-
PDF
- Split View
-
Views
-
Cite
Cite
Demosthenes G. Katritsis, Mark E. Josephson, Classification of electrophysiological types of atrioventricular nodal re-entrant tachycardia: a reappraisal, EP Europace, Volume 15, Issue 9, September 2013, Pages 1231–1240, https://doi.org/10.1093/europace/eut100
Close - Share Icon Share
Abstract
Sequence of retrograde atrial activation is not a reliable criterion for the classification of atrioventricular nodal re-entrant tachycardia (AVNRT) into typical and atypical types. The conventional concept of a lower common pathway is not supported by current evidence and does not represent a reliable or reproducible criterion. The distinction between ‘fast–slow’ and ‘slow–slow’ forms is not unanimously defined, and probably of no practical significance. We suggest that AVNRT should be classified as typical or atypical according to the His–atrial interval or, when a His bundle electrogram is not reliably recorded, the ventriculo-atrial interval measured on the His bundle recording electrode.
Introduction
Although atrioventricular nodal re-entrant tachycardia (AVNRT) represents the most common regular supraventricular arrhythmia in humans, the precise anatomic site of its circuit and the nature of the pathways involved have not yet been established.1–3 Classification of various forms of this arrhythmia as well as the methodology of distinction between typical and atypical AVNRT have also been unsatisfactory, with different criteria adopted in the literature by investigators for both fast–slow and slow–slow AVNRT. Following the seminal report of Goldberger et al.4 on atypical AVNRT that was based on both absolute atrial–His (AH) and His–atrial (HA) times and AH/HA ratios, several criteria have been used, based on the pattern of earliest retrograde atrial activation, absolute values of AH intervals, and identification of a lower common pathway.5–10 This paper discusses these time-honoured criteria and resultant classification schemes in view of published evidence.
Earliest atrial retrograde activation
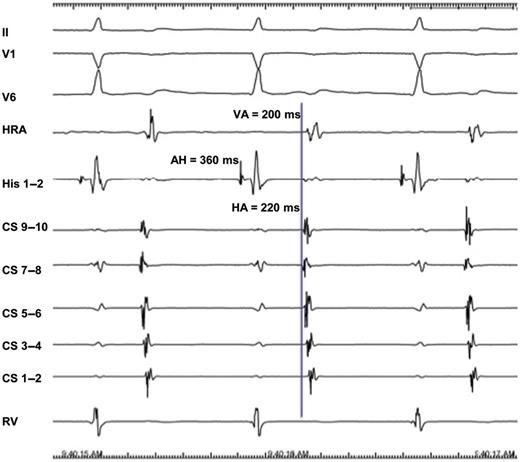
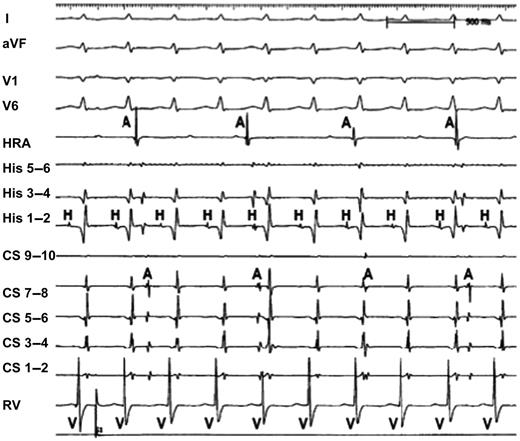
Heterogeneity of both fast and slow conduction patterns has been well described, and all forms of AVNRT may display anterior, posterior, and middle retrograde activation patterns.11–17 In certain cases of atypical AVNRT, retrograde atrial activation is even suggestive of a left lateral accessory pathway.15–17 Appropriate diagnosis in this setting is of importance for the avoidance of prolonged procedures with high fluoroscopy times and unnecessary radiofrequency (RF) lesions. In typical slow–fast AVNRT, posterior or even left atrial fast pathways may occur in up to 8% of patients.12–14 Engelstein et al.12 have identified 7 out of 130 patients (5%) with slow–fast AVNRT and earliest atrial activation at the coronary sinus (CS) ostium, while in 5 patients (4%), atrial activation was simultaneous at the His bundle and CS ostium during tachycardia. Chen et al.13 have reported earliest retrograde atrial activation at the CS ostium in 16 out of 221 patients (7.6%). Nam et al.14 have reported 3 of 52 patients with typical AVNRT where atrial activation was earliest at the His bundle, but was followed by distal coronary sinus activation that preceded activation at the ostium by 10 ms. There has also been evidence that was left septal His recordings routinely performed in patients with AVNRT, the proportion of left-sided retrograde fast pathways might be considerably higher than previously reported.18Figures 1–3 present typical AVNRT (slow–fast) with variable earliest retrograde atrial activation.

Typical slow–fast AVNRT. Earliest retrograde atrial activation is recorded either at proximal His or distal CS (CS 1–2) and proximal His (His 3–4). I–V6, 12-lead ECG leads; HRA, high right atrium; His, His bundle electrogram; CS, coronary sinus.
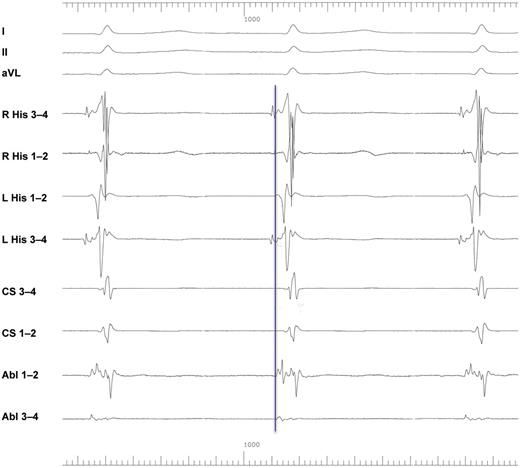
Typical slow–fast AVNRT. Simultaneous mapping of the right septum (R His), left septum (L His), and the anatomic area of the slow pathway is undertaken. Earliest retrograde atrial activation is recorded on the left septum. I–V6, 12-lead ECG leads; HRA, high right atrium; His, His bundle electrogram; CS, coronary sinus; Abl, ablation electrode at the anatomical area of the slow pathway.
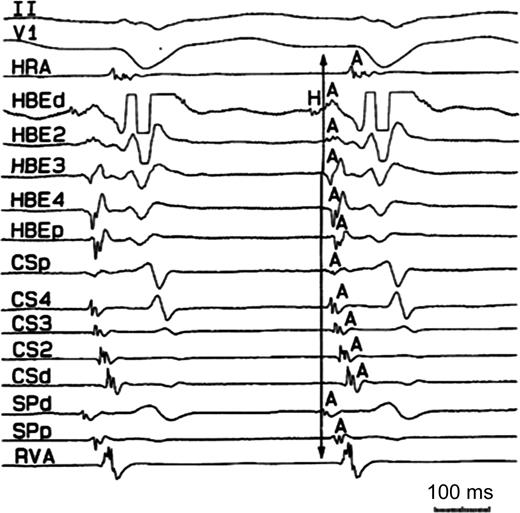
Typical AVNRT. Note multiple retrograde atrial breakthroughs as depicted by simultaneous earliest retrograde atrial activation recorded at various sites of the His bundle electrode and the anatomic area of the slow pathway. I–V6, 12-lead ECG leads; HRA, high right atrium; His, His bundle electrogram; CS, coronary sinus; SP, slow pathway; RVA, right ventricular apex.
In atypical AVNRT, the earliest retrograde atrial activation is traditionally reported at the base of the triangle of Koch, near the coronary sinus ostium. Detailed mapping of retrograde atrial activation in large series of patients, however, has produced variable results. In the series of Hwang et al.15 with 46 patients with atypical AVNRT, 20 patients (11 with slow–slow, and 9 with fast–slow type) displayed eccentric earliest atrial activation at the coronary sinus (8 lateral and 12 posterior), whereas in the series of Chen et al.13 only 2 out of 14 patients (i.e. 14.3%) with fast–slow AVNRT had earliest activation at the CS electrodes. Nawata et al.11 in a series of 12 patients with fast–slow AVNRT, identified six patients with earlier atrial activation at the coronary sinus ostium, three patients with earlier activation at the low right atrial septum, and three patients with simultaneous activation of the coronary sinus and right atrial septum. Eccentric atrial activation, 10–20 mm distal to the CS ostium, was also found in 8 out of 10 patients with atypical AVNRT by Nam et al.14 The CS ostium was the site of earliest atrial activation in only two patients. Case reports of variants of left lateral retrograde activation in slow–slow AVNRT have also been published.16,17
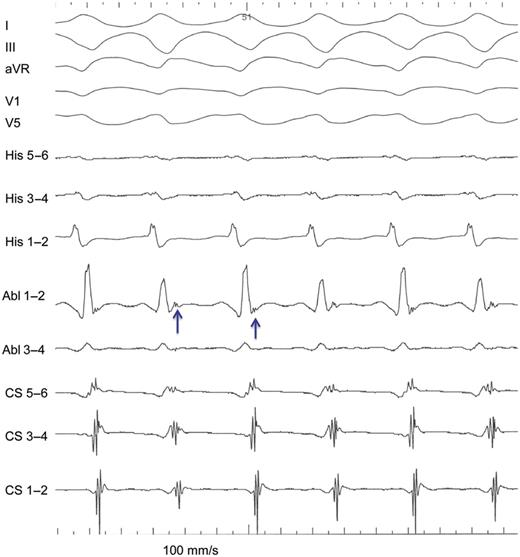
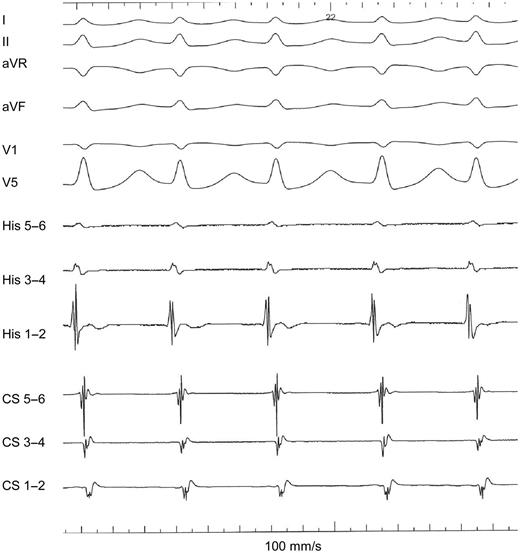
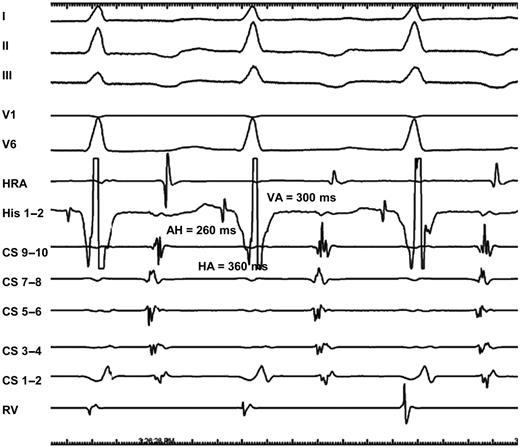
It is obvious, therefore, that classification based on earliest atrial retrograde activation is inappropriate. Figures 4 and 5 depicts fast–slow and slow–slow AVNRT, respectively, with earliest retrograde atrial activation at the His bundle electrode, whereas in Figure 6 retrograde earliest atrial activation in slow–slow AVNRT is most probably simultaneous at the His bundle and distal CS (CS 7–8). Thus, atypical forms may be compatible with earliest atrial retrograde activation at the His bundle electrogram, as typical AVNRT may display variable atrial retrograde activation. Slow–fast AVNRT with an earliest retrograde activation not at the His bundle recording electrode has been specified as ‘posterior or leftward inferior extension or left variant slow–fast AVNRT’ by Jackman and coworkers.10 We beg to differ. Typical slow–fast AVNRT is compatible with variable earliest retrograde atrial activation sites and sub-classification according to this characteristic is rather meaningless. Perhaps, the confusion in terminology originates from the study by McGuire et al.19 who described a posterior or type B form in 2% of their patients with presumed ‘slow–fast’ AVNRT. The AH/HA ratio in that study was >1 thus negating the possibility of a fast–slow form, but VA were prolonged (76–168 ms) thus indicating a slow, not fast, retrograde limb of the circuit. It is logical, therefore, to consider it as atypical AVNRT.
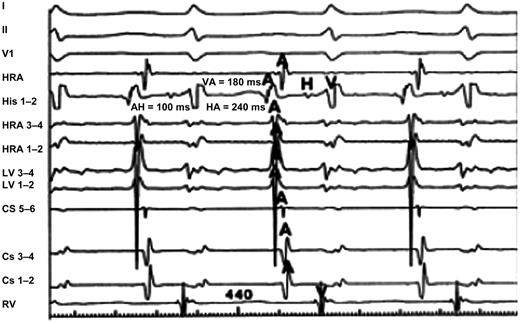
Atypical AVNRT. The form is conventionally fast–slow (AH < HA, HA > 70 ms, AH < 200 ms), and earliest retrograde atrial activation recorded at the His bundle electrode. I–V6, 12-lead ECG leads; HRA, high right atrium; His, His bundle electrogram; CS, coronary sinus; LV, electrode at the left side of the septum; RV, right ventricle.
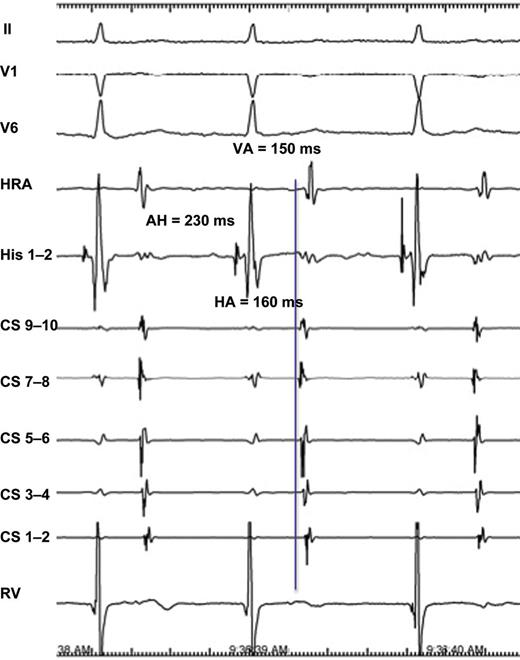
Atypical AVNRT. The form is conventionally slow – slow (AH > HA, HA > 70 ms, AH > 200 ms) and earliest retrograde atrial activation is recorded at the His bundle.
Atypical AVNRT. The form is slow–slow (AH > HA, HA > 70ms, AH > 200ms), and earliest atrial retrograde activation is recorded simultaneously at His bundle and distal CS (CS 7–8).
Lower common pathway
Early studies have considered the possibility of additional atrioventricular (AV) nodal tissue extrinsic to the tachycardia circuit to explain various electrophysiological phenomena observed during AVNRT,20 and the concepts of upper and lower common pathways have been long-standing controversies of AVNRT. The existence of an upper common pathway can now be rather easily refuted by subsequent evidence indicating that multiple atrial breakthroughs are extremely common, and retrograde activation often changes in timing and/or activation without significant alteration in tachycardia cycle, thus negating the notion of a simplistic focal atrial exit site.19,21,22 The perinodal transitional tissue is the route to the atrium, and in this context it may be considered as a common pathway of tissue but not a discrete site. The breakthrough is whatever leads to atrial activation via transitional tissue; thus there are many possibilities (Figures 3, 6, and 7).
Atrioventricular dissociation during AVNRT. Atrial activation is not related to His bundle electrograms, and the last A–A interval is not the same with the previous ones. This suggests retrograde block with variable conduction.
The lower common pathway, as initially considered by Mendez and Moe,23 has been more reluctant to die. There is also evidence, however, that if anything, it represents a concept the mechanism and relevance of which remain speculative.22 The notion of a lower common pathway has been utilized to explain the phenomena of AV block without recording of a His electrogram as well as retrograde Wenckebach periodicity during AVNRT.21,24–27 The lower common pathway is defined as the conduction path between the distal turnaround point of the AVNRT circuit and the His bundle. The conduction time over the lower common pathway has been usually estimated by subtracting the His to atrium interval during tachycardia (measured from the onset of the His electrogram to the onset of the atrial electrogram) from that during ventricular pacing (measured from the end of the His electrogram to the onset of the atrial electrogram) at the same cycle length and considered a measurable interval in the majority of typical AVNRT cases. In the initial study of Miller et al.,20 a lower common pathway was demonstrated in up to 75% of 28 patients with AVNRT who were studied, whereas in subsequent studies Anselme et al.26 with the use of para-Hisian pacing, identified the presence of a lower common pathway in 78% of 23 patients studied. Heidbuchel et al.28 have failed to detect the evidence of a lower common pathway in typical slow–fast AVNRT.
However, AV block during AVNRT without recording activation of the His bundle can also be explained by proximal intra-Hisian block.29 Li et al.30 have shown that in up to one-third of patients with AVNRT the lower turnaround point of the circuit is within the His bundle, thus arguing against an intranodal circuit as a universal feature of AVNRT. Differences in the location of the lower turnaround sites of AV nodal re-entry relatively to the His bundle have also been shown in experimental studies.31 Thus, block during AVNRT does not necessarily define a ‘lower common pathway’; it just defines longer refractory period below the circuit. This is often seen at the onset of very fast AVNRT, which may expose the His-Purkinje tissue to long–short periods and can lead to functional phase 3 block, having nothing to do with the re-entrant circuit.
The electrophysiological proof of the existence of a lower common pathway depends on several assumptions that may not be valid. The necessary conditions are: retrograde fast pathway conduction is the same during pacing and tachycardia, the recording of the proximal His bundle potential corresponds to the proximal end of the His bundle, the beginning of the antegrade His bundle potential during tachycardia and the end of the retrograde His bundle potential during ventricular pacing represent activation at the same site, and autonomic tone remains the same during tachycardia and ventricular pacing. These assumptions are far from proven. Detailed mapping of both sides of the septum has revealed that earliest retrograde atrial activation may well be on the left side for both fast and slow pathways,18,32 and that the breakthrough of atrial activation is discordant from that observed during ventricular pacing in up to 43% of patients with slow–fast AVNRT.18 Even if a lower common pathway exists, therefore, applied methodologies are unable to detect and measure it. Thus, electrophysiological findings suggesting the presence of a lower common pathway can be interpreted in various ways outside the context of a common pathway in most cases. Recent studies from Efimov's lab suggest a three-dimensional AV node with greater variability in the space constant of tissue and poor gap junction connectivity due to differential expression of connexin isoforms, which provide an explanation of dual conduction and nodal re-entrant arrhythmogenesis.33,34 It is very difficult to conceive the presence of ‘common’ pathways in this environment.
Furthermore, the practical applicability of the method is questionable. There are certain cases in the electrophysiology laboratory where an antegrade, let alone a retrograde, His bundle electrogram may not be reproducibly and reliably recorded.20–35Figure 8 depicts a case of AVNRT conducted with left bundle branch abnormality (LBBB) aberration and with inability to record His bundle electrograms during tachycardia despite prolonged efforts. The ablation electrode is positioned at the anatomic area of the slow pathway and depicts retrograde atrial electrograms simultaneously with those recorded by the CS electrode. There is also evidence of alternating VA conduction, a sign previously reported with AVNRT and compatible with the hypothetical model of type-8 re-entry that has been proposed based on the concept of posterior nodal extensions.3 After an atrial tachycardia was excluded, one RF application at the anatomic area of the slow pathway induced a nodal rhythm and rendered the tachycardia non-inducible.
Typical AVNRT conducted with LBBB aberration and with inability to record His bundle electrograms. Retrograde atrial electrograms are indicated by arrows.
Relative AH/HA intervals
The AH time and the relative AH/HA intervals have been proposed as a criterion for distinction between fast–slow and slow–slow AVNRT. However, both absolute and relative values may be meaningless in certain occasions. They depend on autonomic status, age, use of isoprenaline and sedatives, and conduction properties of pathways involved, and may change during a single electrophysiological study. We have often noted different AH/HA times in the same patient at similar or different tachycardia cycle lengths. Furthermore, when a His bundle electrogram cannot be recorded during tachycardia, a diagnosis based exclusively on them is impossible. Figure 9 depicts a typical case of slow–fast AVNRT with simultaneous occurrence of antegrade ventricular and retrograde atrial activation and, again, with inability to record a stable His electrogram. A very short VA interval establishes the diagnosis, after having excluded atrial tachycardia and orthodromic AVRT.
Typical AVNRT with simultaneous occurrence of antegrade ventricular and retrograde atrial activation and inability to record a stable His electrogram.
Proposed classification criteria
A scheme for the classification of various forms of AVNRT that has attempted to overcome existing uncertainties has been proposed.2 We suggest an even more simplified scheme (Table 1).
| . | HA . | VA (His) . | AH/HA . |
|---|---|---|---|
| Typical AVNRT | ≤70 ms | ≤60 ms | >1 |
| Atypical AVNRT | >70 ms | >60 ms | Variable |
| . | HA . | VA (His) . | AH/HA . |
|---|---|---|---|
| Typical AVNRT | ≤70 ms | ≤60 ms | >1 |
| Atypical AVNRT | >70 ms | >60 ms | Variable |
AH, atrial to His interval; HA, His to atrium interval; VA, interval measured from the onset of ventricular activation on surface ECG to the earliest deflection of the atrial activation on the His bundle electrogram.
The distinction is for categorization only, and not relevant for mechanism or therapy.
Atypical AVNRT has been traditionally classified as fast–slow (HA > 70 ms, VA > 60, AH/HA < 1, and AH < 200 ms) or slow–slow (HA > 70 ms, VA > 60 ms, AH/HA > 1, and AH > 200 ms). Not all of these criteria are always met and atypical AVNRT may not be sub-classified accordingly.
| . | HA . | VA (His) . | AH/HA . |
|---|---|---|---|
| Typical AVNRT | ≤70 ms | ≤60 ms | >1 |
| Atypical AVNRT | >70 ms | >60 ms | Variable |
| . | HA . | VA (His) . | AH/HA . |
|---|---|---|---|
| Typical AVNRT | ≤70 ms | ≤60 ms | >1 |
| Atypical AVNRT | >70 ms | >60 ms | Variable |
AH, atrial to His interval; HA, His to atrium interval; VA, interval measured from the onset of ventricular activation on surface ECG to the earliest deflection of the atrial activation on the His bundle electrogram.
The distinction is for categorization only, and not relevant for mechanism or therapy.
Atypical AVNRT has been traditionally classified as fast–slow (HA > 70 ms, VA > 60, AH/HA < 1, and AH < 200 ms) or slow–slow (HA > 70 ms, VA > 60 ms, AH/HA > 1, and AH > 200 ms). Not all of these criteria are always met and atypical AVNRT may not be sub-classified accordingly.
In typical slow–fast AVNRT the onset of atrial activation appears prior, at the onset or just after the QRS complex thus maintaining an AH/HA ratio >1. The HA interval is usually <70 ms, measured from earliest deflection of the His bundle activation to the earliest rapid deflection of the atrial activation in the His bundle electrogram, and the VA interval, measured from the onset of ventricular activation on surface electrocardiogram (ECG) to the earliest rapid deflection of the atrial activation on the His bundle electrogram, is <60 ms. We propose only the AH/HA and absolute HA intervals as criteria for diagnosis of typical AVNRT. The VA interval is also a practical and easily obtainable criterion, when the His bundle potential cannot be reproducibly and reliably recorded during tachycardia (Table 1).
In atypical fast–slow form of atypical AVNRT, the retrograde atrial electrogram begins after ventricular activation with an AH/HA ratio <1. The HA interval is prolonged, ≥70 ms, and the VA interval is ≥60 ms. It has been proposed that the AH interval should be <185 ms10 or 200 ms,5 to establish the diagnosis of a truly fast–slow form, but this criterion has not been adopted by other investigators.11,14,15 The atypical slow–slow form represents, by definition, an arrhythmia utilizing two slow pathways. The AH/HA ratio is ≥1 but the HA interval is ≥70 ms, and the AH interval exceeds 200 ms.4,16,17 Thus, tachycardias with a relatively prolonged AH interval but an AH/HA ratio <1 cannot be reliably classified as either fast–slow or slow–slow (Figure 10). We propose only the HA interval as a criterion for diagnosis of atypical AVNRT. Again, the VA interval can be used when the His bundle potential cannot be reproducibly and reliably recorded during tachycardia (Table 1). Sub-classification to fast–slow or slow–slow is on certain occasions arbitrary.
Atypical AVNRT. The form is fast–slow according to the AH < HA definition, but slow–slow according to the AH > 200 ms criterion.
In view of the presented evidence, retrograde atrial activation sequence should not be necessarily considered as a criterion for classification of AVNRT types. Similarly, the demonstration of a lower common pathway is not a reliable and easily applicable criterion. Finally, the distinction between fast–slow and slow–slow atypical AVNRT is often arbitrary in view of the lack of a unanimously accepted definition. Based on these observations, we have analysed a series of consecutive AVNRT cases that were diagnosed and ablated by the same operator (D.G.K.). Atrioventricular nodal re-entrant tachycardia was diagnosed with certainty by: Using the criteria mentioned above, 11 out of 277 patients (4%) had atypical AVNRT. Of those, four patients (1.4%) had fast–slow AVNRT according to both the AH < HA and AH < 200 ms, and four patients (1.4%) had slow–slow AVNRT. The remaining three patients (1.1%) could not be reliably classified due to borderline or variable intervals. It might be possible that higher rates of atypical AVNRT reported by other authors are exaggerated exactly because of the use of criteria such as the demonstration of characteristics compatible with the notion of the lower common pathway. Examples are Figures 59.31 and 59.33 by Lockwood et al.,10 Figure 4 by Heidbuchel and Jackman,5 and Figures 5 and 6 by Yamabe et al.8 Tachycardias have been diagnosed as slow–slow but their characteristics are compatible with typical slow–fast type. Employment of the criteria proposed in this article, offers a rational and clinically practical way to classify AVNRT types.
1. Fulfillment of established criteria during detailed atrial and ventricular pacing manoeuvres.
2. Abolition of the tachycardia by anatomic ablation of the slow pathway as previously described.
3. Absence of arrhythmia recurrence, or in case of recurrence, abolition of the arrhythmia by repeat anatomic slow-pathway ablation.
Clinical implications
The proposed classification scheme, and consideration of AVNRT in general, has the following practical implications: Conflict of interest: none declared.
1. Retrograde atrial activation during tachycardia should not be relied upon as a diagnostic criterion. Both typical and atypical AVNRT are compatible with varying retrograde atrial activation patterns; keeping this in mind may avoid unnecessary ablation lesions.
2. Attempts at establishing the presence of a ‘lower common pathway’ are scientifically unjustified and of no practical significance. They may result in unnecessarily prolonged procedures.
3. When the diagnosis of AVNRT is established, ablation should only be directed towards the anatomic position of the slow pathway. If right septal attempts are unsuccessful, the left septal side should be tried.36
4. Ablation targeting earliest atrial activation sites during typical AVNRT or the fast pathway in general for any kind of typical or typical AVNRT, is not justified.



