-
PDF
- Split View
-
Views
-
Cite
Cite
Angel Arenal, Alessandro Proclemer, Axel Kloppe, Maurizio Lunati, José Bautista Martìnez Ferrer, Ahmad Hersi, Marcin Gulaj, Maurits C.E.F. Wijffels, Elisabetta Santi, Laura Manotta, Lorenza Mangoni, Maurizio Gasparini, Different impact of long-detection interval and anti-tachycardia pacing in reducing unnecessary shocks: data from the ADVANCE III trial, EP Europace, Volume 18, Issue 11, November 2016, Pages 1719–1725, https://doi.org/10.1093/europace/euw032
Close - Share Icon Share
A long-detection interval (LDI) (30/40 intervals) has been proved to be superior to a standard-detection interval (SDI) (18/24 intervals) in terms of reducing unnecessary implantable cardioverter defibrillator (ICD) therapies. To better evaluate the different impact of LDI and anti-tachycardia pacing (ATP) on reducing painful shocks, we assessed all treated episodes in the ADVANCE III trial.
A total of 452 fast (200 ms < cycle length ≤ 320 ms) arrhythmic episodes were recorded: 284 in 138 patients in the SDI arm and 168 in 82 patients in the LDI arm (106/452 inappropriate detections). A total of 346 fast ventricular tachycardias (FVT) were detected in 169 patients: 208 in 105 patients with SDI and 138 in 64 patients with LDI. Setting LDI determined a significant reduction in appropriate but unnecessary therapies [208 in SDI vs. 138 in LDI; incidence rate ratio (IRR): 0.61 (95% CI 0.45–0.83), P = 0.002]. Anti-tachycardia pacing determined another 52% reduction in unnecessary shocks [208 in SDI with hypothetical shock-only programming vs. 66 in LDI with ATP; IRR: 0.37 (95% CI 0.25–0.53, P < 0.001)]. The efficacy of ATP in terminating FVT was 63% in SDI and 52% in LDI (P = 0.022). No difference in the safety profile (acceleration/degeneration and death/cardiovascular hospitalizations) was observed between the two groups.
The combination of LDI and ATP during charging is extremely effective and significantly reduces appropriate but unnecessary therapies. The use of LDI alone yielded a 39% reduction in appropriate but unnecessary therapies; ATP on top of LDI determined another 52% reduction in unnecessary shocks. The strategy of associating ATP and LDI could be considered in the majority of ICD recipients.
This is the first study to explore the efficacy of anti-tachycardia pacing (ATP) in combination with prolonged detection.
Anti-tachycardia pacing efficacy remains as high as 52% when used after long detection, without impacting hospitalizations or deaths.
The reduction in unnecessary shocks reported in the ADVANCE III trial is due to a combination of the use of long-detection programming and a single ATP attempt during charge.
Introduction
The implantable cardioverter defibrillator (ICD) has improved survival in patients at high risk of ventricular arrhythmias.1–4 However, ICD shocks may increase morbidity and mortality.5 Non-randomized studies have suggested that long-detection intervals (LDI) can reduce device therapies.6,7 This has been proved by recent clinical trials, which have reported that a high-rate cut-off and a LDI reduce the overall number of therapies delivered by ICD in primary and secondary prevention of sudden cardiac death.8,9 The MADIT-RIT trial reported that high-rate cut-off therapy [a single ventricular tachycardia (VT) zone for VT ≥ 200 b.p.m.] was associated with reductions in inappropriate therapies and all-cause mortality, while an LDI determined a reduction in total anti-tachycardia pacing (ATP) and inappropriate shocks during long-term follow-up.8 In the ADVANCE III trial, the LDI strategy reduced overall ICD therapies, inappropriate shocks, and hospitalization rates and costs in comparison with a standard-detection interval (SDI).9,10
Regardless of the timing of delivery, both ATP and shocks may have side effects; while ATP may induce VTs when delivered during supraventricular tachycardia, or accelerate/degenerate true VTs, repeated shocks have been associated with a poor quality of life and prognosis.5 In the light of the MADIT-RIT and ADVANCE III data, it has recently been hypothesized that the simple high-rate (HR) cut-off and/or LDI window might be sufficient to adequately reduce inappropriate or unnecessary therapies.11,12 This approach minimizes the importance of ATP in reducing avoidable therapies, which has been historically recognized on the basis of clearly demonstrated evidence.13,14
In order to obtain new insights into the possible different impact on reducing appropriate but unnecessary therapies by means of LDI or ATP alone, we separately analysed the different effects of programming an LDI and/or using ATP in the large ADVANCE III database. Long-detection interval avoids therapies for non-sustained arrhythmias, but delays ATP delivery for sustained fast VT (FVT) with cycle length (CL) between 200 and 320 ms; this might theoretically reduce the efficacy of ATP or of subsequent shocks if ATP fails.15 The efficacy and safety of ATP/shock therapy were therefore evaluated in the ADVANCE III database.
Methods
Study overview and patient selection
The design and results of the ADVANCE III trial have been published previously.9,10 Briefly, the ADVANCE III trial was a randomized, single-blind, parallel, multi-centre trial that enrolled and analysed 1902 patients undergoing their first implantation of a single-/dual-chamber ICD or a biventricular ICD (cardiac resynchronization therapy defibrillator). All devices were able to deliver ATP during capacitor charge, in order not to delay the high-energy therapy. Patients were randomly assigned to be programmed with a long-detection setting or with the standard-interval programming and were followed up for 1 year.
Device programming
Devices were programmed to deliver a single ATP burst during capacitor charge, followed by shocks when the VT CL was ≥200 and ≤320 ms, and shocks only for VF with CL < 200 ms. Patients were randomized to the standard-detection programming used in the PainFREE II trial14 (18/24 intervals) or to long-detection programming (30/40 intervals).16 A VT zone was programmed when a slow VT with CL > 320 ms had previously been recorded; therapy programming was tailored by the physician to the recorded VT.
Study objectives
For the purpose of these analyses, we considered a subgroup of patients from the ADVANCE III population who had received at least one ATP for appropriate episodes with CL between 200 and 320 ms during follow-up.
The primary endpoint of this study was to determine the separate ability of LDI alone and ATP alone to reduce appropriate but unnecessary ICD therapies in this subset of the ADVANCE III population.
Secondary endpoints were to determine
(1) the efficacy of a therapeutic approach combining ATP during charge with first shock in the two groups;
(2) the efficacy of ATP and the efficacy of the first shock delivered after unsuccessful ATP;
(3) safety of ATP, on considering true FVT accelerations/degenerations or VT inductions (if ATP delivered during supraventricular rhythm); and
freedom from death or cardiovascular hospitalization.
Definitions
(1) Appropriate therapy: therapy delivered for monomorphic or polymorphic FVT/VF.
(2) Inappropriate therapy: therapy delivered for supraventricular episodes or for non-arrhythmic events.
(3) Appropriate but unnecessary therapy: therapy delivered for VT which may either self-terminate or be terminated by ATP, in the case of shock.
(4) Anti-tachycardia pacing efficacy: percentage of FVT episodes terminated by ATP.
(5) Anti-tachycardia pacing safety: percentage of FVT accelerated by ATP and percentage of VT induced by ATP delivered inappropriately.
(6) First-shock efficacy: percentage of first shocks that terminated a FVT unresponsive to ATP.
(7) Successful ATP therapy: ATP was deemed successful when the post-therapy rhythm was not a ventricular tachyarrhythmia.
(8) Acceleration was defined as a 10% decrease in FVT CL after the first ATP attempt.
Statistical methods
Details of sample size calculation, the randomization process, and data collection have been previously described.16 Continuous data are expressed as means and standard deviations, whereas categorical data are expressed as counts and percentage. The homogeneity of baseline characteristics was assessed by means of t-test and χ2 test for continuous and categorical variables, respectively. Rates of total ATP delivered and rates of patients treated with at least one ATP were compared by means of the incidence rate ratio (IRR) and 95% confidence interval (95% CI). An IRR of <1 would indicate a higher incidence of ATP in the SDI group. In order to adjust for multiple episodes per patient, ATP efficacy was adjusted by means of the generalized estimating equation (GEE) method and compared by means of logistic regression. Odd ratios (ORs) and 95% CI were used to compare treatment efficacy in the LDI and SDI groups. An OR of <1 would indicate higher efficacy in the SDI group. Results are presented for all episodes detected and, separately, for appropriately and inappropriately treated episodes, structural heart disease and type of device. Survival was traced by means of Kaplan–Meier curves and compared between the groups by means of the log-rank test. All analyses were performed according to the intention-to-treat approach. All tests were two-sided and a two-tailed P-value of <0.05 was considered to indicate statistical significance. Analyses were performed by means of Stata 12.1 (Stata Corporation, College Station, TX, USA).
Results
Of the total 1902 randomized patients, 220 (138 in SDI arm and 82 in LDI arm) had at least one spontaneous episode appropriately and/or inappropriately treated with ATP during a mean follow-up of 12 months.
A significantly lower number of patients in the LDI arm were treated, 9.9% (95% CI 7.9–12.3) vs. 16.6% (95% CI 14.0–19.6) patients/year in SDI [IRR: 0.60 (95% CI 0.49–0.73), P < 0.001]. Treated patients were mostly male (87.7% in SDI and 92.7% in LDI); the mean age of patients was 63 years (63 ± 13 in SDI and 63 ± 12 in LDI), the mean QRS was prolonged (121 ± 32 ms in SDI and 124 ± 37 ms in LDI), and the mean ejection fraction was reduced (31 ± 12% in SDI and 31 ± 10% in LDI). Table 1 shows the baseline characteristics of both groups. The 220 patients experienced a total of 452 episodes treated with at least one ATP, 346 (76.5%) being appropriately detected.
Baseline characteristics of patients with at least one episode treated with anti-tachycardia pacing
| . | Standard detection (n = 138) . | Long detection (n = 82) . | P-value . |
|---|---|---|---|
| Patient demographics | |||
| Age | 63 (±13) | 63 (±12) | 0.935 |
| Male gender | 121 (87.7%) | 76 (92.7%) | 0.173 |
| Medical history | |||
| Secondary prevention | 48 (34.8%) | 34 (41.5%) | 0.198 |
| VF/V flutter | 18 (13.0%) | 142 (17.1%) | 0.265 |
| Sustained VT history | 30 (21.7%) | 24 (29.3%) | 0.137 |
| Permanent atrial fibrillation | 25 (18.1%) | 14 (17.1%) | 0.499 |
| History of syncopal episodes | 37 (26.8%) | 15 (18.3%) | 0.100 |
| NYHA Class III or IV | 59 (42.8%) | 40 (48.8%) | 0.233 |
| Angina | 17 (12.4%) | 13 (15.9%) | 0.301 |
| Coronary artery disease | 63 (45.6%) | 45 (54.9%) | 0.118 |
| Previous revascularization | 40 (29.0%) | 32 (39.0%) | 0.083 |
| QRS (ms) | 121 (±32) | 124 (±37) | 0.813 |
| LBB | 33 (23.9%) | 22 (26.8%) | 0.371 |
| Hypercholesterolemia | 62 (44.9%) | 46 (56.8%) | 0.060 |
| Diabetes | 32 (23.2%) | 21 (25.6%) | 0.401 |
| Chronic kidney disease | 11 (8.0%) | 9 (11.0%) | 0.302 |
| Baseline echo-cardiographic measures | |||
| Mitral regurgitation (III/IV) | 16 (18.2%) | 6 (12.5%) | 0.273 |
| LVEF (%) | 31 (±12) | 31 (±10) | 0.290 |
| LVDD (mm) | 64 (±9) | 63 (±8) | 0.489 |
| Baseline medication therapy | |||
| ACE inhibitors/ARBII | 108 (78.3%) | 67 (81.7%) | 0.333 |
| Anti-platelets | 68 (49.3%) | 41 (50.0%) | 0.514 |
| Anti-coagulants | 52 (37.7%) | 31 (37.8%) | 0.549 |
| Anti-arrhythmics | 30 (21.7%) | 14 (17.1%) | 0.256 |
| β-Blockers | 110 (79.7%) | 58 (70.7%) | 0.089 |
| Cardiac glycosides | 33 (23.9%) | 14 (17.1%) | 0.152 |
| Diuretics | 110 (79.7%) | 59 (72.0%) | 0.125 |
| Hypolipidaemics | 64 (46.4%) | 44 (53.7%) | 0.183 |
| Other cardiac medications | 11 (8.0%) | 11 (13.4%) | 0.143 |
| Implanted Device | |||
| CRTD | 40 (29.0%) | 28 (34.2%) | 0.690 |
| Dual chamber | 41 (29.7%) | 24 (29.3%) | |
| Single chamber | 57 (41.3%) | 30 (36.6%) | |
| . | Standard detection (n = 138) . | Long detection (n = 82) . | P-value . |
|---|---|---|---|
| Patient demographics | |||
| Age | 63 (±13) | 63 (±12) | 0.935 |
| Male gender | 121 (87.7%) | 76 (92.7%) | 0.173 |
| Medical history | |||
| Secondary prevention | 48 (34.8%) | 34 (41.5%) | 0.198 |
| VF/V flutter | 18 (13.0%) | 142 (17.1%) | 0.265 |
| Sustained VT history | 30 (21.7%) | 24 (29.3%) | 0.137 |
| Permanent atrial fibrillation | 25 (18.1%) | 14 (17.1%) | 0.499 |
| History of syncopal episodes | 37 (26.8%) | 15 (18.3%) | 0.100 |
| NYHA Class III or IV | 59 (42.8%) | 40 (48.8%) | 0.233 |
| Angina | 17 (12.4%) | 13 (15.9%) | 0.301 |
| Coronary artery disease | 63 (45.6%) | 45 (54.9%) | 0.118 |
| Previous revascularization | 40 (29.0%) | 32 (39.0%) | 0.083 |
| QRS (ms) | 121 (±32) | 124 (±37) | 0.813 |
| LBB | 33 (23.9%) | 22 (26.8%) | 0.371 |
| Hypercholesterolemia | 62 (44.9%) | 46 (56.8%) | 0.060 |
| Diabetes | 32 (23.2%) | 21 (25.6%) | 0.401 |
| Chronic kidney disease | 11 (8.0%) | 9 (11.0%) | 0.302 |
| Baseline echo-cardiographic measures | |||
| Mitral regurgitation (III/IV) | 16 (18.2%) | 6 (12.5%) | 0.273 |
| LVEF (%) | 31 (±12) | 31 (±10) | 0.290 |
| LVDD (mm) | 64 (±9) | 63 (±8) | 0.489 |
| Baseline medication therapy | |||
| ACE inhibitors/ARBII | 108 (78.3%) | 67 (81.7%) | 0.333 |
| Anti-platelets | 68 (49.3%) | 41 (50.0%) | 0.514 |
| Anti-coagulants | 52 (37.7%) | 31 (37.8%) | 0.549 |
| Anti-arrhythmics | 30 (21.7%) | 14 (17.1%) | 0.256 |
| β-Blockers | 110 (79.7%) | 58 (70.7%) | 0.089 |
| Cardiac glycosides | 33 (23.9%) | 14 (17.1%) | 0.152 |
| Diuretics | 110 (79.7%) | 59 (72.0%) | 0.125 |
| Hypolipidaemics | 64 (46.4%) | 44 (53.7%) | 0.183 |
| Other cardiac medications | 11 (8.0%) | 11 (13.4%) | 0.143 |
| Implanted Device | |||
| CRTD | 40 (29.0%) | 28 (34.2%) | 0.690 |
| Dual chamber | 41 (29.7%) | 24 (29.3%) | |
| Single chamber | 57 (41.3%) | 30 (36.6%) | |
Continuous data are summarized as mean (standard deviation), categorical data as counts (%).
VF, ventricular fibrillation; V flutter, ventricular flutter; VT, ventricular tachycardia; NYHA, New York Heart Association; LBB, left bundle branch block; LVEF, left ventricular ejection fraction; LVDD, left ventricular diastolic diameter; ACE inhibitors/ARBII, angiotensin-converting-enzyme inhibitor/angiotensin II receptor blockers; CRTD, cardiac resynchronization therapy defibrillator.
Baseline characteristics of patients with at least one episode treated with anti-tachycardia pacing
| . | Standard detection (n = 138) . | Long detection (n = 82) . | P-value . |
|---|---|---|---|
| Patient demographics | |||
| Age | 63 (±13) | 63 (±12) | 0.935 |
| Male gender | 121 (87.7%) | 76 (92.7%) | 0.173 |
| Medical history | |||
| Secondary prevention | 48 (34.8%) | 34 (41.5%) | 0.198 |
| VF/V flutter | 18 (13.0%) | 142 (17.1%) | 0.265 |
| Sustained VT history | 30 (21.7%) | 24 (29.3%) | 0.137 |
| Permanent atrial fibrillation | 25 (18.1%) | 14 (17.1%) | 0.499 |
| History of syncopal episodes | 37 (26.8%) | 15 (18.3%) | 0.100 |
| NYHA Class III or IV | 59 (42.8%) | 40 (48.8%) | 0.233 |
| Angina | 17 (12.4%) | 13 (15.9%) | 0.301 |
| Coronary artery disease | 63 (45.6%) | 45 (54.9%) | 0.118 |
| Previous revascularization | 40 (29.0%) | 32 (39.0%) | 0.083 |
| QRS (ms) | 121 (±32) | 124 (±37) | 0.813 |
| LBB | 33 (23.9%) | 22 (26.8%) | 0.371 |
| Hypercholesterolemia | 62 (44.9%) | 46 (56.8%) | 0.060 |
| Diabetes | 32 (23.2%) | 21 (25.6%) | 0.401 |
| Chronic kidney disease | 11 (8.0%) | 9 (11.0%) | 0.302 |
| Baseline echo-cardiographic measures | |||
| Mitral regurgitation (III/IV) | 16 (18.2%) | 6 (12.5%) | 0.273 |
| LVEF (%) | 31 (±12) | 31 (±10) | 0.290 |
| LVDD (mm) | 64 (±9) | 63 (±8) | 0.489 |
| Baseline medication therapy | |||
| ACE inhibitors/ARBII | 108 (78.3%) | 67 (81.7%) | 0.333 |
| Anti-platelets | 68 (49.3%) | 41 (50.0%) | 0.514 |
| Anti-coagulants | 52 (37.7%) | 31 (37.8%) | 0.549 |
| Anti-arrhythmics | 30 (21.7%) | 14 (17.1%) | 0.256 |
| β-Blockers | 110 (79.7%) | 58 (70.7%) | 0.089 |
| Cardiac glycosides | 33 (23.9%) | 14 (17.1%) | 0.152 |
| Diuretics | 110 (79.7%) | 59 (72.0%) | 0.125 |
| Hypolipidaemics | 64 (46.4%) | 44 (53.7%) | 0.183 |
| Other cardiac medications | 11 (8.0%) | 11 (13.4%) | 0.143 |
| Implanted Device | |||
| CRTD | 40 (29.0%) | 28 (34.2%) | 0.690 |
| Dual chamber | 41 (29.7%) | 24 (29.3%) | |
| Single chamber | 57 (41.3%) | 30 (36.6%) | |
| . | Standard detection (n = 138) . | Long detection (n = 82) . | P-value . |
|---|---|---|---|
| Patient demographics | |||
| Age | 63 (±13) | 63 (±12) | 0.935 |
| Male gender | 121 (87.7%) | 76 (92.7%) | 0.173 |
| Medical history | |||
| Secondary prevention | 48 (34.8%) | 34 (41.5%) | 0.198 |
| VF/V flutter | 18 (13.0%) | 142 (17.1%) | 0.265 |
| Sustained VT history | 30 (21.7%) | 24 (29.3%) | 0.137 |
| Permanent atrial fibrillation | 25 (18.1%) | 14 (17.1%) | 0.499 |
| History of syncopal episodes | 37 (26.8%) | 15 (18.3%) | 0.100 |
| NYHA Class III or IV | 59 (42.8%) | 40 (48.8%) | 0.233 |
| Angina | 17 (12.4%) | 13 (15.9%) | 0.301 |
| Coronary artery disease | 63 (45.6%) | 45 (54.9%) | 0.118 |
| Previous revascularization | 40 (29.0%) | 32 (39.0%) | 0.083 |
| QRS (ms) | 121 (±32) | 124 (±37) | 0.813 |
| LBB | 33 (23.9%) | 22 (26.8%) | 0.371 |
| Hypercholesterolemia | 62 (44.9%) | 46 (56.8%) | 0.060 |
| Diabetes | 32 (23.2%) | 21 (25.6%) | 0.401 |
| Chronic kidney disease | 11 (8.0%) | 9 (11.0%) | 0.302 |
| Baseline echo-cardiographic measures | |||
| Mitral regurgitation (III/IV) | 16 (18.2%) | 6 (12.5%) | 0.273 |
| LVEF (%) | 31 (±12) | 31 (±10) | 0.290 |
| LVDD (mm) | 64 (±9) | 63 (±8) | 0.489 |
| Baseline medication therapy | |||
| ACE inhibitors/ARBII | 108 (78.3%) | 67 (81.7%) | 0.333 |
| Anti-platelets | 68 (49.3%) | 41 (50.0%) | 0.514 |
| Anti-coagulants | 52 (37.7%) | 31 (37.8%) | 0.549 |
| Anti-arrhythmics | 30 (21.7%) | 14 (17.1%) | 0.256 |
| β-Blockers | 110 (79.7%) | 58 (70.7%) | 0.089 |
| Cardiac glycosides | 33 (23.9%) | 14 (17.1%) | 0.152 |
| Diuretics | 110 (79.7%) | 59 (72.0%) | 0.125 |
| Hypolipidaemics | 64 (46.4%) | 44 (53.7%) | 0.183 |
| Other cardiac medications | 11 (8.0%) | 11 (13.4%) | 0.143 |
| Implanted Device | |||
| CRTD | 40 (29.0%) | 28 (34.2%) | 0.690 |
| Dual chamber | 41 (29.7%) | 24 (29.3%) | |
| Single chamber | 57 (41.3%) | 30 (36.6%) | |
Continuous data are summarized as mean (standard deviation), categorical data as counts (%).
VF, ventricular fibrillation; V flutter, ventricular flutter; VT, ventricular tachycardia; NYHA, New York Heart Association; LBB, left bundle branch block; LVEF, left ventricular ejection fraction; LVDD, left ventricular diastolic diameter; ACE inhibitors/ARBII, angiotensin-converting-enzyme inhibitor/angiotensin II receptor blockers; CRTD, cardiac resynchronization therapy defibrillator.
Effects of long-detection interval on appropriate but unnecessary therapies
At least one appropriate ICD therapy was delivered in 169 patients, 105 in the SDI arm and 64 in the LDI arm, 12.7% (95% CI 10.3–15.3) patients/year vs. 7.7% (95% CI 6.0–9.9) patients/year, respectively [IRR: 0.61 (95% CI 0.48–0.78), P < 0.001], indicating a significant reduction in the number of patients experiencing a therapy when LDI was programmed.
Patients in the SDI and LDI arms experienced 208 and 138 episodes appropriately treated with ATPs, respectively, with a significantly lower rate in the LDI arm, 25.1 × 100 patients/year (95% CI 21.8–28.7) in the SDI arm vs. 16.7 × 100 patients/year (95% CI 14.0–19.7) in the LDI arm [IRR: 0.61 (95% CI 0.45–0.83), P = 0.002].
Effects of anti-tachycardia pacing on appropriate but unnecessary therapies
Anti-tachycardia pacing was effective, thus avoiding unnecessary shocks, in 130 out of 208 FVT episodes in the SDI arm and in 72 out of 138 FVT episodes in the LDI arm; consequently, the ATP success rate was 63% in the SDI and 52% in the LDI groups (P = 0.022). The higher ATP efficacy in SDI seemed mainly to involve patients with ischaemic heart disease, 60% (95% CI 47–73%) in SDI vs. 40% (95% CI 28–53%) in LDI, P = 0.040.
In the whole population, successful ATP enabled appropriate but unnecessary shocks to be avoided in 58% of episodes.
The success rate was not different after adjustment for VT cycle (in tertiles 200–270 ms; 271–300 ms; 301–320 ms) (P for interaction = 0.14).
When considering secondary and primary prevention population patients, ATP proved more effective in SDI than in LDI in secondary prevention, 71% (95% CI 51–91%) vs. 45% (95% CI 27–63%), P = 0.042, as expected; by contrast, no difference in ATP efficacy was observed between SDI and LDI in the primary prevention population, 61% (95% CI 49–72%) vs. 49% (95% CI 34–63%), P = 0.214.
Different impact of long-detection interval and anti-tachycardia pacing in reducing appropriate but unnecessary shocks
The ADVANCE III design allowed us to separately analyse the impact of using LDI and ATP in terms of shocks delivered for ventricular episodes. Considering the scenario without the use of both LDI and ATP during charge, 208 episodes would have received at least one shock (SDI arm with shock-only programming). On using only a pure LDI strategy, 138 episodes would have received at least one shock (LDI arm with shock-only programming) (LDI vs. SDI: P = 0.002). Finally, on considering the complete strategy of combining LDI with ATP during charge, only 66 episodes received appropriate and really necessary shocks [LDI + ATP vs. SDI with shock-only IRR: 0.37 (95% CI 0.25–0.53), P < 0.001].
Efficacy of shock therapy
| . | Arm . | Episodes, n (patients, n) . | Success, n (patients, n) . | ATP efficacy (%) . | P-value* . |
|---|---|---|---|---|---|
| ATP or first shock | Standard | 208 (105) | 191 (98) | 92 | 0.716 |
| Long | 138 (64) | 130 (59) | 94 | ||
| ATP | Standard | 208 (105) | 130 (77) | 63 | 0.022 |
| Long | 138 (64) | 72 (36) | 52 | ||
| First shock | Standard | 78 (46) | 61 (37) | 78 | 0.108 |
| Long | 64 (39) | 58 (34) | 91 |
| . | Arm . | Episodes, n (patients, n) . | Success, n (patients, n) . | ATP efficacy (%) . | P-value* . |
|---|---|---|---|---|---|
| ATP or first shock | Standard | 208 (105) | 191 (98) | 92 | 0.716 |
| Long | 138 (64) | 130 (59) | 94 | ||
| ATP | Standard | 208 (105) | 130 (77) | 63 | 0.022 |
| Long | 138 (64) | 72 (36) | 52 | ||
| First shock | Standard | 78 (46) | 61 (37) | 78 | 0.108 |
| Long | 64 (39) | 58 (34) | 91 |
*P-value is GEE adjusted.
| . | Arm . | Episodes, n (patients, n) . | Success, n (patients, n) . | ATP efficacy (%) . | P-value* . |
|---|---|---|---|---|---|
| ATP or first shock | Standard | 208 (105) | 191 (98) | 92 | 0.716 |
| Long | 138 (64) | 130 (59) | 94 | ||
| ATP | Standard | 208 (105) | 130 (77) | 63 | 0.022 |
| Long | 138 (64) | 72 (36) | 52 | ||
| First shock | Standard | 78 (46) | 61 (37) | 78 | 0.108 |
| Long | 64 (39) | 58 (34) | 91 |
| . | Arm . | Episodes, n (patients, n) . | Success, n (patients, n) . | ATP efficacy (%) . | P-value* . |
|---|---|---|---|---|---|
| ATP or first shock | Standard | 208 (105) | 191 (98) | 92 | 0.716 |
| Long | 138 (64) | 130 (59) | 94 | ||
| ATP | Standard | 208 (105) | 130 (77) | 63 | 0.022 |
| Long | 138 (64) | 72 (36) | 52 | ||
| First shock | Standard | 78 (46) | 61 (37) | 78 | 0.108 |
| Long | 64 (39) | 58 (34) | 91 |
*P-value is GEE adjusted.
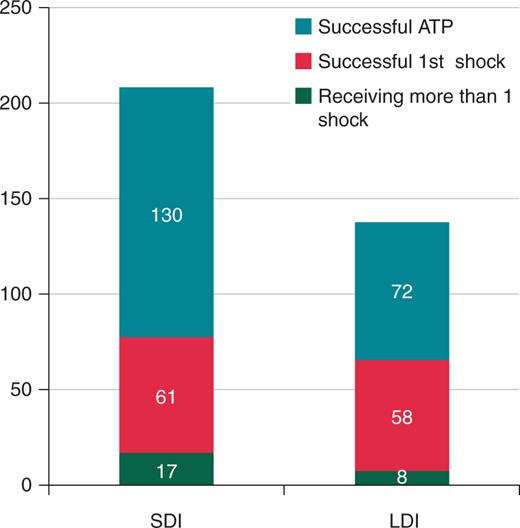
Therapies efficacy. Analysis of the episodes successfully terminated by ATP (turquoise), by the first shock after ATP (red) and by more than one shock after ATP (green). Values are expressed as number of episodes.
Safety of anti-tachycardia pacing
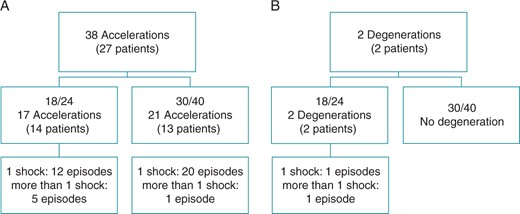
Accelerations (A) and degenerations (B) following ATP. Degenerations are defined as episodes where ATP was delivered inappropriately but the final rhythm was classified as ventricular.
Survival and cardiovascular hospitalization
Freedom from death or cardiovascular hospitalization was analysed in the 220 patients included in this study. No difference was found between the two groups [HR = 1.18 (95% CI 0.68–2.03), P = 0.562].
Discussion
This ADVANCE III sub-study analysis showed that, overall, the use of LDI alone reduced appropriate but unnecessary shocks by 39%; moreover, in >50% of FVT episodes, a single attempt at ATP during capacitor charge converted the arrhythmic episode, thereby avoiding appropriate but unnecessary shocks. Combining ATP during charge with LDI enabled appropriate but unnecessary shocks to be greatly reduced.
The MADIT-RIT trial found a significant reduction in the first occurrence of inappropriate therapy when an high-rate cut-off was programmed. In the light of this finding, it has been hypothesized11 that the main stratagem for achieving optimal programming is simply to use a higher VF cut-off. However, results from the ALTITUDE study showed that there is still a proportion of VFs with CL slower than 200 ms, which may be not treated by means of the high-rate approach. In this setting, the present analysis of the ADVANCE III data showed that combining long detection followed by an ATP attempt and, if necessary, a shock is a safe and effective solution and does not compromise detection rates.
![Different impact of LDI and ATP on appropriate shock reduction: LDI shock only vs. SDI shock only [IRR: 0.61 (95% CI 0.44–0.83), P = 0.002]; and LDI ATP + shock vs. SDI shock only [IRR: 0.37 (95% CI 0.25–0.53), P < 0.001].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/europace/18/11/10.1093_europace_euw032/4/m_euw03203.jpeg?Expires=1748851874&Signature=UstNzJxaiL8H4JZ8ERrZ7-PQFRv8EBvtUMMrCbmrxa41-Gps1dFvP3ViL7pcq-4OkmZH3me0I9KZGEB0aTji8gBM8EsNyOnORjw71rq6mEnsttoZixdvL-70Cs9iBXXPPE3CYnmMkPGr74Yn1DZn9fNVrKCewcWSBjNCCiAcEscdyx68Ha-baqyqCDt~57-rSTAFUac3FVX6f01g94RfASz1Xgrj7RubuvWxK84rXQ~WSjb6u5frIfTHyj2Fn0jbGvFM0D65ZtsLaqVF1WBKKd48tQA-7faJSwWc84R5Rfzv1XBGLg~W6wFlwGFuTUq24dsirfg0Mvf9NFwoczkZLA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Different impact of LDI and ATP on appropriate shock reduction: LDI shock only vs. SDI shock only [IRR: 0.61 (95% CI 0.44–0.83), P = 0.002]; and LDI ATP + shock vs. SDI shock only [IRR: 0.37 (95% CI 0.25–0.53), P < 0.001].
Furthermore, in addition to the already reported reduction in therapies delivered, the overall efficacy of the therapeutic strategy proposed in ADVANCE III (LDI plus ATP during charge) proved to be extremely well powered. Interestingly, the 94% success rate of the ADVANCE III strategy (LDI associated to ATP during charge plus first shock) in converting ventricular episodes is comparable to the reported efficacy of shock delivered as the first therapy.15 Nevertheless, it should be underlined that the efficacy of the LDI strategy should be considered together with the reported significant reduction in the number of ATP therapies and shocks delivered.
Anti-tachycardia pacing efficacy
Several factors have been related to ATP efficacy. A sufficiently long excitable gap is required in order to enable ATP to invade the circuit and terminate a re-entrant VT. Theoretically, the tachycardia CL is the most important factor, since the faster the VT and the shorter the excitable gap, the less likely the ATP will be able to enter the circuit. It has been reported that the CL is the most important predictor of ATP success in spontaneous VTs occurring in ICD patients.17 However, our data do not support this finding, in that we observed no difference in ATP efficacy among different CL ranges. In addition, other studies have shown that the stimulation site18,19 and R–R fluctuations20 may also play a significant role in the ability of ATP to terminate the arrhythmias.
In the ADVANCE III trial, ATP efficacy was lower than that reported for FVT in the Pain FREE I and II studies13,14 and by Jiménez-Candil et al.21 The lower ATP efficacy observed in the ADVANCE III trial could be explained by the differences in patient selection, in that ADVANCE III enrolled a lower proportion of patients with ischaemic heart disease and, more importantly, a markedly greater proportion of primary prevention patients, who are theoretically less predisposed to structured VT amenable to ATP.
Our data support the hypothesis that delivering ATP after short detection leads to overestimation of efficacy. We can speculate that the higher efficacy observed in the SDI arm might be mainly related to the treatment of non-sustained episodes that would not last long enough to be detected in the LDI arm (Supplementary material online, Figures S1 and S2). Accordingly, the 9% difference in efficacy between SDI and LDI did not come as a surprise, bearing in mind that 30% of the episodes in the shock arm of the Pain FREE II trial self-terminated during capacitor charge. However, the causal link between potentially over-treated non-sustained episodes and the higher ATP efficacy in SDI is not clearly established. Further specific investigations are needed in order to clarify this point.
First-shock efficacy
It could be expected that a longer duration of a poorly tolerated FVT could produce some degree of metabolic disturbance, which might increase the defibrillation threshold. However, the present data do not support this suspicion. On the contrary, in our analysis, the first shock proved to be slightly more effective in the LDI group than in the SDI group [91 vs. 78% (P = 0.108)], though statistical significance was not reached. Furthermore, the observed efficacy of shock after unsuccessful initial ATP in the LDI arm proved, nonetheless, to be slightly higher than that recorded in a large cohort of patients who experienced 3677 episodes.15
It should also be noted that LDI reduced the overall number of episodes treated with multiple shocks (Figure 1). While the effect of a single shock is still controversial, patients who suffer multiple shocks have a poor quality of life.22 It is therefore crucial to limit the delivery of repeated high-energy shocks.
Anti-tachycardia pacing safety
Although ATP was less effective after a LDI, it proved consistently safe, as acceleration and VT induction were rare (19 in SDI and 21 in LDI) and similar (P = 0.079) to the rates observed in the standard-detection group. Some concerns about long-detection programming could arise in those patients presenting only sustained episodes, as reduced ATP efficacy may result in a higher rate of necessary appropriate shocks. However, these concerns seem unjustified, since our results show a significant reduction in the number of shocks delivered in the LDI arm. Moreover, death and cardiovascular hospitalizations were similar in the two groups, although it must be acknowledge that the analysis was not powered to detect differences in the clinical outcome.
Limitations
The data presented in this paper refer to a subgroup analysis of the ADVANCE III trial, which randomized patients to two different detection strategies, but not to therapy strategies. Nevertheless, the results obtained by our group are very promising and could be considered as a starting point for the design of an ad hoc trial to further confirm the clinical usefulness of ATP.
Conclusions
In the ADVANCE III trial, an approach combining a long-detection strategy with one ATP attempt during capacitor charge and a backup shock proved to be extremely efficacious and greatly reduced appropriate but unnecessary shocks.
Long-detection interval and ATP play different roles in reducing unnecessary shocks. The use of LDI alone cut appropriate but unnecessary ICD therapy by 39%, while the use of a single ATP attempt on top of LDI avoided the need for painful shocks in >50% of cases, thus confirming the importance of this painless strategy. Anti-tachycardia pacing was confirmed to be safe in terms of VT accelerations, death, or hospitalizations. For the above-mentioned reasons, the combination of ATP during charge with a long-detection window should be considered in the majority of ICD recipients. Further studies are warranted to specifically optimize ATP programming in ICD recipients.
Supplementary material
Supplementary material is available at Europace online.
Funding
The ADVANCE III Study was supported financially by Medtronic, Inc. Minneapolis, MN, USA.
Conflict of interest: A.A., A.P., A.K., M.L., J.B.M.F., A.H., M.G., M.C.E.F.W., and M.G. have received grants from Medtronic, Inc. E.S., L. Manotta, and L. Mangoni are employees of Medtronic, Inc.
Acknowledgements
We thank the study coordinators and the principal investigators at each of the enrolling centres.
References



