-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel Cismaru, Radu Rosu, Lucian Muresan, Mihai Puiu, Marius Andronache, Erika Hengan, Daniel Ispas, Gabriel Gusetu, Dana Pop, Petru Adrian Mircea, Dumitru Zdrenghea, The value of adrenaline in the induction of supraventricular tachycardia in the electrophysiological laboratory, EP Europace, Volume 16, Issue 11, November 2014, Pages 1634–1638, https://doi.org/10.1093/europace/euu042
Close - Share Icon Share
Abstract
The most commonly used drug for the facilitation of supraventricular tachycardia (SVT) induction in the electrophysiological (EP) laboratory is isoprenaline. Despite isoprenaline's apparent indispensability, availability has been problematic in some European countries. Alternative sympatomimethic drugs such as adrenaline have therefore been tried. However, no studies have determined the sensitivity and specificity of adrenaline for the induction of SVT. The objective of this study was to determine the sensitivity and specificity of adrenaline for the induction of SVT.
Between February 2010 and July 2013, 336 patients underwent an EP study for prior documented SVT. In 66 patients, adrenaline was infused because tachycardia was not induced under basal conditions. This group was compared with 30 control subjects with no history of SVT. Programmed atrial stimulation was carried out during baseline state and repeated after an infusion of adrenaline (dose ranging from 0.05 mcg/kgc to 0.3 mcg/kgc). The endpoint was the induction of SVT. Among 66 patients with a history of SVT but no induction under basal conditions, adrenaline facilitated induction in 54 patients (82%, P < 0.001). Among the 30 control subjects, SVT was not induced in any patient (0%) after infusion. Adrenaline was generally well tolerated, except for two patients (3.0%), where it had to be discontinued due to headache and high blood pressure or lumbar pain.
Adrenaline infusion has a high sensitivity (82%) and specificity (100%) for the induction of SVT in patients with prior documented SVT. Therefore, it could serve as an acceptable alternative to isoprenaline, when the latter is not available.
Adrenaline can be used for the induction of SVT in patients with paroxysmal documented SVT.
It may also be considered in patients who undergo an electrophysiological study to determine the mechanism of their palpitations and/or syncope, if no documentation of arrhythmia exists (12-lead electrocardiogram), after having undergone a complete negative set of noninvasive tests.
Because adrenaline cannot always facilitate the induction of SVT in patients with a history of paroxysmal SVT even at infusion rates of 0.3 μg/kg/min, it is important to be aware of the fact that the addition of other drugs such as atropine or isoprenaline might be necessary to induce and assess the mechanism of SVT before catheter ablation.
Introduction
Isoprenaline, a beta-adrenergic drug, commonly used in clinical practice for its properties of increasing heart rate can induce supraventricular tachycardia (SVT) in the electrophysiology (EP) laboratory.1,2 Despite its apparent indispensability, availability has been problematic in Eastern Europe. Alternative sympatomimethic drugs like adrenaline have therefore been tried.
The sensitivity and specificity of isoprenaline for the induction of paroxysmal atrial fibrillation have already been reported.3 Although adrenaline is known to facilitate the induction of SVT, its sensitivity and specificity in the EP laboratory have not previously been evaluated.
The purpose of this study was to determine the sensitivity and specificity of adrenaline for the induction of SVT during the electrophysiological (EP) study.
Methods
Study subjects
From February 2010 to July 2013, a total of 336 patients with clinically documented paroxysmal SVT (PSVT) were referred to our department for an EP study ± radiofrequency catheter ablation procedure. Sixty-six patients necessitated adrenaline infusion because under basal conditions no PSVT was induced. Twenty-four patients were men (36.4%) and 42 women, with a mean age of 49.2 years. Patients with known coronary artery disease, hypertrophic obstructive cardiomyopathy, severe aortic or mitral valve stenosis were excluded from the study. All patients had recurrent episodes of PSVT documented by 12-lead electrocardiogram (ECG).
A group of 30 subjects with no history of tachycardia constituted the control group. The EP study was performed in these patients for the following reasons: to assess the sinus node function and atrioventricular (AV) conduction in 10 patients, to investigate the cause of syncope in 8 patients, to determine the refractory period of an accessory pathway in 7 patients and prior to ventricular extrasystole ablation in 6 patients. Adrenaline was infused in all and a complete EP study was conducted.
Electrophysiological study
The EP study was performed in non-sedated patients in the post-absorptive state after an informed consent was obtained. All patients were in sinus rhythm at the beginning of the study.
Heart catheterization was performed through the right femoral vein with four multielectrode catheters. Electrograms were recorded from the high right atrium, the bundle of His, coronary sinus, and the right ventricle.
Atrial and ventricular programmed stimulation as well as overdrive pacing was conducted, to determine the conduction properties and refractoriness of the AV node, to exclude the presence of an accessory pathway, to induce and to stop SVTs, and to perform the differential diagnosis of PSVT.
Our atrial programmed stimulation protocol employed delivery of up to three atrial extrastimuli at two atrial sites and at two atrial drive pacing lengths (600 and 400 ms).
If no arrhythmia was induced at the basal state, adrenaline was consecutively administered. Infusion was started at 0.05 μg/kg/min and up-titrated until an increase in the basal heart rate by at least 50% was noticed, to at least 100 beats/min (maximum 150 beats/min or 400 ms of cycle). The amount of adrenaline required to induce the desired changes in heart rate ranged from 0.1 to 0.3 μg/kg/min. Attempts to induce SVT by atrial and ventricular programmed stimulation and overdrive pacing were repeated during adrenaline infusion. For patients in which adrenaline infusion was not sufficient for SVT induction, atropine 1 to 2 mg iv was administrated.
Statistical analysis
Statistical analysis was performed using the SPSS Statistics version 21.0 (SPSS, Inc.). Descriptive statistics were used to summarize patient characteristics. Means and standard deviations were used for normally distributed continuous variables as well as counts and proportions for categorical variables. The McNemar test for related samples was performed to compare in a pairwise fashion the fraction of patients with inducible PSVT before and after adrenaline infusion.
Results
In 115 out of 336 patients (34.2%), there was no need for drug provocation: 50 patients (44%) with AV node re-entry tachycardia (AVNRT), 44 patients (38%) with AV re-entry tachycardia (AVRT) conducted retrogradely through an accessory pathway, and 21 (18%) with atrial tachycardia (AT).
In 221 out of 336 patients (65.8%) without induction in the basal state, we used medication for SVT induction. For patients included in our study from February 2010 to July 2012, we used atropine and isoprenaline (isoprenaline was available in our EP laboratory during this period of time). For patients included in our study from July 2012 to July 2013, we used atropine and adrenaline (because isoprenaline was not available in our EP laboratory during this period of time).
Concerning the use of adrenaline or atropine, the choice of one drug or the other as the initial medication for facilitating the induction of SVT was left to the physician's free will. Consequently, one doctor used adrenaline first for SVT induction and another doctor used atropine first for SVT induction. If no SVT was induced after the administration of the first drug, then the other drug was added (Figure 1).
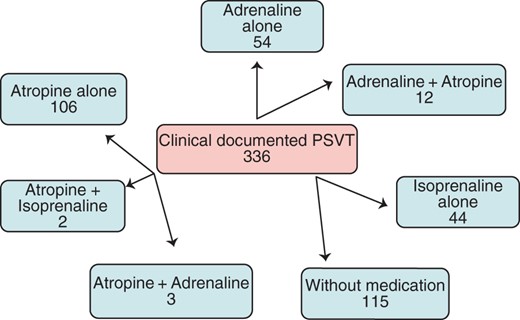
The population included in the study and the distribution of drugs used for SVT induction. PSVT, paroxysmal supraventricular tachycardia. Adrenaline + atropine indicates that tachycardia was not induced after the administration of adrenaline alone, so atropine was administered on top to facilitate the induction of SVT. Atropine + adrenaline indicates that tachycardia was not induced after the administration of atropine alone, so adrenaline was administered on top to facilitate the induction of SVT. Overall, three patients necessitated adrenaline infusion for SVT induction after the administration of atropine: one patient had dual-AV nodal physiology but no tachycardia was induced after atropine alone was administrated; AVNRT was induced after subsequent adrenaline infusion and slow pathway ablation was successfully performed; for the second patient, no SVT was induced after adrenaline infusion, but he also had dual-AV nodal physiology, thus slow pathway ablation was performed; the third patient had no SVT induction after adrenaline infusion, no evidence of dual-AV nodal physiology and the procedure was terminated.
Effects of adrenaline in patients with supraventricular tachycardia
Sixty-six patients (19.6%) received adrenaline for SVT induction. Among the 66 patients with prior documented PSVT, using the above-mentioned stimulation protocols, no SVT was induced under basal conditions (prior to adrenaline administration).
After the infusion of adrenaline, sustained SVT was induced in 54 patients. Of these 54 patients, 40 had AVNRT, 11 patients had orthodromic AVRT using a concealed accessory pathway, and 3 patients had focal ATs arising from the right atrium. The sensitivity of the adrenaline test defined as the percentage of inducible sustained SVT was 82%.
We had no patient with a concealed accessory pathway and concomitant AVNRT induction.
For the 12 patients in whom tachycardia could not be induced after adrenaline infusion, atropine was added. Paroxysmal supraventricular tachycardia was subsequently induced after the administration of atropine in 11. Among them, eight patients had AVNRT, three patients had AVRT, and one patient had AT. In one patient no arrhythmia was induced but slow pathway ablation was performed because documented ECG during tachycardia was suggestive of AVNRT, and the EP study revealed the presence of dual-AV nodal morphology (Figure 2).
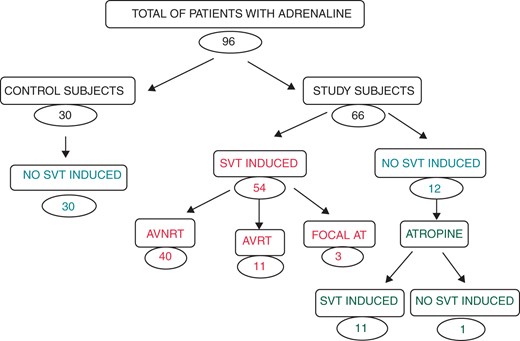
Effects of adrenaline in control subjects and in patients with documented SVT. SVT, supraventricular tachycardia; AVNRT, atrioventricular node reentrant tachycardia; AVRT=atrioventricular reentrant tachycardia using an accessory pathway as the retrograde limb; AT, atrial tachycardia.
A related-samples McNemar change test used for nominal data showed significant difference between SVT induction before and after the administration of adrenaline, P < 0.0001.
Effects of adrenaline in control subjects
Among the 30 control subjects, SVT was not induced during the EP study, neither before nor after infusion of adrenaline. The specificity, defined as the percentage of negative test in the control group, was 100%.
Diagnostic accuracy
The sensitivity and specificity of adrenaline for the induction of PSVT were 82 and 100%, respectively. The positive and negative predictive values were 100 and 71%. The overall diagnostic accuracy was 88% (Table 1).
| Sensitivity . | Specificity . | PPV . | NPV . |
|---|---|---|---|
| 82% | 100% | 100% | 71% |
| Sensitivity . | Specificity . | PPV . | NPV . |
|---|---|---|---|
| 82% | 100% | 100% | 71% |
Data shown in percentages are positive predictive value (PPV) and negative predictive value (NPV).
| Sensitivity . | Specificity . | PPV . | NPV . |
|---|---|---|---|
| 82% | 100% | 100% | 71% |
| Sensitivity . | Specificity . | PPV . | NPV . |
|---|---|---|---|
| 82% | 100% | 100% | 71% |
Data shown in percentages are positive predictive value (PPV) and negative predictive value (NPV).
Adverse effects
Adrenaline was generally well tolerated. Side effects were tremor (for which the infusion was not discontinued because it was considered tolerable by the patient), headache, and lumbar pain. The adrenaline infusion was discontinued prematurely in 2 of 96 patients (2.1%). In the first patient, headache was attributed to high systolic blood pressure >180/110 mmHg, which appeared during infusion of adrenaline at rates of 0.2 μg/kg/min. The symptoms resolved after discontinuation of adrenaline. The other patient presented lumbar pain that disappeared after the discontinuation of infusion.
Induction of non-specific arrhythmias occurred in the form of runs of premature atrial contractions (four patients = 4.2%), non-sustained AT (one patient = 1.0%), ventricular premature beats (three patients = 3.1%), but none of these influenced the overall result of the EP study.
There were no ECG changes suggestive of ischaemia in any of the patients.
Discussion
Main findings
This study demonstrates that adrenaline has a high sensitivity and specificity for the induction of SVT in patients with paroxysmal documented SVT.
In a prior study, Brembilla-Perrot et al.1 reported a sensitivity of 90% and a specificity of 100% for isoprenaline in the diagnosis of SVT.
Huycke et al.2 found a sensitivity of 67% and a specificity of 100% for isoprenaline-facilitated induction of AVNRT. However, the number of patients was lesser (20 patients) than in the study of Brembilla-Perrot (67 patients).
Stellbrink et al.4 randomized 80 patients to receive either atropine or isoproterenol before AVNRT ablation. The inducibility in the isoproterenol group increased from 58% in the baseline state to 93% after isoproterenol infusion (P < 0.001).
Pauriah et al. studied 63 patients with Wolff Parkinson White syndrome and spontaneous adverse clinical presentation (syncope or resuscitated ventricular fibrillation, VFib). At baseline orthodromic tachycardia was induced in 44% and antidromic tachycardia in 11%. After isoproterenol infusion, inducibility increased to 68.2% for orthodromic tachycardia and 22.2% for antidromic tachycardia.5
In the absence of isoprenaline, it appears that adrenaline might be an acceptable alternative, due to its high sensibility and specificity, of 82 and 100%, respectively. In our study, adrenaline was generally well tolerated with minimal side effects and with a low percentage of premature discontinuation of 2.1%.
Electrophysiological effects of adrenaline and dosage
An alternative approach to the adrenergic initiation of tachycardias facilitated by isoprenaline could be the use of adrenaline or noradrenaline. Furthermore, the use of a vagolytic agent such as atropine could facilitate the induction of tachycardias by leaving the action of natural catecholamines unopposed by the parasympathetic system and thus induce tachycardia.6
Adrenaline is a nonselective agonist of alpha- and beta-adrenergic receptors, and thus its activity, side effects, and efficacy differ from isoprenaline. The overall EP effects of adrenaline result from stimulation of the beta-adrenergic receptors. Stimulation of the alpha-adrenergic receptors by adrenaline has no effect on the AV node, but prolongs the effective refractory period of the atrium and the ventricle, partially offsetting the shortening of refractory periods mediated by beta-receptor stimulation.6,7
The mechanism by which adrenaline induces sustained SVT may be multifactorial. In physiological doses, adrenaline shortens the effective refractory period of the atrium, AV node, and ventricle and improves AV node conduction. Episodes of tachycardias induced by adrenaline are attributed to the acceleration of the sinus rate, which might sufficiently shorten the retrograde refractory periods of additional pathways (accessory pathway, slow nodal pathway) to permit retrograde conduction up the additional pathway to the atrium, thus causing an echo beat and initiate tachycardia.6,7
Because adrenaline can reproduce stress hypokalaemia, another mechanism by which adrenaline might have facilitated the induction of SVT would be a reduction in intracellular potassium.8
Probably the best way to estimate adrenergic activity after intravenous infusion is the measurement of plasma concentration of adrenaline.9 Although plasma adrenaline concentrations were not measured in our study, prior studies have determined the plasma adrenaline concentrations corresponding to the infused doses. Accordingly, an adrenaline infusion of 0.001–0.313 μg/kg/min would correspond to a plasma concentration of 0.005–3 μg/L.10–16 In our study, the doses of adrenaline required to induce the desired change in heart rate ranged from 0.1 to 0.3 μg/kg/min.
Previous studies have demonstrated that constant rate infusions are characterized by the attainment of a steady state in plasma concentrations within 5–10 min. Furthermore, steady-state concentrations are directly proportional to the rate of infusion14 In our study, adrenaline infusion was started at a dose of 0.05 μg/kg/min rate and increased every 5 min to obtain the desired increase in the heart rate, or up to a dose of 0.3 μg/kg/min. This was effective in increasing the heart rate and subsequently inducing SVT by programmed atrial stimulation.
Safety of adrenaline in patients with concealed accessory pathways
By giving adrenaline there is a theoretical risk of unmasking antegrade conduction and inducing VFib in patients who have a concealed accessory pathway. There are data in the literature indicating that isoprenaline can facilitate the unmasking of antegrade conduction of the accessory pathway.17 In the case of atrial fibrillation initiation, the pathway can conduct rapidly to the ventricles and induce VFib. However, the risk is relatively small. Our EP laboratory is properly equipped to handle such cases (defibrillator, intubation, mechanical ventilation, etc.).
Limitations
One limitation of this study is that the effects of adrenaline were assessed in conscious sedated or non-sedated patients. It is not clear whether adrenaline would have similar properties if administrated to patients under general anaesthesia.
The induction of ATs is not necessarily clinical tachycardia. In this case, the patients were always asked for their symptoms. If they were asymptomatic or their symptoms did not suggest it to be clinical tachycardia, AT was considered non-specific. The induced and clinical tachycardia may be different but may look the same on the surface ECG. However, the P wave during AT and the presence of non-sustained or sustained arrhythmia should make the difference between non-specific and specific ATs.
Finally, because the effects of adrenaline may be time-dependent, it is possible that SVT may have been induced at lower doses if more time was allowed before the increase of the infusion rate.
Conflict of interest: none declared.



