-
PDF
- Split View
-
Views
-
Cite
Cite
Patrice Carroz, Dominique Delay, Grégoire Girod, Pseudo-pacemaker syndrome in a young woman with first-degree atrio-ventricular block, EP Europace, Volume 12, Issue 4, April 2010, Pages 594–596, https://doi.org/10.1093/europace/eup373
Close - Share Icon Share
Abstract
First-degree atrio-ventricular (AV) block is defined as a PR interval longer than 200 ms. If too long, it can become clinically relevant and may mimic a pacemaker syndrome. We report the case of a young woman with a long PR interval, probably congenital, with episodes of syncope and dizziness since childhood. Pseudo-pacemaker syndrome is rare and is a Class IIa recommendation for a pacemaker implantation. A dual-chamber pacemaker was implanted and short AV delay was programmed, with rapid clinical improvement.
Introduction
First-degree atrio-ventricular (AV) block is defined as a delay in transmission of an impulse from the atria to the ventricles resulting in a PR interval longer than 200 ms. 1 It can be due to anatomical or functional impairment in the conduction system. It can be observed in healthy children and athletes and is usually asymptomatic. However, in some cases, loss of AV synchrony because of a marked prolongation of the PR interval may cause important haemodynamic alterations, with subsequent decrease in cardiac output and symptoms of heart failure, mimicking a pacemaker syndrome, so-called ‘pseudo-pacemaker syndrome’.
Case
A 40-year-old female consulted the emergency department for nausea, vomiting, and syncope in the setting of gastroenteritis for 2 days. Her clinical history revealed dizziness, palpitations, and several episodes of syncope at rest during childhood. She also mentioned experiencing dyspnoea on exertion for a few years. The physical examination revealed only neck vein distension with intermittent ‘a canon waves’ without other signs of heart failure. Heart rate and blood pressure were normal. The electrocardiogram (ECG) showed a first-degree AV block with a PR interval of 480 ms ( Figure 1 ). The echocardiography, coronary angiogram, and cardiac magnetic resonance imaging were all normal. Auto-immune, endocrinologic, metabolic, and serological investigations were equally normal. The exercise test with Bruce's protocol was maximal for load (10.2 METs) but submaximal for heart rate (157 bpm, 87% of theoretic maximal heart rate) and was stopped for reason of dyspnoea. Electrocardiogram during stress test showed constant PR interval ( Figure 2 ) with gradual shortening of the RR interval, leading to a certain degree of chronotropic insufficiency. Complete electrophysiological study was not available in our hospital, but we performed rapid atrial stimulation. This revealed a Wenckebach point at 130 bpm and a 2:1 AV block point at 150 bpm. After 1 mg atropine, Wenckebach block appeared at 160 bpm and 2:1 AV block at 180 bpm. Finally, there were several episodes of Wenckebach and 2:1 AV block during night time on Holter data.
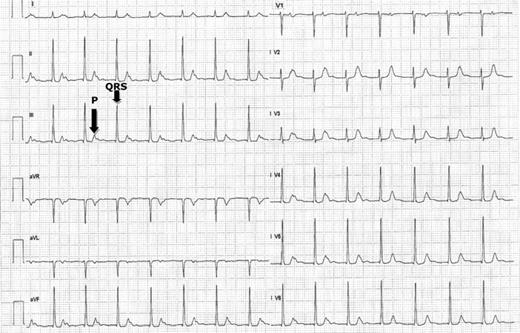
Twelve-lead ECG at rest showing first-degree AV block with a PR interval of 480 ms. The QRS complex following the corresponding P-wave is shown by the black arrows.
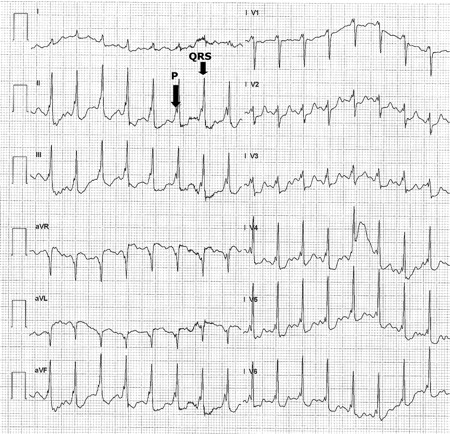
Twelve-lead ECG of the exercise test showing constant PR interval with gradual shortening of the RR interval. The QRS complex following the corresponding P-wave is shown by the black arrows.
Discussion
Our patient showed a pseudo-pacemaker syndrome in the setting of a marked prolonged PR interval. Electrophysiological observations suggested a block at the level of the AV node site, probably congenital. When marked first-degree AV block causes atrial systole in close proximity to the preceding ventricular systole, signs and symptoms similar to the pacemaker syndrome may occur. 2 With marked first-degree AV block, atrial contraction occurs before complete atrial filling, ventricular filling is compromised, and an increase in pulmonary capillary wedge pressure and a decrease in cardiac output follow. The symptoms related by our patient are in relation to this AV asynchrony. A dual-chamber pacemaker was implanted (right atrial and high septum leads) with both clinical and echocardiographic improvement after short AV delay was programmed. Indeed, palpitations, dizziness, dyspnoea, and syncope totally disappeared.
Conclusion
Small uncontrolled trials have suggested some symptomatic and functional improvement by AV pacing of patients with prolonged PR intervals >300 ms by decreasing the time for AV conduction. 3 These same principles also may be applied to patients with type I second-degree AV block who experience haemodynamic compromise due to loss of AV synchrony, even without bradycardia. Permanent pacemaker implantation is actually a Class IIa recommendation for first-degree AV block with symptoms similar to those of pacemaker syndrome or haemodynamic compromise. 1
Conflict of interest: none declared.



