-
PDF
- Split View
-
Views
-
Cite
Cite
Roberto Keegan, Luis Aguinaga, Guilherme Fenelon, William Uribe, Gerardo Rodriguez Diez, Mauricio Scanavacca, Manuel Patete, Ricardo Zegarra Carhuaz, Carlos Labadet, Claudio De Zuloaga, Domingo Pozzer, Fernando Scazzuso, on behalf of the SOLAECE registry investigators, The first Latin American Catheter Ablation Registry, EP Europace, Volume 17, Issue 5, May 2015, Pages 794–800, https://doi.org/10.1093/europace/euu322
Close - Share Icon Share
Abstract
To assess the results of transcatheter ablation of cardiac arrhythmias in Latin America and establish the first Latin American transcatheter ablation registry.
All ablation procedures performed between 1 January and 31 December 2012 were analysed retrospectively. Data were obtained on the characteristics and resources of participating centres (public or private institution, number of beds, cardiac surgery availability, type of room for the procedures, days per week assigned to electrophysiology procedures, type of fluoroscopy equipment, availability and type of electroanatomical mapping system, intracardiac echo, cryoablation, and number of electrophysiologists) and the results of 17 different ablation substrates: atrio-ventricular node reentrant tachycardia, typical atrial flutter, atypical atrial flutter, left free wall accessory pathway, right free wall accessory pathway, septal accessory pathway, right-sided focal atrial tachycardia, left-sided focal atrial tachycardia, paroxysmal atrial fibrillation, non-paroxysmal atrial fibrillation, atrio-ventricular node, premature ventricular complex, idiopathic ventricular tachycardia, post-myocardial infarction ventricular tachycardia, ventricular tachycardia in chronic chagasic cardiomyopathy, ventricular tachycardia in congenital heart disease, and ventricular tachycardias in other structural heart diseases. Data of 15 099 procedures were received from 120 centres in 13 participating countries (Argentina, Bolivia, Brazil, Chile, Colombia, Cuba, El Salvador, Guatemala, Mexico, Peru, Dominican Republic, Uruguay, and Venezuela). Accessory pathway was the group of arrhythmias most frequently ablated (31%), followed by atrio-ventricular node reentrant tachycardia (29%), typical atrial flutter (14%), and atrial fibrillation (11%). Overall success was 92% with the rate of global complications at 4% and mortality 0.05%.
Catheter ablation in Latin America can be considered effective and safe.
This is the first information of catheter ablation in Latin America as a result of a multicentre registry including a large number of procedures.
Efficacy and safety are considered similar to other places worldwide.
According to the results, ventricular tachycardia ablation in chagasic patients could be considered a challenging procedure.
Introduction
Transcatheter ablation of cardiac arrhythmias was successfully introduced into daily clinical practice over 30 years ago.1,2 Since then, surveys and multicentre registries have mainly been reported from centres across the Europe and the USA,3–5 whereas in Latin America registries are limited to a few countries.6,7 Therefore, the Latin American Society of Electrophysiology and Cardiac Stimulation (SOLAECE) decided to compile the first Catheter Ablation Registry in Latin America.
Methods
The registry was designed to retrospectively analyse all ablations, either first-time or re-do procedures, performed between 1 January and 31 December 2012. Voluntary invitations to all local representatives were issued by SOLAECE through the scientific electrophysiology (EP) societies to complete an online form related to the centre resources and all transcatheter ablation procedures conducted. Data collected covered the centres' resources, different ablation substrates, and the success and complication rates of procedures. Every participating investigator had to be affiliated to any scientific EP society and to sign up an agreement of reliability and confidentiality before data entering.
Centre-related information: Public or private institution, number of beds, cardiac surgery availability, type of room for the procedures [EP laboratory, catheterization (Cath) laboratory, or operating room], days per week assigned to EP procedures, type of fluoroscopy equipment, availability and type of electroanatomical mapping system (Carto®, EnSite®, or both), intracardiac echo, cryoablation, and number of electrophysiologists.
Seventeen ablation substrates were analysd: Atrio-ventricular node reentrant tachycardia (AVNRT), typical atrial flutter (AF), atypical AF, left free wall accessory pathway (left AP), right free wall accessory pathway (right AP), septal accessory pathway (septal AP), right-sided focal atrial tachycardia (right AT), left-sided focal atrial tachycardia (left AT), paroxysmal atrial fibrillation (PAF), non-PAF, atrio-ventricular node (AVN), premature ventricular complex (PVC), idiopathic ventricular tachycardia (VT), post-myocardial infarction ventricular tachycardia (MIVT), ventricular tachycardia in chronic chagasic cardiomyopathy (Chagas VT), ventricular tachycardia in congenital heart disease (congenital VT), and ventricular tachycardias in other structural heart diseases (cardiopathy VT).
Outcomes of the procedures: These included total number of patients and procedures, success of the procedures, type of catheter used (4 mm, 8 mm, or irrigated tip), procedures with radiofrequency as the power source, cryoablation, fluoroscopy, and electroanatomical mapping, type of anaesthesia (local, conscious sedation, and general), and patients with at least one complication during hospitalization. Additionally, the results included specific details of the complications that arose as a result of treatment: hematoma, arteriovenous fistula, thrombosis and thrombophlebitis, pneumothorax, pleural effusion, atrio-ventricular block with and without pacemaker implantation, pericarditis, pericardial effusion, cardiac tamponade, myocardial infarction/ischaemia, congestive heart failure /acute pulmonary edema, transient ischaemic attack, stroke, peripheral embolism, death, or other complications.
Success was determined at the end of the procedure. The definitions of success had been consented for substrates such as AVNRT, typical and atypical AF, right AP, left AP, septal AP, right AT, left AT, AVN, and idiopathic VT. Success criteria for more complex substrates were defined as follows: isolation of all pulmonary veins for PAF; isolation of pulmonary veins plus achievement of additional end points (i.e. additional lines, complex fractionated atrial electrogram mapping) for non-PAF and absence of culprit ventricular complexes 30 min after ablation for PVCs. Post-MIVT, Chagas VT, congenital VT, and cardiopathy VT ablation procedures were considered successful if all the monomorphic VTs induced at the baseline became non-inducible post-ablation.
Results were expressed as average, ranges, and percentages.
Results
Data were received from 120 centres located in Argentina, Bolivia, Brazil, Chile, Colombia, Cuba, El Salvador, Guatemala, Mexico, Peru, Dominican Republic, Uruguay, and Venezuela. The total population of these 13 countries represents 90% of the population of Latin America. The average population per centre across the 13 participating countries was 8 053 176 habitants (656 349 in Argentina and 16 841 000 in Colombia). The distribution of the participating centres by country was as follows: 52% from Argentina, 18% from Brazil, 12% from Mexico, and 18% from the remaining countries. However, 79% of the procedures were referred by two countries: Brazil (45%) and Argentina (34%). Forty-three centres (36%) performed over 100 procedures in the 1 year period, 24 centres (20%) performed between 50 and 100, and 53 centres (44%) performed fewer than 50 procedures. Table 1 shows the number of the centres that performed ablations in the 17 categories of ablation substrate (Figure 1).
Number of centres participating in the Latin American Registry that performed ablations in the 17 substrates analysed
| Substrate . | Centres . |
|---|---|
| Atrio-ventricular nodal reentrant tachycardia | 116 (97%) |
| Typical Atrial flutter | 105 (88%) |
| Atypical Atrial flutter | 56 (47%) |
| Left Accessory Pathways | 113 (94%) |
| Right Accessory Pathways | 83 (69%) |
| Septal Accessory Pathways | 102 (85%) |
| Right Focal atrial tachycardia | 77 (64%) |
| Left Focal atrial tachycardia | 43 (36%) |
| Paroxysmal atrial fibrillation | 56 (47%) |
| Not paroxysmal atrial fibrillation | 38 (32%) |
| Atrioventricular node ablation | 75 (63%) |
| Premature ventricular complexes | 70 (58%) |
| Idiopathic VT | 80 (67%) |
| Post-myocardial infarction ventricular tachycardia | 42 (35%) |
| Ventricular tachycardia in Chagas disease | 22 (18%) |
| Congenital VT | 7 (6%) |
| Cardiopathy VT | 21 (18%) |
| Substrate . | Centres . |
|---|---|
| Atrio-ventricular nodal reentrant tachycardia | 116 (97%) |
| Typical Atrial flutter | 105 (88%) |
| Atypical Atrial flutter | 56 (47%) |
| Left Accessory Pathways | 113 (94%) |
| Right Accessory Pathways | 83 (69%) |
| Septal Accessory Pathways | 102 (85%) |
| Right Focal atrial tachycardia | 77 (64%) |
| Left Focal atrial tachycardia | 43 (36%) |
| Paroxysmal atrial fibrillation | 56 (47%) |
| Not paroxysmal atrial fibrillation | 38 (32%) |
| Atrioventricular node ablation | 75 (63%) |
| Premature ventricular complexes | 70 (58%) |
| Idiopathic VT | 80 (67%) |
| Post-myocardial infarction ventricular tachycardia | 42 (35%) |
| Ventricular tachycardia in Chagas disease | 22 (18%) |
| Congenital VT | 7 (6%) |
| Cardiopathy VT | 21 (18%) |
Number of centres participating in the Latin American Registry that performed ablations in the 17 substrates analysed
| Substrate . | Centres . |
|---|---|
| Atrio-ventricular nodal reentrant tachycardia | 116 (97%) |
| Typical Atrial flutter | 105 (88%) |
| Atypical Atrial flutter | 56 (47%) |
| Left Accessory Pathways | 113 (94%) |
| Right Accessory Pathways | 83 (69%) |
| Septal Accessory Pathways | 102 (85%) |
| Right Focal atrial tachycardia | 77 (64%) |
| Left Focal atrial tachycardia | 43 (36%) |
| Paroxysmal atrial fibrillation | 56 (47%) |
| Not paroxysmal atrial fibrillation | 38 (32%) |
| Atrioventricular node ablation | 75 (63%) |
| Premature ventricular complexes | 70 (58%) |
| Idiopathic VT | 80 (67%) |
| Post-myocardial infarction ventricular tachycardia | 42 (35%) |
| Ventricular tachycardia in Chagas disease | 22 (18%) |
| Congenital VT | 7 (6%) |
| Cardiopathy VT | 21 (18%) |
| Substrate . | Centres . |
|---|---|
| Atrio-ventricular nodal reentrant tachycardia | 116 (97%) |
| Typical Atrial flutter | 105 (88%) |
| Atypical Atrial flutter | 56 (47%) |
| Left Accessory Pathways | 113 (94%) |
| Right Accessory Pathways | 83 (69%) |
| Septal Accessory Pathways | 102 (85%) |
| Right Focal atrial tachycardia | 77 (64%) |
| Left Focal atrial tachycardia | 43 (36%) |
| Paroxysmal atrial fibrillation | 56 (47%) |
| Not paroxysmal atrial fibrillation | 38 (32%) |
| Atrioventricular node ablation | 75 (63%) |
| Premature ventricular complexes | 70 (58%) |
| Idiopathic VT | 80 (67%) |
| Post-myocardial infarction ventricular tachycardia | 42 (35%) |
| Ventricular tachycardia in Chagas disease | 22 (18%) |
| Congenital VT | 7 (6%) |
| Cardiopathy VT | 21 (18%) |
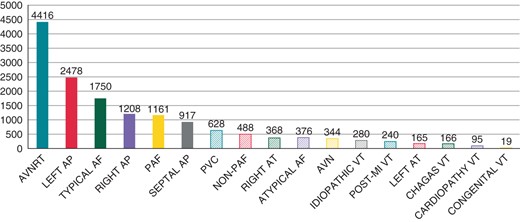
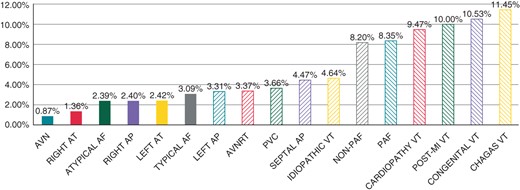
Total number of procedures conducted for each substrate in the participating centres in the Latin American Registry.
Centre-related information
Of the participating centres, 63% were private, whereas 25% were public and 12% academic (university hospitals), with average beds per centre of 235 (10–1000). Cardiac surgery was available in 109 centres (91%). An EP laboratory was available in 72 centres (60%), with the remaining 48 (40%) centres performing the procedures in Cath laboratories or operating rooms. On average, 2.81–4 EP procedures were conducted each week.
Fluoroscopy was provided by an angiographer in 67 centres (56%) while a C-arch with rotating anode was used in 40 (33%) centres and a C-arch with a fixed anode in only 4 (3%) centres. Information about the type of fluoroscopy equipment was not provided by nine of the centres (8%).
Fifty-nine centre (49%) had electroanatomical mapping available including 16 with Carto® mapping, 34 with EnSite®, and 9 with both, whereas 24 centres (20%) had intracardiac echocardiography (5 from Argentina, 5 from Mexico, 4 from Brazil, 3 from Uruguay, 3 from Venezuela, 2 from Colombia, 1 from Peru, and 1 from El Salvador). Only four centres (3%) were equipped with cryoablation facilities (three from Argentina and one from Mexico).
Sixty centres (50%) had a fellowship programme as part of their working structure and organization.
Ablation substrates and resources
Atrio-ventricular node reentrant tachycardia was the most frequently treated substrate. However, after substrate grouping, accessory pathways were the most frequently performed procedure (31%), followed by AVNRT (29%), typical AF (14%), and atrial fibrillation (11%). These four ablation substrate groups represented 85% of the procedures overall, whereas ventricular arrhythmias represented less than 10% of the referred ablations (Figures 2 and 3).
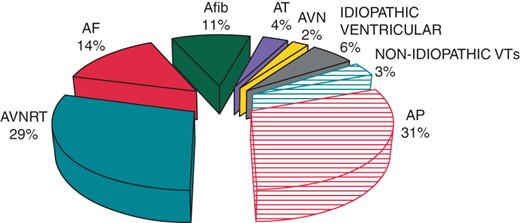
Grouped substrates. AP, accessory pathways; AVNRT, atrio-ventricular nodal reentrant tachycardia; AF, atrial flutter; Afib, atrial fibrillation; AT, focal atrial tachycardia; AVN, atrio-ventricular node.
Atrial fibrillation ablation was performed in 63 centres (52%) and the average annual number of procedures per centre was 26. Only five centres performed 100 or more procedures. Most of the centres ablated PAF and non-PAF while 15 centres only treated paroxysmal AF.
The 4 mm tip was the most commonly used ablation catheter (66%). The irrigated tip was used in 20% of the procedures, with the 8 mm ablation catheter counting for the remaining 14%. Radiofrequency was the predominant power source used, since cryoablation was chosen in only 25 procedures (0.17%). Electroanatomical mapping was used in 20% of the cases.
Local anaesthesia and conscious sedation were used most frequently, with only 18% of the patients undergoing general anaesthesia.
Ablation results
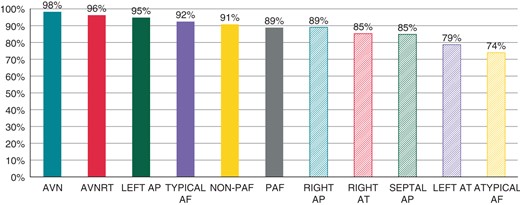
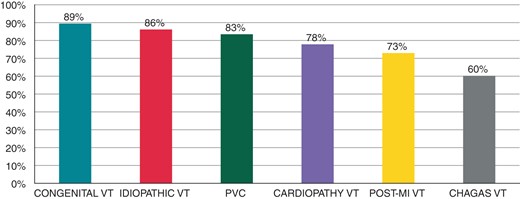
The total number of procedures included in the analysis was 15 099 and the total number of patients 14.349. Thus, 750 of procedures (5%) were performed by arrhythmia recurrence and/or unsuccessful previous ablation. Overall success was achieved in 92% of the procedures (13 838). The success rate per substrate is shown in Figures 4 and 5. The complication rate among all procedures was 4%. Figures 6 and 7 show complication rates per substrate and the prevalence of different complications. Table 2 summarizes the number of procedures and outcomes of different substrates in each country.
| Country . | Centres . | Procedures . | Average per centre per year . | AP . | AVNRT . | AFL . | AF . | AT . | AVN . | IVA . | Chagas VT . | Post-MIVT . | VT other . | Success (%) . | Complications (%) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | 18 | 6853 | 381 | 2203 | 2180 | 731 | 742 | 173 | 97 | 410 | 125 | 146 | 46 | 89 | 4 |
| Argentina | 63 | 5071 | 80 | 1375 | 1443 | 946 | 613 | 237 | 96 | 258 | 32 | 55 | 16 | 92 | 4 |
| Venezuela | 4 | 807 | 202 | 167 | 232 | 87 | 124 | 38 | 25 | 93 | 5 | 22 | 14 | 92 | 6 |
| Mexico | 12 | 806 | 67 | 262 | 202 | 116 | 68 | 34 | 67 | 45 | 0 | 9 | 3 | 95 | 3 |
| Colombia | 3 | 425 | 142 | 66 | 95 | 88 | 72 | 9 | 24 | 38 | 4 | 0 | 29 | 97 | 4 |
| Cuba | 2 | 356 | 178 | 204 | 97 | 29 | 0 | 9 | 9 | 8 | 0 | 0 | 0 | 90 | 1 |
| Uruguay | 4 | 300 | 75 | 81 | 85 | 59 | 13 | 17 | 14 | 22 | 0 | 3 | 6 | 91 | 3 |
| Peru | 4 | 259 | 65 | 159 | 30 | 40 | 0 | 4 | 7 | 19 | 0 | 0 | 0 | 90 | 5 |
| Chile | 1 | 71 | 71 | 10 | 10 | 18 | 17 | 6 | 2 | 4 | 0 | 4 | 0 | 96 | 0 |
| Dominican Republic | 5 | 65 | 13 | 28 | 21 | 5 | 0 | 3 | 1 | 7 | 0 | 0 | 0 | 95 | 0 |
| Guatemala | 1 | 37 | 37 | 31 | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 86 | 3 |
| El Salvador | 1 | 32 | 32 | 13 | 9 | 3 | 0 | 1 | 1 | 4 | 0 | 1 | 0 | 84 | 13 |
| Bolivia | 2 | 17 | 9 | 4 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 | 0 |
| Country . | Centres . | Procedures . | Average per centre per year . | AP . | AVNRT . | AFL . | AF . | AT . | AVN . | IVA . | Chagas VT . | Post-MIVT . | VT other . | Success (%) . | Complications (%) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | 18 | 6853 | 381 | 2203 | 2180 | 731 | 742 | 173 | 97 | 410 | 125 | 146 | 46 | 89 | 4 |
| Argentina | 63 | 5071 | 80 | 1375 | 1443 | 946 | 613 | 237 | 96 | 258 | 32 | 55 | 16 | 92 | 4 |
| Venezuela | 4 | 807 | 202 | 167 | 232 | 87 | 124 | 38 | 25 | 93 | 5 | 22 | 14 | 92 | 6 |
| Mexico | 12 | 806 | 67 | 262 | 202 | 116 | 68 | 34 | 67 | 45 | 0 | 9 | 3 | 95 | 3 |
| Colombia | 3 | 425 | 142 | 66 | 95 | 88 | 72 | 9 | 24 | 38 | 4 | 0 | 29 | 97 | 4 |
| Cuba | 2 | 356 | 178 | 204 | 97 | 29 | 0 | 9 | 9 | 8 | 0 | 0 | 0 | 90 | 1 |
| Uruguay | 4 | 300 | 75 | 81 | 85 | 59 | 13 | 17 | 14 | 22 | 0 | 3 | 6 | 91 | 3 |
| Peru | 4 | 259 | 65 | 159 | 30 | 40 | 0 | 4 | 7 | 19 | 0 | 0 | 0 | 90 | 5 |
| Chile | 1 | 71 | 71 | 10 | 10 | 18 | 17 | 6 | 2 | 4 | 0 | 4 | 0 | 96 | 0 |
| Dominican Republic | 5 | 65 | 13 | 28 | 21 | 5 | 0 | 3 | 1 | 7 | 0 | 0 | 0 | 95 | 0 |
| Guatemala | 1 | 37 | 37 | 31 | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 86 | 3 |
| El Salvador | 1 | 32 | 32 | 13 | 9 | 3 | 0 | 1 | 1 | 4 | 0 | 1 | 0 | 84 | 13 |
| Bolivia | 2 | 17 | 9 | 4 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 | 0 |
AP, accessory pathways; AVNRT, atrio-ventricular nodal reentrant tachycardia; AFL, atrial flutter; AF, atrial fibrillation; AT, focal atrial tachycardia; AVN, atrioventricular node ablation; IVA, idiopathic ventricular arrhythmias; Chagas VT, ventricular tachycardia in chronic chagasic cardiomyopathy; post-MIVT, post-myocardial infarction ventricular tachycardia; VT other, ventricular tachycardia in congenital and other structural heart disease.
| Country . | Centres . | Procedures . | Average per centre per year . | AP . | AVNRT . | AFL . | AF . | AT . | AVN . | IVA . | Chagas VT . | Post-MIVT . | VT other . | Success (%) . | Complications (%) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | 18 | 6853 | 381 | 2203 | 2180 | 731 | 742 | 173 | 97 | 410 | 125 | 146 | 46 | 89 | 4 |
| Argentina | 63 | 5071 | 80 | 1375 | 1443 | 946 | 613 | 237 | 96 | 258 | 32 | 55 | 16 | 92 | 4 |
| Venezuela | 4 | 807 | 202 | 167 | 232 | 87 | 124 | 38 | 25 | 93 | 5 | 22 | 14 | 92 | 6 |
| Mexico | 12 | 806 | 67 | 262 | 202 | 116 | 68 | 34 | 67 | 45 | 0 | 9 | 3 | 95 | 3 |
| Colombia | 3 | 425 | 142 | 66 | 95 | 88 | 72 | 9 | 24 | 38 | 4 | 0 | 29 | 97 | 4 |
| Cuba | 2 | 356 | 178 | 204 | 97 | 29 | 0 | 9 | 9 | 8 | 0 | 0 | 0 | 90 | 1 |
| Uruguay | 4 | 300 | 75 | 81 | 85 | 59 | 13 | 17 | 14 | 22 | 0 | 3 | 6 | 91 | 3 |
| Peru | 4 | 259 | 65 | 159 | 30 | 40 | 0 | 4 | 7 | 19 | 0 | 0 | 0 | 90 | 5 |
| Chile | 1 | 71 | 71 | 10 | 10 | 18 | 17 | 6 | 2 | 4 | 0 | 4 | 0 | 96 | 0 |
| Dominican Republic | 5 | 65 | 13 | 28 | 21 | 5 | 0 | 3 | 1 | 7 | 0 | 0 | 0 | 95 | 0 |
| Guatemala | 1 | 37 | 37 | 31 | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 86 | 3 |
| El Salvador | 1 | 32 | 32 | 13 | 9 | 3 | 0 | 1 | 1 | 4 | 0 | 1 | 0 | 84 | 13 |
| Bolivia | 2 | 17 | 9 | 4 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 | 0 |
| Country . | Centres . | Procedures . | Average per centre per year . | AP . | AVNRT . | AFL . | AF . | AT . | AVN . | IVA . | Chagas VT . | Post-MIVT . | VT other . | Success (%) . | Complications (%) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | 18 | 6853 | 381 | 2203 | 2180 | 731 | 742 | 173 | 97 | 410 | 125 | 146 | 46 | 89 | 4 |
| Argentina | 63 | 5071 | 80 | 1375 | 1443 | 946 | 613 | 237 | 96 | 258 | 32 | 55 | 16 | 92 | 4 |
| Venezuela | 4 | 807 | 202 | 167 | 232 | 87 | 124 | 38 | 25 | 93 | 5 | 22 | 14 | 92 | 6 |
| Mexico | 12 | 806 | 67 | 262 | 202 | 116 | 68 | 34 | 67 | 45 | 0 | 9 | 3 | 95 | 3 |
| Colombia | 3 | 425 | 142 | 66 | 95 | 88 | 72 | 9 | 24 | 38 | 4 | 0 | 29 | 97 | 4 |
| Cuba | 2 | 356 | 178 | 204 | 97 | 29 | 0 | 9 | 9 | 8 | 0 | 0 | 0 | 90 | 1 |
| Uruguay | 4 | 300 | 75 | 81 | 85 | 59 | 13 | 17 | 14 | 22 | 0 | 3 | 6 | 91 | 3 |
| Peru | 4 | 259 | 65 | 159 | 30 | 40 | 0 | 4 | 7 | 19 | 0 | 0 | 0 | 90 | 5 |
| Chile | 1 | 71 | 71 | 10 | 10 | 18 | 17 | 6 | 2 | 4 | 0 | 4 | 0 | 96 | 0 |
| Dominican Republic | 5 | 65 | 13 | 28 | 21 | 5 | 0 | 3 | 1 | 7 | 0 | 0 | 0 | 95 | 0 |
| Guatemala | 1 | 37 | 37 | 31 | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 86 | 3 |
| El Salvador | 1 | 32 | 32 | 13 | 9 | 3 | 0 | 1 | 1 | 4 | 0 | 1 | 0 | 84 | 13 |
| Bolivia | 2 | 17 | 9 | 4 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 | 0 |
AP, accessory pathways; AVNRT, atrio-ventricular nodal reentrant tachycardia; AFL, atrial flutter; AF, atrial fibrillation; AT, focal atrial tachycardia; AVN, atrioventricular node ablation; IVA, idiopathic ventricular arrhythmias; Chagas VT, ventricular tachycardia in chronic chagasic cardiomyopathy; post-MIVT, post-myocardial infarction ventricular tachycardia; VT other, ventricular tachycardia in congenital and other structural heart disease.
Per substrate complications in the 17 ablation substrates analysed.
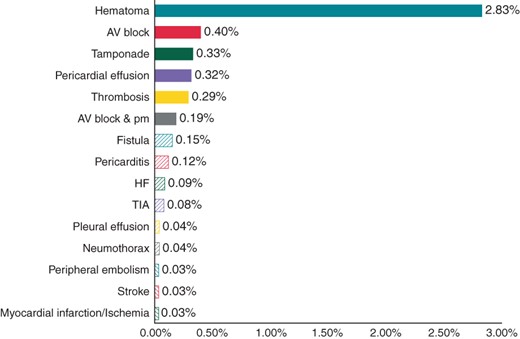
Prevalence of the different complications recorded from all of the 17 ablation substrates analysed.
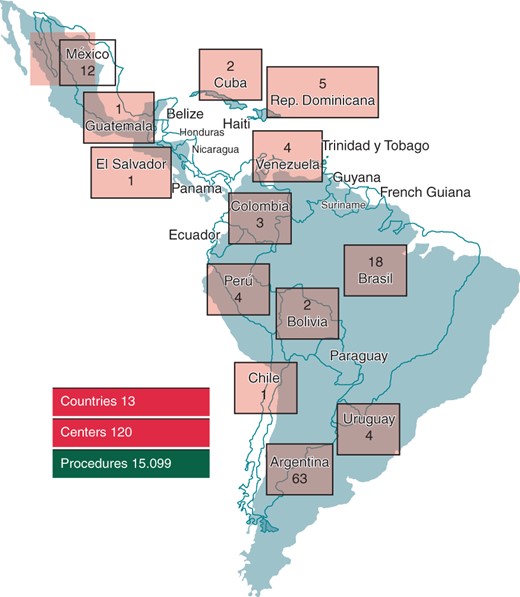
(Representative figure): First Latin American Catheter Ablation Registry: countries, centres, and procedures.
Eight procedure-related deaths were reported (0.05%): three of them occurred during a Chagas VT ablation (1.81%), two during an AVN ablation (0.58%), one during a PAF procedure (0.09%), one during a right free wall AP (0.08%), and the other one during AVNRT ablation (0.02%). Substrate grouping revealed a mortality rate of 0.58% for VT when structural heart disease was present and of 0.58% for AVN ablation, 0.06% for atrial fibrillation ablation, and 0.02% for AP and AVNRT ablations. The complications related to mortality were pulmonary embolism (right AP endocardial/epicardial ablation in a patient with Ebstein anomaly, and AVN ablation), tamponade (AVNRT and Chagas VT), tamponade associated to severe aortic valvular insufficiency (Chagas VT), and unknown in three cases (PAF ablation, AVN ablation, and Chagas VT ablation).
Discussion
Even though almost 80% of the procedures came from two countries (Brazil and Argentina), the first Latin American multicentre retrospective catheter ablation registry can be considered representative of transcatheter ablation procedures in Latin American as the population of the 13 countries participating accounted for the majority of the population living in this region of the world.
When the centre-related information was analysed, we observed some limitations regarding infrastructure and technology resources. Less than 50% of the centres had a dedicated EP laboratory or an electroanatomical mapping system. This could be related to the economic situation in Latin America, as the majority of countries are developing countries.
Even though the distribution of the ablated arrhythmias is similar to other registries with the majority of ablations performed for AVRT, accessory pathways, and atrial flutter, based on the number of the centres that performed more complex ablations, such as atrial fibrillation and VT with structural heart diseases, it is possible that these procedures are underused for treating these types of arrhythmias.
The global success rate was lower and the complication rate higher than other registries.5 However, in the analysis of procedure success rates, atrial fibrillation and post-MIVT data were included in the Latin American Registry, but not in the comparison registries. In the Latin American Registry, haematoma accounted for more than 50% of the complications reported in all 17 substrates, irrespective of whether treatment was required. In the other registries, only haematomas that required treatment such as blood transfusion and/or surgical intervention were included. The success rate in simpler ablations was similar. On the other hand, the rate of complications in atrial fibrillation ablation was higher than expected8 but similar to the European AFib ablation registry published recently.9,10 This finding could be associated with the low numbers of procedures performed yearly for this arrhythmia.
Finally, it is important to mention that this is the first registry that analysed VT ablation in Chagas disease. Even though Chagas disease is endemic in many countries in Latin America, globalization and migration have increased the likelihood of treatment of patients with VT as a direct result of Chagas disease elsewhere in the world. Consequently, the data on VT ablation in Chagas disease could provide important information regarding the performance of this challenging ablation. As reported here, this arrhythmia had the lowest success rate and the highest rate of complications. This could be related to the complexity of the arrhythmia itself, the complexity of the procedure (an epicardial access is frequently required), and the frequently poor clinical condition of the patients at the time of the procedure, as in many cases incessant VT and electrical storm is the indication for ablation.
Limitations
Owing to lack of information of total number of centres performing catheter ablation in Latin America, the participation degree of the centres as a representative sample is missing.
No auditing procedure was established to assess the reliability of collected data and outcomes of ablations.
According to the registry design no prospective data such as recurrence of arrhythmias after the procedure or complication rate beyond discharge the patient were available.
Conclusions
Catheter ablation in Latin America can be considered effective and safe. However, it may be underutilized, especially for more complex arrhythmias. Perhaps with improvements to infrastructure and more technical resources greater numbers of patients would gain access to ablation facilities in Latin America and improve the overall results.
Supplementary material
Supplementary material is available at Europace online.
Conflict of interest: none declared.
References
Author notes
Name of investigators and centres are reported in online Appendix.
- cardiac arrhythmia
- atrial fibrillation
- tachycardia
- atrial flutter
- premature ventricular contractions
- tachycardia, ventricular
- atrioventricular accessory pathway
- atrial tachycardia
- atrioventricular node
- cardiomyopathy
- cardiac ablation
- cardiac surgery procedures
- heart diseases
- congenital heart disease
- argentina
- beds
- bolivia
- brazil
- chile
- colombia
- cryosurgery
- cuba
- dominican republic
- el salvador
- electrophysiology
- fluoroscopy
- guatemala
- latin america
- mexico
- peru
- uruguay
- venezuela
- mortality
- paroxysmal atrial fibrillation
- accelerated atrioventricular conduction
- post myocardial infarction
- ablation
- intracardiac echocardiography



