-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Di Rienzo, Vittorio Racca, Francesco Rizzo, Bruno Bordoni, Gianfranco Parati, Paolo Castiglioni, Paolo Meriggi, Maurizio Ferratini, Evaluation of a textile-based wearable system for the electrocardiogram monitoring in cardiac patients, EP Europace, Volume 15, Issue 4, April 2013, Pages 607–612, https://doi.org/10.1093/europace/eus368
Close - Share Icon Share
Abstract
We developed a textile-based wearable system, named MagIC, for the unobtrusive monitoring of one electrocardiogram (ECG) lead, respiratory frequency and motion. In the present study, we investigated the ability of this system to monitor cardiac rhythm and arrhythmic events in cardiac patients.
The study was carried out by comparing ECG tracings simultaneously recorded by MagIC and traditional ECG devices (Trad-ECG) in 40 cardiac patients at rest and during physical exercise. Data were manually scored by two cardiologists. At rest the artefact rates observed with MagIC and Trad-ECG were virtually identical (1.4% of the registered signal); while during physical exercise the artefact rate observed with MagIC was much lower than with Trad-ECG (4.07 vs. 17.31%). Recordings from MagIC allowed a correct identification of the type of rhythm in the vast majority of patients (92.5%) and an estimation of PQ interval and QRS duration similar to Trad-ECG (<0.016 s). MagIC displayed a good performance in detecting arrhythmias, with only 14 misclassified events out of 3618, and both specificity and sensitivity being above 99%. No practical difference was observed in the estimation of the beat-by-beat RR interval by the two methods.
This study indicates that in static condition MagIC has a capability of monitoring cardiac rhythm and arrhythmic events which is comparable with what obtainable by a traditional one-lead ECG recorder. During movement MagIC provides an ECG signal of better quality.
We developed a textile-based wearable system, for the unobtrusive monitoring of one electrocardiogram (ECG) lead, respiratory frequency, and motion. In the present study, we investigated the ability of this system to monitor cardiac rhythm and arrhythmic events in cardiac patients. To the best of our knowledge this study represents the first systematic evaluation of a textile monitoring system for clinical use.
This study indicates that in static condition the textile system has a capability of monitoring cardiac rhythm and arrhythmic events which is comparable with what obtainable by a traditional one-lead ECG recorder. During movement the textile system provides an ECG signal of better quality.
Introduction
The ‘care continuum’ represents an important advancement for the patient assistance and the health system organization. The practical application of the ‘care continuum’ concept, also implies the availability of devices able to remotely monitor the health status of patients at risk during daily living, either at home (in the frame of home care and telemedicine programmes) or during outdoor activities. From the patient's perspective, it is essential that these systems be comfortable, simple to use, and not interfering with spontaneous activities. In addition, it would be desirable to reduce or even completely avoid the need of the manual application of sensors and wires on the body, in order to avoid errors and misplacements.
Over the years, different innovative devices, including sensorized belts1 (http://www.zephyr-technology.com/products/bioharness_bt) and patches (http://www.irhythmtech.com/zio-solution/zio-patch/index.html, http://www.vpatchmedical.com/) have been proposed for a simplified monitoring of cardiac activity in freely moving subjects. The firsts are mainly used in sport and fitness areas while the seconds are designed for spot Holter assessments. Applicability of these devices for a prolonged remote surveillance of the patient should still be validated.
A different and interesting solution to the ‘care continuum’ needs was suggested in 1996 at the Massachusetts Institute of Technology in Boston, when researchers foresaw the possibility to obtain an unobtrusive monitoring of vital signs, including the electrocardiogram (ECG) by underwear garments embedding textile sensors.2 Since then, several groups in the world3–5 (http://vivonoetics.com/products/sensors/smartex-wearable-wellness-system/, http://www.smartlifetech.com/technology/Health-Vest-/), including our team, have been working on the implementation of this innovative concept. Details on research activities in this area can be found in refs.6,7
Partial transpositions of the idea of sensorized garment are also available. They include systems that either integrate into the garment the wiring but still use traditional adhesive electrodes (http://www.vitaljacket.com/), or make use of embedded wiring and textile electrodes but only provide heart rate values and not disclose the ECG waveform (http://www.numetrex.com/).
In our laboratory, a full-featured textile-based garment, named MagIC (Maglietta Interattiva Computerizzata), is currently available and functioning. This system can detect one ECG lead, respiratory frequency, and the subject's movement. Applicability of MagIC has been tested on more than 200 subjects, including healthy subjects during daily activities, physical exercise, exposure to gravitational stress8,9 as well as to high-altitude environments (at the base and advanced camps on Mount Everest, 5400–6800 m asl; and at the Margherita Hut on Monte Rosa, Italian Alps, at 4554 m asl).10–12
In the present study, we specifically investigated the ability of MagIC to monitor cardiac rhythm and arrhythmic events in cardiac patients. This was done by comparing ECG tracings simultaneously recorded by our system and by traditional ECG devices in patients at rest and during physical exercise. In this validation we focused on signal quality, morphology of the ECG waveform and on the ability of MagIC to monitor cardiac rhythm and to detect arrhythmic events.
To the best of our knowledge this study represents the first systematic evaluation of a textile-based monitoring system in a clinical setting.
Methods
System description
The MagIC System is composed of a vest with embedded textile sensors, and a portable electronic board having size and weight of a mobile telephone (see Figure 1). The vest is mainly made of cotton and elastan and is fully washable. One ECG lead is obtained by two knitted electrodes, made by conductive fibres, integrated in the vest at a level approximately corresponding to the fifth intercostal space at the intersection with the left and right anterior axillary lines; the contact between textile electrodes and the thorax is obtained by the elastic properties of the garment. After an extensive series of experiments such position of electrodes was selected because less sensitive to movement artefacts. To further improve the signal quality a small amount of conductive gel can be applied on the textile electrodes before wearing the garment. Just below the electrodes, the vest also integrates a textile-based piezoresistive plethysmograph that detects changes in the thorax circumference from which respiratory frequency is derived. Textile pathways made of the same conductive fibres connect the above sensors with the electronic module which is hooked to the vest by a Velcro strip. Electronics includes a three-axis accelerometer to detect the subject's movements, it stores data on a local memory card and can transmit all signals via a Bluetooth connection to an external device (PC or smartphone) for data visualization, storage and, possibly, a relay transmission via WiFi or UMTS channels to a remote monitoring station. The ECG signal is digitized at 200 Hz, the other signals at 50 Hz with a 12 bit resolution. The system is powered by a rechargeable lithium-ion battery allowing more than 72 h of continuous data storage per charge (30 h in the case of continuous Bluetooth data transfer). The vest is available in different sizes with a front or lateral opening and a Velcro or zip fastener to facilitate wearing by people with movement difficulties (e.g. elderly subjects or patients after a recent cardiothoracic surgery).
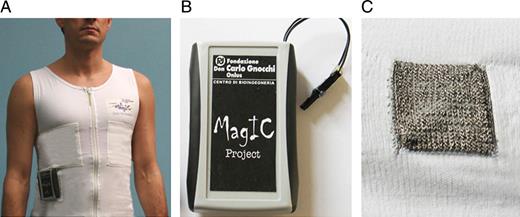
(A) MagIC system used for the study. (B) Particular of the portable electronic module. (C) Particular of the woven ECG electrode.
According to the approach selected for data storage and transmission, the system can thus be used for: a 24–72 h Holter monitoring (data are directly stored on the local memory card and can be read at the end of the whole recording period); a telemetric online monitoring (data are transmitted via Bluetooth from MagIC to the home gateway of a telemedicine platform or any other monitoring station located within a range of 10–20 m); remote online monitoring (data are transmitted via Bluetooth to a smartphone that re-transmits data in real-time through a Wi-Fi or UMTS connection to a remote computer via Internet).
Further details on the system and its applications can be found in refs.10–12
Experiment description
Forty male cardiac patients of the Cardiac Rehabilitation Unit of Fondazione Don Gnocchi have been enrolled for the study [group age: 66.72±11.4 years, mean±sd, range: 29–81 years; group weight: 73.6±11.0 kg, range: 52.0–104.0 kg; group body mass index (BMI): 26.5±4.0, range: 20.3–36.0]. Patients suffered from coronary artery disease, cardiac valve disease, or chronic heart failure. Eight patients were wearing a pacemaker. In each patient ECG was simultaneously monitored by MagIC and a traditional ECG device (Trad-ECG).
In 20 patients, whose clinical conditions were particularly severe, the recording was performed for a period of 30 min while the subjects were at rest in bed in the hospital cardiac unit. These subjects have been recruited because of their high rate of arrhythmic events. In this case, the reference Trad-ECG was the Cardioline Delta 1, Trento, Italy.
In the remaining 20 patients ECG recordings were performed for a period of 36 min during sessions of physical rehabilitation according to the following protocol: at rest (4 min lying, 1 min standing), during mild calisthenic physical exercise (10 min), while pedaling on a cycloergometer (15 min) and during a 6 min walking test. In this case, the reference ECG device was the Fukuda Denshi telemetric ECG (mod DS 5700, Tokyo, Japan).
Four standard adhesive AgCl electrodes were used for the reference recordings from the Trad-ECGs. They were placed on the left shoulder, right shoulder, fifth intercostal space (left midclavicular line), and fourth intercostal space (right midclavicular line). From these electrodes, lead I or lead II were selected for the ECG recording, based on the quality of the obtained signal, as usually done in the clinical practice. Attention was paid to avoid any interference between textile and traditional electrodes. Patients undergoing rehabilitation were asked to clothe themselves with the MagIC vest to evaluate its easiness of use.
The research protocol was approved by the Ethics Committee of Fondazione Don Gnocchi and the subjects provided their informed consent.
Data processing
The ECG signal measured by MagIC was stored on the memory card of the system, while the concomitant Trad-ECG was recorded on a notebook computer at 200 Hz (namely at the same sampling frequency used by MagIC). At the beginning and at the end of each recording an artificial artefact was produced by tapping on the MagIC and Trad-ECG electrodes simultaneously, so as to obtain an exact synchronization of the data.
After each recording, the entire tracings obtained by MagIC and Trad-ECG were plotted at 25 mm/s on separate report sheets and labelled with an anonymous code from which neither the patient nor the system used for the recording could be identified. At the end of the whole experiment, the 80 reports were manually analysed in a blind manner by two cardiologists who identified and annotated (i) artefacts (defined as segments of signal in which the different waves of the ECG complex could not be clearly identified), (ii) morphology of the ECG waveforms and (iii) rhythm abnormalities, with particular focus on atrial fibrillation, atrial flutter, and supraventricular and ventricular ectopic beats (isolated and repetitive).
Signal quality (SQ) was quantified as the percentage of recorded signal without artefacts. Artefacts rate was scored as 100-SQ. Differences in SQ between MagIC and Trad-ECG recordings were estimated by the Wilcoxon matched pairs test.
Concerning the ECG signal, the following parameters were considered (i) readability of the P-wave, (ii) PQ interval (iii) the shape of QRS complex as classified by the traditional nomenclature (Q = first negative deflection before positive, R = any positive deflection, S = first negative deflection after a previous positive one; capital letters for major and small letters for minor deflections), (iv) QRS duration, and (v) T-wave morphology (classified as positive, negative, or biphasic). PQ interval and QRS duration were estimated from the first 10 beats of each recording and differences in the evaluation of these time lengths were quantified by the rooted mean square error (RMSE) index.
The ability of the MagIC system to detect rhythm abnormalities was evaluated by matching the beat-by-beat annotations made by the cardiologists on the report sheets of the corresponding MagIC and Trad-ECG recordings. The 2 × 2 contingency table was created by considering (i) the number of true positive (TP) events, i.e. ectopic beats observed in both recordings; (ii) the number of true negative (TN) events, i.e. normal sinusal beats observed in both recordings; (iii) the number of false-positive (FP) events, i.e. normal beats for Trad-ECG but ectopic beats for MagIC; and (iv) the number of false-negative (FN) events, i.e. ectopic beats for Trad-ECG but normal beats for MagIC. Sensitivity and specificity indices were defined as TP/(TP+FN) and TN/(TN+FP), respectively.
Additionally, we evaluated the accuracy of MagIC to provide a correct beat-by-beat RR interval (RRI) measure. For this purpose in a subgroup of 17 subjects beat-by-beat RRI values were measured from the whole MagIC and Trad-ECG tracings. To increase the measure resolution, the apex of every sampled R peak was interpolated by a parabola and the true time location of the R peak was obtained by determining in an analytical way the position of the apex of the interpolating parabola. This procedure was reported to increase the precision of the RRI estimate.13 For each heart beat, the RRI values obtained by MagIC and Trad-ECG were compared and the absolute value of the difference was computed.
The level of comfort of the patients in wearing the system was qualitatively assessed by an interview at the end of each recording session.
Results
In this study, 97320 heart beats were considered for the system validation.
Signal quality and artefact rate
In the group of patients at bed rest, the ECG signal was readable (namely, every wave in the ECG complex could be clearly detected) on average for 98.58 ± 0.89% (mean ± sd) of the recording time when detected by MagIC and for 98.57 ± 0.68% of the recording time when detected by Trad-ECG. These figures correspond to an artefact rate of 1.42% for MagIC e 1.43% for Trad-ECG. During physical exercise, the ECG signal was readable for 95.93 ± 1.13% of the recording time when recorded by MagIC and for 82.69 ± 3.12% of the recording time by Trad-ECG. These values are statistically different (P < 0.002) and correspond to artefact rates of 4.07 and 17.31%, respectively.
Morphology
Examples of ECG signals simultaneously recorded by MagIC and Trad-ECG are shown in Figure 2. In spite of the different electrode location, morphology of ECG waveforms detected by MagIC and Trad-ECG was similar (according to the criteria illustrated in Methods) in the majority of the patients. Indeed we observed that shape of the QRS complex estimated by MagIC and Trad-ECG was comparable in 29 patients (72.5% of the considered population, see example in Figure 2A–G) while the morphology of T-wave was similar in 32 patients (80.0%). An example of opposite T polarity in a patient with a pacemaker is shown in Figure 2F. Similarity in waveform morphology was not correlated with the type of lead configuration used in Trad-ECG (I or II).
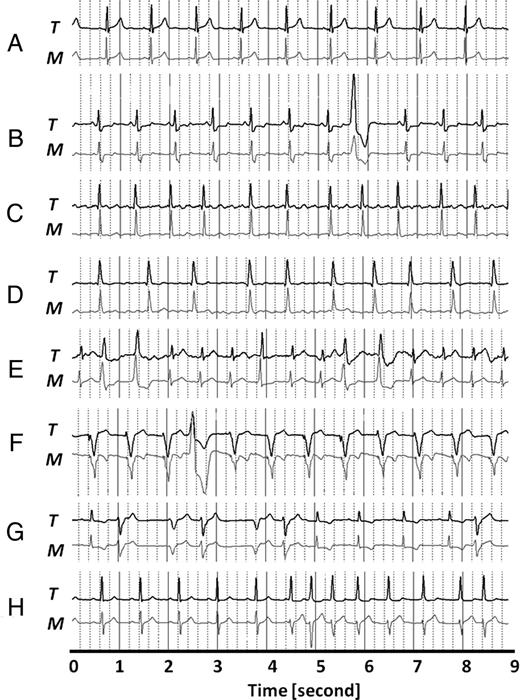
Examples of pairs of electrocardiogram tracings simultaneously obtained by Magic (M) and Trad ECG (T) in different patients. (A) Patient with normal sinusal rhythm. (B) Ventricular ectopic beat in a patient with ST depression. (C) Patient with atrial fibrillation (the f-wave is more evident in T than in M). (D) Other patient with atrial fibrillation (the f-wave is more evident in M than in T). (E) Patient with polymorphic ventricular ectopic beats. (F) Patient with pacemaker. (G) Patient with couplets of ventricular ectopic beats. (H) Patient during the onset of atrial fibrillation (in this patient during sinusal rhythm, the QRS morphology was different in the two recordings: type R for Trad-ECG and type RS for MagIC).
PQ intervals and QRS durations estimated by the two techniques were comparable and the average error, as quantified by the RMSE index, was very small: 0.016 s for PQ interval and 0.00 8s for QRS duration.
Rhythm
The type of rhythm could be correctly identified in 37 out of 40 patients (92.5% of the overall population), including 28 patients with sinus rhythm, 5 patients with atrial fibrillation (example in Figure 2C, D and H) and 4 patients with pacemaker (example in Figure 2F). In two patients the rhythm could not be clearly assessed because the P-wave was not evident in the MagIC signal. In one subject with atrial fibrillation the F-wave in MagIC was present but with a reduced amplitude than in Trad-ECG (see Figure 2C).
Ectopic beats
From the analysis of all the Trad-ECG recordings 3618 ectopic beats were identified. As shown in Table 1, the analysis of the MagIC recordings allowed the correct identification of 3609 events with only 14 events misclassified. Thus, sensitivity and specificity of the MagIC system in detecting arrhythmic events both resulted to be extremely high (99.7 and 99.9%, respectively). Examples are shown in Figure 2B, E–G.
| . | Trad-ECG ectopic beats . | Trad-ECG normal beats . |
|---|---|---|
| MagIC ectopic beats | 3609 (true positive) | 5 (false positive) |
| MagIC normal beats | 9 (false negative) | 93697 (true negative) |
| . | Trad-ECG ectopic beats . | Trad-ECG normal beats . |
|---|---|---|
| MagIC ectopic beats | 3609 (true positive) | 5 (false positive) |
| MagIC normal beats | 9 (false negative) | 93697 (true negative) |
| . | Trad-ECG ectopic beats . | Trad-ECG normal beats . |
|---|---|---|
| MagIC ectopic beats | 3609 (true positive) | 5 (false positive) |
| MagIC normal beats | 9 (false negative) | 93697 (true negative) |
| . | Trad-ECG ectopic beats . | Trad-ECG normal beats . |
|---|---|---|
| MagIC ectopic beats | 3609 (true positive) | 5 (false positive) |
| MagIC normal beats | 9 (false negative) | 93697 (true negative) |
Details on the classification of the ectopic beats estimated by MagIC and Trad-ECG are reported in Table 2.
| . | MagIC . | Trad-ECG . |
|---|---|---|
| Supraventricular ectopic beats—isolated | 655 | 657 |
| Supraventricular ectopic beats—runs | 7 | 8 |
| Ventricular ectopic beats—isolated | 1256 | 1246 |
| Ventricular ectopic beats—couplets | 121 | 123 |
| Ventricular ectopic beats—triplets | 163 | 163 |
| Non-sustained ventricular tachycardia—runs | 106 | 105 |
| . | MagIC . | Trad-ECG . |
|---|---|---|
| Supraventricular ectopic beats—isolated | 655 | 657 |
| Supraventricular ectopic beats—runs | 7 | 8 |
| Ventricular ectopic beats—isolated | 1256 | 1246 |
| Ventricular ectopic beats—couplets | 121 | 123 |
| Ventricular ectopic beats—triplets | 163 | 163 |
| Non-sustained ventricular tachycardia—runs | 106 | 105 |
| . | MagIC . | Trad-ECG . |
|---|---|---|
| Supraventricular ectopic beats—isolated | 655 | 657 |
| Supraventricular ectopic beats—runs | 7 | 8 |
| Ventricular ectopic beats—isolated | 1256 | 1246 |
| Ventricular ectopic beats—couplets | 121 | 123 |
| Ventricular ectopic beats—triplets | 163 | 163 |
| Non-sustained ventricular tachycardia—runs | 106 | 105 |
| . | MagIC . | Trad-ECG . |
|---|---|---|
| Supraventricular ectopic beats—isolated | 655 | 657 |
| Supraventricular ectopic beats—runs | 7 | 8 |
| Ventricular ectopic beats—isolated | 1256 | 1246 |
| Ventricular ectopic beats—couplets | 121 | 123 |
| Ventricular ectopic beats—triplets | 163 | 163 |
| Non-sustained ventricular tachycardia—runs | 106 | 105 |
RRI accuracy
The absolute value of the discrepancies in the RRI estimates obtained by Magic and Trad_ECG was 1.04 ± 0.60 ms.
Comfort
Thirty-eight out of 40 patients found the vest comfortable during activity and preferable to the standard technique because it simplified the initial set-up and avoided the nuisance related to the final detachment of the adhesive electrodes. The subjects reported that the level of adherence of the vest did not interfere with movements.
Discussion
MagIC is a textile-based device developed for the unobtrusive assessment of vital signs during spontaneous behaviour. The integration of sensors in the vest structure prevents their possible misplacement and detaching under massive sweating thus facilitating the self-management of the system by the user. Moreover, the smooth and silky surface of the textile electrodes does not irritate the skin, and this makes the system suitable for prolonged and/or frequent recordings even in patients with delicate skin (e.g. children or elderly subjects).
In this study, we investigated the performances of this device in the assessment of cardiac rhythm and arrhythmic events in cardiac patients at rest and during physical exercise.
The crucial issue to be addressed while designing a smart garment is the maintenance of good signal quality during movement. Indeed, textile electrodes do not have any adhesive means, and stability in the contact between electrodes and thorax is obtained by the proper level of compression of the garment and the correct location of electrodes. The results observed in this study indicate that the adopted structural solutions are adequate to guarantee a reliable and comfortable monitoring also in a dynamical context. Indeed, we observed that for the patients at rest the artefact rate of MagIC is virtually identical to the reference; while during physical exercise the artefact rate observed with MagIC is markedly lower (−76%). The latter result may be explained by considering that in Trad-ECG the level of artefacts importantly increase during exercise because of the movement of connection cables and of a possible partial or complete detaching of the electrodes caused by sweating.
We recall that in MagIC the electrodes are placed in an ‘unconventional’ position to reduce movement artefacts. Thus, differences in the shape of the ECG waveform can be expected from the comparison with data recorded by Trad-ECG (where standard lead I or II were adopted). Conversely, our data show that QRS complex and T-wave are similar in the majority of the patients (62.5% for QRS complex and 80.0% for T-wave).
However, independently from the similarity in morphology, the main interest of the study was to check if the MagIC vest could provide reliable information on cardiac rhythm, timing among ECG waves, and occurrence of arrhythmic events. In this respect we observed that the type of rhythm could be correctly identified by the MagIC system in the vast majority of patients and the estimation of PQ interval and QRS duration from MagIC and T-ECG recordings showed only minimal discrepancies. A clinically important feature of MagIC is its ability to reliably detect arrhythmias, as shown by a failure rate <0.5% (only 14 misclassified events out of 3618) and by the corresponding high values of specificity and sensitivity.
No practical difference was found in the estimation of the beat-by-beat RR interval as estimated by MagIC and T-ECG.
Parenthetically, the above positive results have been obtained in a population with an average BMI = 26.5 and individual BMI values ranging from 20.3 to 36.0. Thus, the quality of the ECG signal assessed by the garment does not seem to be influenced by body weight excess, at least up to class I obesity.
In conclusion, this study indicates that the textile system has a capability of detecting cardiac rhythm and arrhythmic events which is similar to what is obtainable by a traditional one-lead ECG recorder. As an additional advantage, MagIC may provide a signal of better quality during physical activity than the traditional recorders. These characteristics when coupled with the above-mentioned easiness of use, comfort and possibility to either locally store or transmit data to a proximal or remote monitoring station, make the system suitable for a clinical use whenever the focus is on cardiac rhythm monitoring.
Clinical areas of applications of the system include home care and telemedicine services for the remote surveillance of arrhythmic events in subjects at risk such as elderly people, patients with chronic heart failure, coronary artery disease, etc. Recently, tests have been started in our lab to evaluate a further applicability of the smart garment also in the context of telerehabilitation programmes. This service would allow early discharged cardiac patients to attend their physical rehabilitation programme at home under a supervised remote control of their vital parameters.
Within the hospital area the system can be used to monitor subjects in whom a prolonged assessment of heart rhythm can hardly be obtained by the traditional approaches (e.g. in children—a specific version of the vest for them is under development—or in subjects with cognitive impairments) because of a poor compliance with the usual systems or because of skin irritations. It should be emphasized, however, that MagIC is intended for a prolonged personal use. Thus, it is particularly suited for patients that are required to perform repeated ECG recordings over time. For this reason, the vest is available in different sizes to fit individual body conformation and is easily washable as a traditional personal piece of cloth. When only a spot ECG assessment is required maybe the traditional approach based on adhesive disposable electrodes is still preferable, thus avoiding the need of the vest sterilization on shifting from a patient to the other.
Improvements in the system are now in progress. The first refers to the development of the female version of the system that was not available for this study (see the Limitation section). Actually, this is a difficult task, requiring a careful re-design of the vest. Indeed, a simple reshaping of the vest to comply with the female structure of the chest is not sufficient to produce the proper level of adherence of the textile electrodes on the thorax and more sophisticated tailoring actions have to be identified and implemented.
Further improvements refer to the miniaturization of the electronic board and the additional simultaneous measure of the thoracic electrical impedance (to estimate the thoracic fluid content and stroke volume) and the seismocardiogram (i.e. the assessment of micro-vibrations produced by the heart contraction and blood ejection into the aorta, from which indexes of cardiac mechanics can be derived14).
Limitations
We acknowledge one limitation of the system and two limitations of the study.
Concerning the system, the vest embeds two electrodes and thus only one ECG lead is available. As said, this configuration was due to the need to simplify the whole system and this strategy led to the advantage of getting good performances also in a dynamic context, and a significant reduction in size and weight of the electronic module. The implicit limitation of this choice is that no reliable information can be guaranteed on the ischaemic changes in the ST segment.
Concerning the study, this was performed on males only because the female version of the vest was not yet available at the moment of the data collection. In addition, in this study we evaluated the performances of the system in the identification of major and more frequent arrhythmic events. We have not directly investigated the system capability of recognizing other kinds of severe arrhythmias, such as sustained ventricular tachycardia, Torsade de point, etc. However, the positive results we observed in the detection of ectopic beats make it reasonable to assume that the system could detect also these additional rhythm aberrances, although this characteristic remains to be verified in practice.
Conflict of interest: none declared.



