-
PDF
- Split View
-
Views
-
Cite
Cite
M. Guenther, S. Kolschmann, T.P. Rauwolf, M. Christoph, V. Sandfort, R.H. Strasser, C. Wunderlich, Implantable cardioverter defibrillator lead implantation in patients with a persistent left superior vena cava—feasibility, chances, and limitations: representative cases in adults, EP Europace, Volume 15, Issue 2, February 2013, Pages 273–277, https://doi.org/10.1093/europace/eus287
Close - Share Icon Share
Abstract
Device implantation may be challenging in patients with venous abnormalities. The most common congenital variation—frequently associated with other congenital abnormalities—is described as persistent left superior vena cava (PLSVC).
The present case series demonstrates successful implantable cardioverter defibrillator (ICD) lead implantation in the most common anatomic variations of PLSVC. All types of current ICD models (single and dual chamber, VDD, and cardiac resynchronization therapy devices) were used. Angiographic findings and implantation techniques (e.g. guiding and diagnostic catheters, wires, occlusion balloons, and rotation sequences) are presented in images and movie sequences.
Device implantation in patients with PLSVC may be complex but a successful transvenous approach is possible in most of the cases. Careful imaging prior to implantation procedure is essential for understanding the individual anatomy and in order to choose adequate material and implantation strategy.
Introduction
Implantation of pacemaker and implantable cardioverter defibrillator (ICD) leads can be challenging due to congenital anomalies of the systemic superior veins. This includes the presence of a persistent left superior vena cava (PLSVC) with (double venous system) or without (single left superior vena cava) a right-sided venous vessel. In the double venous system-situation a superior cross connection via an innominate vein between left and right superior caval veins is facultative. Persistent left superior vena cava is a rare venous abnormality in healthy adults (0.3–1%), but it has a 10-fold higher incidence with congenital heart disease.1,2
In most of the cases drainage of venous blood of the left upper part of the body and the left arm is guaranteed via subclavian and jugular vein, PLSVC, and coronary sinus (CS) to the right atrium. This compensated situation is clinically asymptomatic and is often discovered incidentally under central venous catheterization or pacemaker implantation.
Embryological background
During normal embryonic development, the anterior cardinal veins (drain head, neck, and arm) fuse with the posterior cardinal vein in an early stage.3 They reach the heart as the right and left parts of the coronary sinus.
Most of the left-sided cardinal system disappears, leaving only the CS itself and a remnant known as the ligament of Marshall. Failure of obliteration of the left anterior cardinal vein results in the presence of PLSVC.4 The most common anatomic variations are presented in Figure 1, right side. A rare, but clinical important variation, is a PLSVC draining directly into the left atrium (LA). In combination with an unroofed CS and atrial septal defect this situation is referred as Raghib-Complex5 (Figure 1, left side and movie 1).
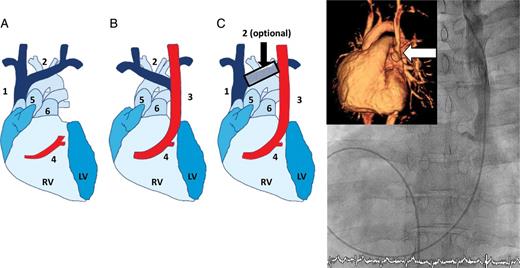
(Right side) (modified from Schreve-Steensma et al.4). Schematic overview of upper venous variations. (A) Normal situation. (B) Single left superior vena cava. (C) Double superior vena cava with or without a cross-connection. 1 = right superior vena cava, 2 = Innominate vein, 3 = left superior vena cava, 4 = coronary sinus, 5 = aorta, 5 = main pulmonary artery, RV = right ventricle, LV = left ventricle. (Left side) Venous angiogram of persistent left superior vena cava entering directly into the left atrium. Inserted image: three-dimensional magnetic resonance imaging (persistent left superior vena cava entry into the left atrium marked with arrow).
Methods
Transvenous implantation of devices and leads may be difficult in patients with unexpected PLSVC, notably in these patients, who had no prior imaging of the anatomic structures and their relations. Especially, venous flaps, atypical confluence with the CS, or unfavourable geometry of CS ostium may generate challenging situations during implantation procedures. In various situations special materials (straight and hand-shaped stylet kits, safe sheets, angiography catheters in different curves, and steerable catheters) will be needed to achieve a successful implantation.
Nevertheless, successful access via PLSVC to right atrium (RA) and ventricle as well as CS is reported.6–10
Here we report a first small series of adult patients with successful implantation strategies via PLSVC in single and dual ICD's, VDD-ICD and cardiac resynchronization therapy (CRT)-ICD.
Results
Single chamber implantable cardioverter defibrillator implantation, double venous situation
Case presentation
A 29-year-old female patient suffered from an magnetic resonance imaging (MRI)-trusted non-compaction-cardiomyopathy with syncope and severely decreased left ventricular function (LVEF 25%). Previous cardiac surgery (correction of an aortic coarctation) in early childhood and an Ullrich-Turner-syndrome (XO genotype) was known. Implantable cardioverter defibrillator implantation was planned for the prevention of sudden cardiac death.
Implantation procedure
Initially a peripheral venous angiogram was performed. A double upper venous system without a cross connection to the right venous system was evident. A multipurpose catheter (MP) was inserted via left cubital vein [percutaneous puncture with a 18 G safety catheter (Vasofix® safety, B. Braun, Germany) placing a hydrophilic wire (Radifocus® guide wire M, Terumo®, Somerset, USA) in the RA and right ventricle (RV) via Vena brachialis and PLSVC followed by an over-the-wire (OTW) insertion of the MP] for angiogram in right and left anterior oblique projections (RAO 30° and LAO 40°). These fluoroscopy projections are useful to understand the three-dimensional (3D) geometry between CS-ostium, tricuspidal valve level, and right ventricular apex. Subsequently followed the subclavian vein puncture and implantation of a single coil shock lead (Endotak Reliance, Boston Scientific, Natick, USA) parallel to the preliminarily inserted MP catheter, which was used as a ‘guide post’. This implantation technique alongside the previous inserted MP catheter was suitable to place the lead without any additionally use of contrast agent and reduces the radiation time to lower than 2min at all. Access to the RV was gained by using a hand-shaped stylet and first advancing the lead towards the lateral wall of the RA and then subsequently with the tip of the lead pointing to the atrium into the RV. After fixation of the screw-in-lead with good electrical values a typical ‘figure of alpha (α)’ of the lead in RA and RV was installed (RAO and PA-projections) (Figure 2 and movie 2).
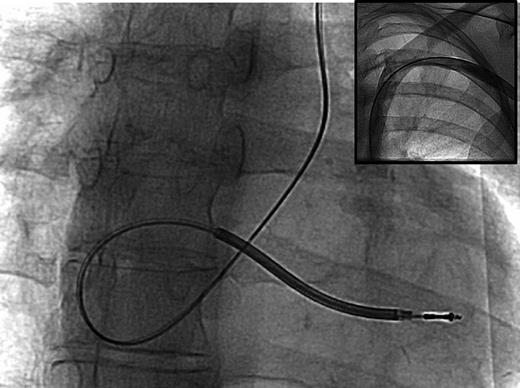
Alpha configuration in conventional chest X-ray (enlarged detail), and venous angiogram without cross branch to the right-sided upper veins (small inserted image).
VDD-implantable cardioverter defibrillator implantation, persistent left superior vena cava, and absence of right vena cava
Case presentation
A 52-year-old female patient was referred for device implantation 14 days after cardiac surgery (aortic valve replacement due to severe aortic regurgitation and bicuspid valve). After cardiac surgery a persistent total atrioventricular block and multiple episodes of ventricular fibrillation without any evidence for myocardial ischaemia were documented (LVEF 45%).
Implantation procedure
Initially a venous angiography with injection of contrast agent via left and right V. cubitalis was performed. It showed an anatomical variation with PLSVC and absence of the right superior vena cava. Thus, all venous blood from the upper part of the body was drained by PLSVC. A screw-in VDD single-coil ICD lead (Linux 65/17, Biotronik, Berlin, Germany) was inserted into the right ventricular apex. The implantation technique was similar as described in case 1 except that we were not using an MP catheter as a guide post. In this situation it is much more easy to pass the tricuspid valve level, because there is no right-sided vena cava entering the RA as a second ‘exit’ for the ICD lead. Right ventricular lead measurements showed acceptable values, atrial signals were detected alongside the whole coronary sinus. Best atrial sensing was achieved in typical α-position of the lead as shown in Figure 3 and movie 3.

Alpha configuration of VDD-implantable cardioverter defibrillator lead implanted via persistent left superior vena cava. Inserted images: (a) venous situation at left side. (b) venous situation at the right side. (c) the floating right atrium sensing dipole is placed near the anterior wall of right atrium in lateral projection.
Dual-chamber implantable cardioverter defibrillator, double venous system, persistent left superior vena cava as an exit strategy by a coexisting total thrombotic occlusion of right-sided brachiocephalic trunk
Case presentation
A 71-year-old male patient suffered from non-compaction-cardiomyopathy (LVEF 35%, paroxysmal atrial fibrillation, previous successfully cardiopulmonary resuscitation due to ventricular fibrillation). The patient was admitted for lead revision of a dual-chamber ICD because the RV shock lead showed insulation failure of the P/S part. Electric values of the shock part were found correct. Under the initial implantation via right vena cava no noticeable problems were reported.
Implantation procedure
At first the preparation of the device and leads was performed followed by subclavian vein puncture. Fluoroscopy showed an unexpected course of the inserted wire consistent with the presence of a PLSVC. Venous angiogram demonstrated a thrombotic occlusion of the brachiocephalic trunk near the confluence with the right venous vessels, which was most likely to be lead associated (Figure 4). A dilated PLSVC with side connections to the CS was obvious; however, a typical common ostium entering the RA was not present. This may be a specific characteristic of secondary dilated PLSVC due to contralateral thrombotic occlusion. An extended angiography using a Judkins right coronary catheter (5 F JR 3.5) was performed and an hydrophilic percutaneous coronary intervention (PCI) wire (Pilot 50®, Abbott, Abbott park, IL, USA) was inserted in a suitable target vessel via this catheter. Finally a small venous cross connection was used for insertion of an OTW P/S lead (Easytrak 2, Boston Scientific, Natick, USA) via a septal vein near the right apex. Electrical measures were acceptable (threshold: 1.2/0.5 V/ms, sensing 12 mV, impedance 642 Ω) and defibrillation threshold testing test was successful in sensing and defibrillation.
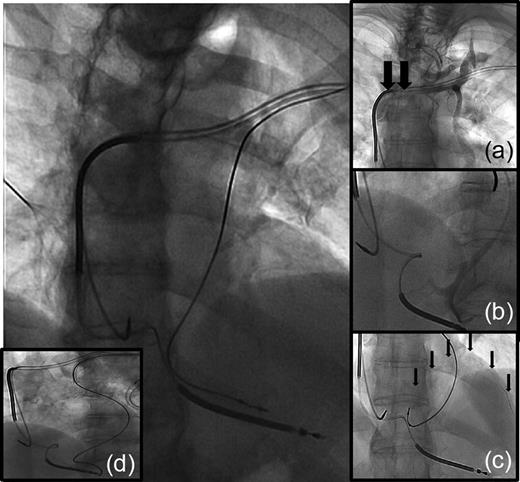
P/S lead via persistent left superior vena cava placed in a septal vein near the right ventricular apex. Inserted images: (a) venous situation demonstrates total occlusion (arrows) near the distal shock coil in the left brachiocephalic vein. (b) selective angiogram of distal veins (coronary sinus and side branches). (c) tip of guide wire in a posterolateral vein via origin coronary sinus, passage of coronary sinus into the target vessel was not possible with the over-the-wire lead. (d) over-the-wire implantation of the lead into a small septal vein, left anterior oblique projection confirm septal location of the lead tip.
Cardiac resynchronization therapy–implantable cardioverter defibrillator, double venous system, persistent left superior vena cava as an access to posterolateral coronary sinus vein
Case presentation
A 71-year-old male patient with ischaemic cardiomyopathy (LVEF 20%) and previous implanted, right-sided dual-chamber pacemaker was scheduled for CRT-ICD upgrade after an unsuccessful implantation attempt in a nearby hospital. First implantation procedure was aborted due to an unexpected PLSVC with widely dilated CS.
Implantation procedure
Initially preparation of the device and leads was performed followed by subclavian vein puncture. A guiding catheter was advanced into PLSVC. The following venous angiogram was insufficient in contrast to identify the confluence of CS and PLSVC. This phenomenon was caused by wash out effect of the contrast agent due to the enormous venous blood flow in the PLSVC. A cubital vein puncture at the left arm was performed and a Guide wire (Radifocus®, Terumo®, Somerset, USA) was inserted into the PLSVC. An OTW balloon catheter (Balloon Wedge Pressure Catheter®, Arrow®, Kington, UK) was positioned into the superior part of PLSVC to suppress venous blood flow at the time of angiography. In this setting the ostium of CS was successfully identified, angiogram was stored in LAO and RAO projection (road map) and CS was explored with selective angiography with an internal mammary artery coronary diagnostic catheter. This catheter was used to place a PCI wire (Boston Scientific, Natick, USA, PT 2, heavy support) into a suitable vein and an OTW-lead (Easytrak 2, Boston Scientific, Natick, USA) was inserted (Figure 5).
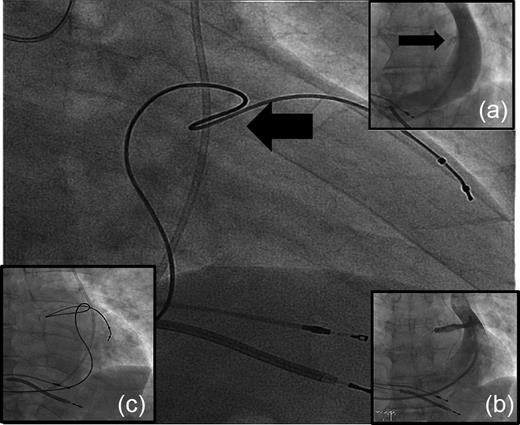
Cardiac resynchronization therapy–implantable cardioverter defibrillator via persistent left superior vena cava, right-sided approach due to an upgrade of a previously implanted dual-chamber pacemaker system. Inserted images: (a) venous angiogram of persistent left superior vena cava, flow-rate in this dilated persistent left superior vena cava was minimized using an occlusion balloon (balloon not shown), inserted via left cubital vein, to achieve an acceptable contrast. (b) selective angiogram of coronary sinus entrance into persistent left superior vena cava. (c) left anterior oblique projection confirms a posterolateral location of lead tip.
Discussion
In patients with PLSVC implantation of pacemaker and ICD leads may be difficult due to unfavourable anatomy and limited suitable materials with conventional methods (leads, sheets, and catheters). Nevertheless, successful implantations of pacemakers, ICD's, and CRT's are reported.1,6,7,11 With an estimated frequency of 0.3–1.0% in healthy adults and 10-fold higher incidence in patients with congenital structural anomalies operators with a high implantation frequency will be repetitively confronted with this problem.
Essential for successful procedures is the understanding of the underlying 3D anatomy in echocardiography12 and multi-plane fluoroscopy.6,7 Previous information of the individual anatomy and imaging (CT and MRI) is helpful for planning the procedure and for choosing the most suitable material. Particularly the passage of the tricuspid valve incoming from the common ostium of CS and PLSVC for implantation of right ventricular pacing leads can be difficult and the variable anatomy (angle and venous flaps) must have been thoroughly examined. In this respect multi-plane fluoroscopy equipment is fundamental.
Furthermore a pre-procedural venous angiography may be useful and should be discussed in patients with increased risk for venous anomalies before starting with invasive procedures. The current guidelines for cardiac pacing13,14 do not require a venous angiogram, but it is quite helpful in these special cases. Anyhow, in the authors' point of view routine use of a venous angiogram in all pacemaker or ICD patients is not justified because of the low incidence of relevant venous abnormalities and possible side effects of the contrast agent.
The drainage of a PLSVC directly into the LA is a rare variation. Nevertheless, this situation carries important clinical implications because of the risk of systemic embolism and should therefore be ruled out before implantation. This can easily be done by echocardiography combined with application of ultrasound contrast agent via both left and right cubital vein.
A challenge is the implantation of CRT systems via PLSVC.6,9,15 In the presence of a right superior vena cava with adequate diameter a right-sided approach seems to be more promising. The sticking point in this procedure is to localize the entrance of the native CS. A venous angiogram may be not sufficient in all cases. One might encounter high flow in the PLSCV and ‘wash out phenomenon’ can avert an adequate quality of angiogram. In these cases an alternative imaging (MRI and CT) or a supported angiogram (blocking catheters or diagnostic coronary catheters) may be useful. Another attractive alternative for detecting target vessels for left ventricular lead implantation is the visualization of cardiac veins after left main angiogram. For insertion of the CS lead a guiding system with atypical curves or steerable catheters may support a successful procedure. In patients with PLSVC-only situation (absence of right-sided upper veins) a successful implantation of CRT (RV lead in α-formation, RA lead, and CS lead) is given only in exceptional cases because of interference of sheets and leads in the PLSVC. In this situation a VDD-ICD-lead for right ventricular pacing, atrial sensing and shock function can help to minimize lead interferences. Nevertheless, in these rare cases, a primary surgical approach should be considered.
Special anatomy should be expected in patients with ‘revascularized’ and secondary dilated PLSVC associated with thrombotic occlusions of right-sided large upper veins. In these individual cases extensive imaging is necessary to understand the complex venous anatomy. A common ostium entering the RA is not imperative and the drainage via small bypass veins is possible and variable. Lead implantation in these small vessels must be an individual decision.
Conclusion
Summarizing the presented variations of lead implantation via PLSVC this approach seems to be successful in experienced centres with high implantation frequency. Careful imaging before implantation is essential for the understanding of the individual anatomy and in order to choose adequate material and implantation strategy.
Acknowledgements
None.
Conflict of interest: none declared.
References
Author notes
Both authors contributed equally.



