of respondents to the EP Wire survey thought that the psychologist should also be a member of the Arrhythmia Team. This is supported by the results of The Atrial Fibrillation and Congestive Heart Failure (AF-CHF) trial, which showed a prevalence of depressive symptoms in as high as 32% of patients with the arrhythmia. Interestingly, cardiovascular and all-cause mortality was significantly associated with the presence of a depressive disorder even after adjustment for confounders.16 The impact of ICD/CRT therapy on psychology is relevant and insufficiently explored.17 Finally, 15% respondents thought that additionally a specialist in palliative care should have a role in the multidisciplinary management of ICD patients. The high risk of unnecessary and painful shocks near-end of life may explain this finding.18
Conclusion
In conclusion, the Arrhythmia Team is present in less than half the centres responding to the EP Wire survey. Nevertheless, the significant majority think that it is useful and should be implemented. A multidisciplinary approach involving a wide range of health professionals could facilitate the management of patients with complex arrhythmic problems.
Funding
Conflict of interest: none declared.
Acknowledgements
The production of this EP wire document is under the responsibility of the Scientific Initiative Committee of the European Heart Rhythm Association: Nikolaos Dagres (chair), Tatjana S. Potpara (co-chair), Serge Boveda, Jian Chen, Jean Claude Deharo, Dan Dobreanu, Stefano Fumagalli, Kristina Haugaa, Torben Bjeregaard Larsen, Radosław Lenarczyk, Antonio Madrid, Elena Sciaraffia, Milos Taborsky, and Roland Tilz. Document reviewer for EP-Europace: Irene Savelieva (St George's University of London, London, UK). The authors acknowledge the EHRA Research Network centres participating in this EP Wire. A list of the Research Network can be found on the EHRA website.



