-
PDF
- Split View
-
Views
-
Cite
Cite
A. John Camm, Seah Nisam, European utilization of the implantable defibrillator: has 10 years changed the ‘enigma’?, EP Europace, Volume 12, Issue 8, August 2010, Pages 1063–1069, https://doi.org/10.1093/europace/euq282
Close - Share Icon Share
Abstract
The correct rate of implantation for implantable cardioverter defibrillator (ICD) and CRT-D devices is not known, but practice surveys suggest persistent under-utilization of these treatments on both sides of the Atlantic. Although recent clinical trial results and the implementation of current guidelines appear to have encouraged a growth of the rate of implantation in most countries, there remains a remarkable trans- Atlantic difference which has not changed much for more than 10 years. For every European ICD implant, there are four implants in the USA after adjustment for the size of the populations. Since very large variations in the implantation rates also occur between and within European Countries, an opportunity is afforded to explore the possible cause of these differences. It seems very unlikely to be explained simply by guideline discrepancies, financial constraints, or differences in disease prevalence. Instead, it is more likely to be attributable to a relative paucity of electrophysiologists, and their associated resources. In turn, the failure to establish effective educational programmes, screening, and referral pathways contributes to far fewer patients. It seems unlikely that adequate equity of access to this potentially lifesaving treatment will be provided until adequate registries, audits, and gap analyses are undertaken throughout Europe.
Introduction
Official mortality census reports have shown that sudden cardiac death (SCD) claims ∼450 000 victims annually in the USA. 1 While no official statistics are reported in Europe, the very similar cardiovascular risk profile of Western Europeans 2 implies that the SCD number must be similar. Thus, SCD is responsible for more deaths than cancers, stroke, and AIDS combined. 1 , 3–5 Since the implantable cardioverter defibrillators (ICDs) have proven to be the most effective therapy to combat SCD, its acceptance has increased rapidly after its introduction in 1980. 6
Nearly a decade ago, we reported on the remarkable disparity in ICD utilization between Europe and the USA. 7 ‘Remarkable’, because we found no other well-established medical therapy, where the gaps in clinical implementation differed so significantly between the two continents. Our earlier article speculated in some detail on the possible explanations, and guideline difference was identified as one of the reasons. In 2006, the cardiological societies in Europe and the USA agreed for the first time on a common set of guidelines for the management of patients with ventricular arrhythmias and the prevention of SCD. 8 Recently, the ACC/AHA and HRS, on the one hand, and the ESC and EHRA, on the other hand, have updated their device guidelines. 9–11 Thus, as the past decade has substantially solidified the already strong evidence base, culminating in general agreement on the guidelines, we thought it would be useful to re-examine the implementation question, and see how it has evolved in these past 10 years.
Implantable cardioverter defibrillator utilization
There has certainly been an uptake in acceptance of ICD therapy, as is evident from Figure 1 . Even though the US implant rate for ICD/CRT-D has slowed in 2006–07, it is currently approximately four times that in Europe, compared with approximately five times, in our analysis 10 years ago. The implant rates for the ICD (with or without cardiac resynchronization pacing—CRT-D) have increased in all the Western European countries ( Figure 2 ), reaching an average of ∼155 per million population in 2007; and, clearly, the trend is still upwards. 12 However, there is also a great variation between different European countries. Taking statistics from the four largest European countries—Italy, France, Germany, and the UK—it is evident ( Figure 3 ) that there is also great inhomogeneity between different regions in the same country (A. Proclemer et al ., personal communication; H. Lorenz, personal communication; D. Cunningham, personal communication; E. Aliot, personal communication).
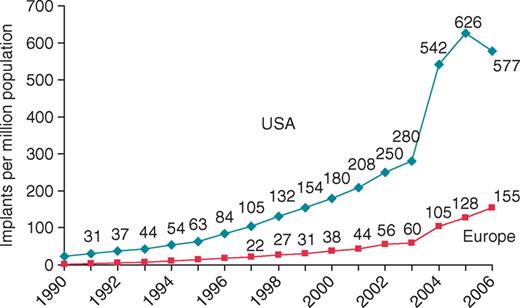
Implantable cardioverter defibrillator/CRT-D implantations per million of the population in Europe and the USA from 1990 to 2006.
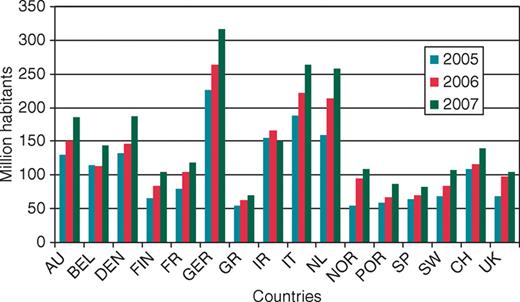
Implantable cardioverter defibrillator and CRT-D European implant rates per million inhabitants between 2005 and 2007 inclusive. (Ireland data reported separately from the UK.) The data are kindly provided by EUCOMED 12 .
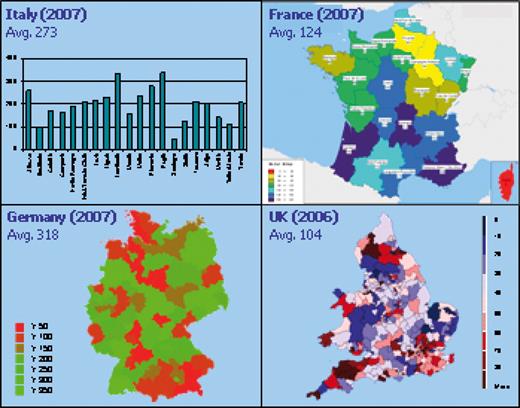
Implantable cardioverter defibrillator/CRT-D implant rates (per million population). The data were kindly supplied by: Italy: A. Proclemer; France: E. Aliot; Germany: H. Lorenz, Medtronic, Germany; U.K.: D. Cunningham. The graphs represent the regional implant rates for 2007 for Italy, France, and Germany, but for 2006, for the UK. The 2007 averages for the four countries are the EUCOMED 2008 numbers, which vary slightly from the data reported by the physicians indicated above. For the UK, the map represents 2006 data, but the country average (104) is for 2007.
In trying to understand these differences in implant rates, it is important to examine the number of patients deemed by guidelines to be appropriate for ICD implantation. McComb and colleagues 13 (Newcastle, UK) audited patient records against the recommendations for ICD implantation made by the National Institute for Clinical Excellence (NICE) in order to determine whether the patients fulfilled the criteria for ICD implantation; and they repeated the audit with the same patient records against the MADIT-II selection criteria. Approximately 190 patients/million (annual incidence plus ‘prevalence’) fulfilled the NICE national guidelines for ICD implantation; and ∼800/million satisfied the MADIT-II criteria. In a similarly conducted audit in the Netherlands, Borleffs et al . 14 found that 510 patients per million population per year met the 2005 Dutch guidelines. 14 It should be noted that, even in the USA, where ICD therapy acceptance is the highest, there appears to be at least 50% under-utilization, as we reported several years ago 15 and which was confirmed by the analysis reported by Hernandez et al.16 just 1 year ago. Our US estimate of appropriate ICD candidates—excluding patients with co-morbidities and aged over 79 years—was 833 patients/million, hence similar to the UK and Dutch estimates.
Figure 4 , taken from an analysis conducted by Guidant UK Ltd 17 in 2005, shows that only ∼8% of patients fitting specific randomized ICD trial criteria actually received ICDs in Western Europe through 2005. These figures do not include patients with contraindications for age or for generally poor prognosis due to high co-morbidity from other diseases, and every effort was made to avoid double counting, for patients fitting overlapping indications. From this analysis, it is clear that only a few years ago, less than 1 in 10 ‘ICD-indicated’ patients actually received ICDs in Western Europe. These data, together with the country data presented above, are in line with recent assessments from two independent financial consultant companies, 18 , 19 all basically supporting the notion that the annual incidence of appropriate ICD candidates should be somewhere in the range 750–1000 per million population.
![Percentage of patients fulfilling the criteria for the major randomized implantable cardioverter defibrillator (ICD) trials, which actually get implanted with ICDs in Western Europe. The histograms represent the total number of patients (W. Europe), who fulfil the study criteria. [In case of overlapping criteria, the patients are only counted once (the earlier indication); patients with high co-morbidity due to cancer or other diseases have been excluded.] The triangles represent the actual number of patients, corresponding to a given study, who were implanted with ICDs in the years indicated. Analysis from Ref. 17 .](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/europace/12/8/10.1093_europace_euq282/3/m_euq28204.jpeg?Expires=1747862998&Signature=QPKelFG92Mk2J92621yiGc3HWd0PVVywsoAe5Xf8vf6-nlNGao4KiSs1pEP0xMnwZ1rydsGaxikbkD6Bl~mg4eSvDIuUW2GaoE~Updm6TFH3g~4QGEreu2BzKM7hdPcwUd0W12~D9SPOBIBIDznKNQmfDvS6-6XsrhCzGgG1-OWMo0JXlB5OMbY5z3gY9vMtYWuq5AGXAdpGd12kBuoojeTBJVHP7JPcmHNmDvp6z23T1hYFJmdH6pJPXDEeTERJ0NnNXsLKQwg6nULNdsFQOfBF4NuM7gKbI3xmzVfqCnKl~R8Bj5MqW0t2uAGeimihFaq2Y3vFERwWIobi2hUEXQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Percentage of patients fulfilling the criteria for the major randomized implantable cardioverter defibrillator (ICD) trials, which actually get implanted with ICDs in Western Europe. The histograms represent the total number of patients (W. Europe), who fulfil the study criteria. [In case of overlapping criteria, the patients are only counted once (the earlier indication); patients with high co-morbidity due to cancer or other diseases have been excluded.] The triangles represent the actual number of patients, corresponding to a given study, who were implanted with ICDs in the years indicated. Analysis from Ref. 17 .
Why is the implantable cardioverter defibrillator under-utilized?
There are no major differences between the cardiovascular mortality incidence between the European countries and the USA. 20 , 21 This is an important point, as it dispels the argument that the need for ICD therapy, on a patient per million population basis, is different between the two continents. It is useful to re-look at the reasons which were postulated in our earlier article, to examine whether and how the situation has evolved in the intervening 10 years, and discuss still further explanations.
At the end of the 1990s, there were no official European guidelines for the use of ICDs. This situation has evolved significantly, as the first ‘European’ guidelines were published in 2001, 22 followed in 2006 by the first ‘global’ guidelines 8 and the updates of these in the past few months. 9–11 Gradually, most of the Western European countries have officially adopted the ‘global’ guidelines, or developed national guidelines, which are essentially similar. Electrophysiologists and ICD implanting centres on both sides of the ocean, and importantly also heart failure specialists, 11 seem now to be in general agreement on the indications for ICD implantation, although some national guidelines remain unaccountably at odds with the widely endorsed international recommendations. In an interesting recent survey, appointed experts evaluated the patient records on 183 out-of-hospital cardiac arrest survivors in Canada and the USA, determining that 55% of the patients should have received an ICD. 23 In actual practice, adherence in Canada was only 20% lower compared with the USA. Thus, we do not believe that nuance differences between European and American electrophysiologists and their practice even marginally account for the present four-fold difference in implant rates between the USA and Europe.
An extremely important reason for the major ICD utilization difference between continents is because Europe on a per capita basis has a far smaller number of implanting centres and electrophysiologists. In the four major countries, France, Germany, Italy, and UK ( Table 1 ), there is some correlation between ICD implant rate and the number of implanting centres, with high implant rates in Italy and Germany—where there are 4.4 and 6.8 implant centres per million population, respectively; compared to low implant rates in the UK and France—where there are only 0.7 and 1.4 implanting centres, respectively, per million population. An additional factor complicating this situation is the fact that more and more of the electrophysiologists' workload is spent on ablation. Ablation procedures, in particular for atrial fibrillation, have increased ∼36% annually from 2005 to 2007, and a similar further increase is anticipated for the coming few years (F. Pumares, personal communication). Considering the lengthy procedure time for ablation interventions for atrial fibrillation, it has been estimated from a survey undertaken in 20 laboratories in four European countries in 2007 that on average at least 25% of European electrophysiologists' time is now spent on ablation procedures (F. Pumares, personal communication). Obviously, this effort competes with the time of the electrophysiologist and the electrophysiology laboratory that can be made available for ICD/CRT-D implantation. This may be another important contributor to ICD under-utilization in Europe.
Implantable cardioverter defibrillator/CRT-D implantations per million and centres implanting (per million population)
| . | Implants per million . | ICD/CRT-D centres per million . | Index implants per million . | Index ICD/CRT-D centres per million . |
|---|---|---|---|---|
| Germany | 226 | 4.4 | 100 | 65 |
| Italy | 192 | 6.8 | 85 | 100 |
| France | 83 | 1.4 | 37 | 21 |
| UK | 69 | 0.7 | 31 | 10 |
| . | Implants per million . | ICD/CRT-D centres per million . | Index implants per million . | Index ICD/CRT-D centres per million . |
|---|---|---|---|---|
| Germany | 226 | 4.4 | 100 | 65 |
| Italy | 192 | 6.8 | 85 | 100 |
| France | 83 | 1.4 | 37 | 21 |
| UK | 69 | 0.7 | 31 | 10 |
The ICD/CRT-D implant rate in four European countries expressed as implants per million, together with the number of implant centres per million of the population. The right-hand columns are a percentage of the highest figures.
Implantable cardioverter defibrillator/CRT-D implantations per million and centres implanting (per million population)
| . | Implants per million . | ICD/CRT-D centres per million . | Index implants per million . | Index ICD/CRT-D centres per million . |
|---|---|---|---|---|
| Germany | 226 | 4.4 | 100 | 65 |
| Italy | 192 | 6.8 | 85 | 100 |
| France | 83 | 1.4 | 37 | 21 |
| UK | 69 | 0.7 | 31 | 10 |
| . | Implants per million . | ICD/CRT-D centres per million . | Index implants per million . | Index ICD/CRT-D centres per million . |
|---|---|---|---|---|
| Germany | 226 | 4.4 | 100 | 65 |
| Italy | 192 | 6.8 | 85 | 100 |
| France | 83 | 1.4 | 37 | 21 |
| UK | 69 | 0.7 | 31 | 10 |
The ICD/CRT-D implant rate in four European countries expressed as implants per million, together with the number of implant centres per million of the population. The right-hand columns are a percentage of the highest figures.
There are relatively few referrals to the implanting centres. Data supporting this contention emanate from a survey conducted by Boston Scientific which involved 251 heart failure specialists in four countries (Holland, UK, France, and Austria) who screened a total of 2256 patients under their care for a 3-year period ending in July 2008 24 ( Table 2 ). Using the guidelines for ICD implantation based on the major trials, it was established that 41% of the screened patients met the study criteria and were potential candidates for ICD implantation. These heart failure specialists then referred 55% of the indicated patients on to electrophysiology centres for evaluation for ICDs (and 26% of the referred patients were eventually implanted with an ICD). From this large database, heart failure specialists recognized that they were referring only about half of the patients, who met ICD implantation guidelines, on to their electrophysiology colleagues. A recent large registry in Germany reinforces the problem relating to referrals. The ‘Cardiac Resynchronisation under evaluation in daily Therapy’ (CREDIT) Registry, which was carried out in 101 hospitals in Germany, evaluated 3148 patients with NYHA heart failure III/IV or LVEF <0.35, reported that well over 25% of screened patients met the inclusion criteria for COMPANION, MADIT II, or SCD-HeFT. However, only 20% of patients meeting the indications for these studies were referred for device implantation. 25 It is interesting to note that in apparently comparable patients, those who were received device therapy survived far better than those who did not (relative risk reduction 46.9%, P < 0.009).
Patient referrals for implantable cardioverter defibrillators/CRT-Ds by HF physicians
| Country a . | Physicians using HF-radar (cumulative) . | Screened patients (cumulative) . | Indicated b patients (cumulative) . | Referred c patients (cumulative) . | Implanted c patients (cumulative) . | Indicated/screened (%) . | Referred/indicated (%) . | Implanted indicated (%) . |
|---|---|---|---|---|---|---|---|---|
| The Netherlands | 57 | 947 | 432 | 235 | 105 | 46 | 54 | 24 |
| Austria | 16 | 496 | 233 | 92 | 58 | 47 | 39 | 25 |
| UK | 35 | 414 | 102 | 39 | 25 | 25 | 38 | 25 |
| France | 143 | 399 | 150 | 136 | 47 | 38 | 91 | 31 |
| Italy | 53 | 204 | 81 | 15 | 2 | 40 | 19 | 2 |
| Total | 304 | 2460 | 998 | 517 | 237 | 41 | 52 | 24 |
| Country a . | Physicians using HF-radar (cumulative) . | Screened patients (cumulative) . | Indicated b patients (cumulative) . | Referred c patients (cumulative) . | Implanted c patients (cumulative) . | Indicated/screened (%) . | Referred/indicated (%) . | Implanted indicated (%) . |
|---|---|---|---|---|---|---|---|---|
| The Netherlands | 57 | 947 | 432 | 235 | 105 | 46 | 54 | 24 |
| Austria | 16 | 496 | 233 | 92 | 58 | 47 | 39 | 25 |
| UK | 35 | 414 | 102 | 39 | 25 | 25 | 38 | 25 |
| France | 143 | 399 | 150 | 136 | 47 | 38 | 91 | 31 |
| Italy | 53 | 204 | 81 | 15 | 2 | 40 | 19 | 2 |
| Total | 304 | 2460 | 998 | 517 | 237 | 41 | 52 | 24 |
a Only countries with relevant numbers of screened patients are mentioned and used for the statistics.
b Guidelines used for the screening: Heart Failure ESC Guidelines 2005, ACC/AHA/ESC Sudden Cardiac Death Guidelines 2006, ESC/EHRA Pacemaker/CRT Guidelines 2007.
c The number of referred and implanted patients can be under-evaluated as they indicate the number of patients reported by physicians through HF-radar. 24
Patient referrals for implantable cardioverter defibrillators/CRT-Ds by HF physicians
| Country a . | Physicians using HF-radar (cumulative) . | Screened patients (cumulative) . | Indicated b patients (cumulative) . | Referred c patients (cumulative) . | Implanted c patients (cumulative) . | Indicated/screened (%) . | Referred/indicated (%) . | Implanted indicated (%) . |
|---|---|---|---|---|---|---|---|---|
| The Netherlands | 57 | 947 | 432 | 235 | 105 | 46 | 54 | 24 |
| Austria | 16 | 496 | 233 | 92 | 58 | 47 | 39 | 25 |
| UK | 35 | 414 | 102 | 39 | 25 | 25 | 38 | 25 |
| France | 143 | 399 | 150 | 136 | 47 | 38 | 91 | 31 |
| Italy | 53 | 204 | 81 | 15 | 2 | 40 | 19 | 2 |
| Total | 304 | 2460 | 998 | 517 | 237 | 41 | 52 | 24 |
| Country a . | Physicians using HF-radar (cumulative) . | Screened patients (cumulative) . | Indicated b patients (cumulative) . | Referred c patients (cumulative) . | Implanted c patients (cumulative) . | Indicated/screened (%) . | Referred/indicated (%) . | Implanted indicated (%) . |
|---|---|---|---|---|---|---|---|---|
| The Netherlands | 57 | 947 | 432 | 235 | 105 | 46 | 54 | 24 |
| Austria | 16 | 496 | 233 | 92 | 58 | 47 | 39 | 25 |
| UK | 35 | 414 | 102 | 39 | 25 | 25 | 38 | 25 |
| France | 143 | 399 | 150 | 136 | 47 | 38 | 91 | 31 |
| Italy | 53 | 204 | 81 | 15 | 2 | 40 | 19 | 2 |
| Total | 304 | 2460 | 998 | 517 | 237 | 41 | 52 | 24 |
a Only countries with relevant numbers of screened patients are mentioned and used for the statistics.
b Guidelines used for the screening: Heart Failure ESC Guidelines 2005, ACC/AHA/ESC Sudden Cardiac Death Guidelines 2006, ESC/EHRA Pacemaker/CRT Guidelines 2007.
c The number of referred and implanted patients can be under-evaluated as they indicate the number of patients reported by physicians through HF-radar. 24
Physicians are not always aware of the effectiveness of ICD treatment in those at risk of SCD. To evaluate this question, EUCOMED conducted a survey of 250 general cardiologists and heart failure specialists (not including device implanters) at ESC and European HF congresses in 2005–06. 26 The results showed that (i) somewhere between 25 and 65% of physicians were not aware of the major ICD studies and guidelines; (ii) about half were not aware that the device-based guidelines had been updated as a result of these studies. Similarly, a US survey conducted in 2007 responded to by 331 primary care physicians, concluded that ‘…only a very small minority of primary care physicians are aware of ICD referral guidelines.’ 27
There are financial considerations relating to ICD cost-effectiveness. Saunders et al.28 made an extensive analysis of the cost-effectiveness of ICD (and CRT-D), for the landmark randomized ICD trials, which ranged from $25 000 to $50 000 per life year saved ( Table 3 ). There is a very wide range of estimates of the cost–utility of ICD and CRT-D therapy with sensitivity analyses that exceed or are contained within acceptable cost levels. A recent analysis of incremental cost–utility compared CRT-D with CRT, which concluded that the ICD component of therapy was unaffordable, may be subject to methodological faults reminiscent of similar comparisons between single and dual chamber pacing devices. What matters is the cost–utility of individual therapies rather than potentially artificial differences between two possible treatments based on a single trial. Analyses with lifetime horizons generally show convincingly that ICD therapy is affordable by western health care purchasers. It is inconceivable that this should be the major reason for transatlantic differences in ICD utilization, especially when such differences do not exist with other expensive therapies.
Implantable cardioverter defibrillator (and CRT-D) cost-effectiveness (dollars per life-year saved), for the major randomized implantable cardioverter defibrillator studies
| ICD (and CRT-D) cost-effectiveness | |
| MADIT | $25 000 |
| MUSTT | $24 500 |
| MADIT II | $39 000 |
| DEFINITE | $36 800 |
| COMPANION (CRT-D) | $36 500 |
| SCD-HeFT | $50 700 |
| ICD (and CRT-D) cost-effectiveness | |
| MADIT | $25 000 |
| MUSTT | $24 500 |
| MADIT II | $39 000 |
| DEFINITE | $36 800 |
| COMPANION (CRT-D) | $36 500 |
| SCD-HeFT | $50 700 |
Adapted from Ref. 28 .
Implantable cardioverter defibrillator (and CRT-D) cost-effectiveness (dollars per life-year saved), for the major randomized implantable cardioverter defibrillator studies
| ICD (and CRT-D) cost-effectiveness | |
| MADIT | $25 000 |
| MUSTT | $24 500 |
| MADIT II | $39 000 |
| DEFINITE | $36 800 |
| COMPANION (CRT-D) | $36 500 |
| SCD-HeFT | $50 700 |
| ICD (and CRT-D) cost-effectiveness | |
| MADIT | $25 000 |
| MUSTT | $24 500 |
| MADIT II | $39 000 |
| DEFINITE | $36 800 |
| COMPANION (CRT-D) | $36 500 |
| SCD-HeFT | $50 700 |
Adapted from Ref. 28 .
Implantable cardioverter defibrillators for primary prevention are a relatively recent innovation. There are major differences in the use of ICDs for primary prevention, i.e. for patients without a previous history of sustained, symptomatic VT/VF, between the European countries and the USA. Thus in 2005, 82% of ICDs implanted in the USA were for primary prevention indications, whereas the corresponding figure in Italy was 36% although this did rise to 54% by 2007. 29 Similar figures from Belgium indicate that only 10% of ICDs were implanted for primary prevention purposes in 2005, which increased to ∼41% by early 2008. 30 Even if the trends are increasing in recent years, it is clear that the under-utilization of ICDs for primary prevention, as depicted in Figure 4 , leaves much to do. This observation specific to primary prevention use of ICDs may well be related to the patient referrals issue discussed above. There is little ‘referral issue’ when a patient is resuscitated from an out-of-hospital cardiac arrest or symptomatic VT—when appropriate such patients are likely to receive an ICD in Europe as in the USA. In contrast, patients identifiable only on the basis of history, left ventricular ejection fraction, and other risk factors, but without a previous VT/VF history, should be proactively screened and referred to electrophysiologists to determine their appropriateness for ICD implantation. The most recent European and global guidelines have unequivocally placed most primary prevention patients in a Class I recommendation category. Similarly, the requirement for primary prevention ICD (CRT-D) therapy has been emphasized in the recent European Society of Cardiology Heart Failure Guidelines where simple and straightforward patient care pathways have been set out. 11
Discussion
In this re-examination of ICD utilization in Europe, it is clear that the evidence-base (published, randomized, prospective studies), as well as the guidelines emanating from these studies, are significantly more complete and robust, compared with when we made our original analysis 10 years ago. Without question, ICD utilization in Europe is increasing compared with the implantation rate reported earlier. Nevertheless, there appears to be an even larger (and growing) divergence in device use, not only compared with the USA., but more importantly, in relation to the guidelines endorsed by the leaders in European cardiology.
A question pertinent to this issue is whether the populations enrolled in the studies and their results correspond to the ‘real world’, and several registries have demonstrated that there is indeed coherence. 31 , 32 Stein et al.31 reported very similar event rates in patients receiving ICDs for primary and secondary prevention indications. In the European SEARCH-MI registry, Santini et al . 32 reported that ‘routine clinical practice in European patients can replicate the results of therapeutic interventions observed in more selected MADIT-II trial populations’. At 1 year, 21% of patients in the registry had an arrhythmic event appropriately terminated, compared with 17% of patients from the MADIT-II study. At 2 years, the results were similar, with 31% of SEARCH-MI patients and 27% of the MADIT-II patients having had an arrhythmic event terminated by the ICD. Overall mortality or SCD was comparable at 1 and 2 years.
We have emphasized that much of the under-utilization problem is related to three factors: shortage of electrophysiologists, poorly developed local referral strategies and care pathways, and difficult or confusing financial circumstances. Concerning the number of electrophysiologists, exact figures are simply unknown in Europe, but it is nowhere near the ∼2300 electrophysiology specialists practicing in the USA, a continent with approximately half as many potential patients as Europe. Thus, there are too few electrophysiologists to deal with the European patients—especially as these same physicians are spending an increasing percentage of their limited time undertaking ablation procedures. As a result, the patients are not actively ‘sought’, particularly since many electrophysiologists would also have an up-hill struggle persuading their hospitals/Trusts that more ICDs are needed.
In some locales where the electrophysiology specialty is well developed, electrophysiologists develop strong local referral patterns and there is a high rate of implantation. There are some obvious examples in the UK, but it is probable that this situation is similar in any jurisdiction, as highlighted by the huge heterogeneity of device use ( Figure 3 ) in major European countries. As funding and reimbursement are fundamentally the same within any given country, these large variations within the same country provide further manifest evidence of differences in physician acceptance of device therapy and the extent to which local services have been developed.
Unlike in the USA, in Europe neither the patients nor their relatives and friends are usually well informed about medical opportunities or are particularly active in seeking out appropriate and expert care. Direct to the consumer advertising of medical services and products is either forbidden or not considered appropriate. Latterly, support groups for patient and carers and organizations that take a special and enthusiastic interest in the causes of life-threatening arrhythmias, cardiomyopathies, channelopathies, and other cardiac arrhythmias are just beginning to emerge in Europe. However, neither the socialized medical systems nor the average patient in Europe is likely to fund these organizations to the extent that will be necessary to achieve a real impact on patient (and physician) education. Organizations such as the Arrhythmia Alliance 33 that seek to enrol all stakeholders in arrhythmia, SCD, pacemakers and defibrillators, etc. are more likely to be effective. The ability of such organizations to bring doctors, nurses, physiologists, technicians, patients, carers, support groups, health care payers, health care managers, and government officials together with industry is likely to pay huge dividends in terms of the improvement of the care of patients with cardiac arrhythmias.
Starting in 2006, the USA developed a national [Only pertains to Medicare primary prevention although 76% of hospitals are including all of their patients (Medicare, non-Medicare, secondary and primary prevention.], compulsory (hospitals can be audited and risk Medicare fraud if compliance on registration of the device implantation is not adhered to), financially compelling (in that payment is withheld pending registration of the device implantation) database for ICD registration. This national registry will yield considerable benefit to the administration of healthcare in the USA by providing oversight of ICD and CRT-D implantation. Using this scheme, it will be possible to identify areas with high- and low-implantation rates and to assess those diagnoses and patient groups for which ICD therapy is being under- or over-used. A longitudinal component to this registry is proposed, but is not yet funded, which will also improve patient management. In Europe, there is no such registry on a similar scale and none is ‘compulsory’. Some countries, for example the UK, have a voluntary registry, the data from which is to be used by health care professionals and administrators to identify the cases and rectify the causes of inequity of ICD utilization and initiate corrective action. The Netherlands is in the process of establishing a Registry, which will include examining whether Dutch patients are treated in accordance with the recent guidelines (M. Schalij, personal communication). The registry includes all baseline parameters (including indication, LVEF, etc.). Furthermore, the registry includes long-term follow-up. A more determined and widespread implementation of such schemes should be strongly encouraged.
At last, Europe has comprehensive and valuable guidelines relating to device implantation in those at risk of life-threatening ventricular arrhythmias. Theoretically, these guidelines have been endorsed by the National Societies of almost every European country. The guidelines have been written by expert cardiologists, who by their experience and understanding of the literature and the evidence base, can make very important contributions to the framing of recommendations. However, the resulting guidelines may be criticized because they are written only by those with potential vested interests, i.e. physicians. It is essential that all stakeholders concerned with ICD therapy are involved in guideline production such that all accept responsibly for the end-product and its implementation. This is particularly true for health care payers who must accept ownership of such guidelines if they are to have any binding effect on the provision of healthcare. The failure of the medical community to adhere to this fundamental rule weakens the guidelines and their impact.
Conclusion
The implementation of global guidelines for ICD/CRT-D therapy remains substantially less in Europe than in the USA. This cannot be explained simply by better economic funding in the USA since European countries of similar economic standing fail to implant these devices on a similar scale. Setting aside the large gap between USA and European ICD/CRT-D implant rates, it is still necessary to explain why different countries within Europe utilize ICD therapy so differently. Although economic factors obviously play a substantial role, they cannot possibly explain the great implant variation which is seen within European countries.
As is the case with pacemaker implantation in the past, the main drivers for adequate guideline implementation appear to be the number of electrophysiologists and electrophysiology centres, referrals for device implantation and investment in specialist health care.
Conflict of interest: A.J.C. is an advisor and speaker for Biotronik, Boston Scientific, and Medtronic. S.N. is an employee of Boston Scientific.
References
Author notes
Professor Camm is British Heart Foundation Professor of Clinical Cardiology.



