-
PDF
- Split View
-
Views
-
Cite
Cite
Philippe Maury, Alexandre Duparc, Alain Graffeille, Aurelien Hebrard, Pierre Mondoly, Anne Rollin, Marc Delay, Concealed left superior accessory pathway. Distinctive features of retrograde atrial activation and successful ablation using transseptal approach, EP Europace, Volume 12, Issue 4, April 2010, Pages 584–586, https://doi.org/10.1093/europace/eup386
Close - Share Icon Share
Abstract
Concealed left superior accessory pathways are very infrequent and can be difficult to diagnose and ablate. We describe here the case of a patient presenting with reciprocating tachycardia involving superior and inferior left accessory pathways. Left superior accessory pathway was suspected because of the simultaneous retrograde atrial activation at the distal coronary sinus (CS) and His bundle lead and could be successfully ablated using transseptal catheterization.
Case report
A 52-year-old man was referred to our institution for ablation of recurrent paroxysmal tachycardia. There was no pre-excitation on surface ECG. Retrograde conduction was not decremental and insensitive to adenosine. Two types of supra-ventricular tachycardia were repetitively induced by fast atrial pacing: the first one was non-sustained and display earliest atrial depolarization at the proximal CS with a cycle length of 305 ms and a VA interval of 80 ms. After a few seconds, this tachycardia changed into a second, more sustained tachycardia with a longer cycle length (370 ms) and a longer ventriculo-atrial (VA) interval (125 ms) ( Figure 1 ). Earliest atrial depolarization occurred almost simultaneously at the His bundle area and at the distal CS during this second tachycardia ( Figure 1 ). This was understood as synchronous atrial activations from a more superior and median left accessory pathway. P-wave polarity was negative in the inferior leads during the first tachycardia and positive in the inferior leads and negative in VL during the second one. The diagnosis of reciprocating atrioventricular tachycardia using concealed accessory pathways (AP) was confirmed by anticipation of atrial depolarization after a paced premature ventricular beat at the time the His bundle was refractory together with VAV pattern response, and by the lack of change in VA interval during para-hisian pacing.
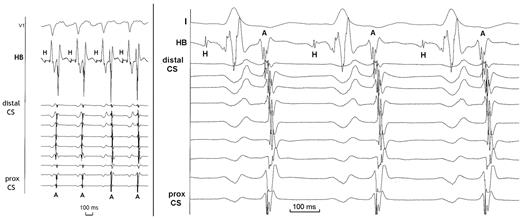
Left: intracardiac recordings showing the change from the first tachycardia to the other one, with an increase in VA interval and in tachycardia cycle length (see text). Right: intracardiac recordings during the tachycardia utilizing the left superior accessory pathways showing nearly simultaneous retrograde activation at the His bundle lead and at the distal coronary sinus. Of note that distal and proximal coronary sinus were also almost synchroneously activated, which would have not been the case in presence of anteroseptal or left posterosuperior accessory pathways. CS, coronary sinus; HB, His bundle lead; H, H bundle potential; A, retrograde atrial depolarisation.
Retrograde conduction could not be eliminated into any accessory pathway due to the inability in positioning the ablation catheter at the low and particularly at the high part of the mitral annulus using retrograde transaortic approach. Due to the length of this first procedure and because of the anticoagulation needed during retrograde aortic approach, a second procedure using transseptal catheterization was planned in the following days. Earliest retrograde activation was found again at the inferior mitral annulus for the first tachycardia and at the superior mitral annulus ( Figure 2 ) for the second one, preceding atrial activation at the His bundle area by 40 ms ( Figure 3 ). The second tachycardia stopped after 5 s of radio-frequency (RF) application at this site and could not be reinduced thereafter (irrigated 4 mm tip catheter, power 30 W, 180 s application). The remaining inducible first tachycardia became then non-sustained and mapping of retrograde activation was performed during ventricular pacing. A similar RF application at the septal side along the lower mitral annulus led to VA dissociation and to the inability to induce any tachycardia. The patient did not present recurrence of supraventricular tachycardia over a follow-up of 3 months.
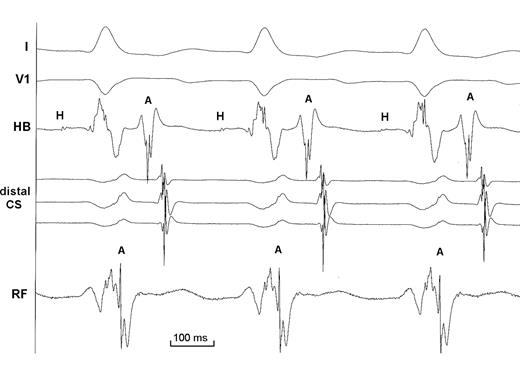
Intracardiac recordings during the second radio-frequency (RF) procedure showing earliest retrograde atrial activation at the RF catheter located at the superior aspect of the mitral annulus. Coronary sinus activation was more delayed during this procedure because coronary sinus lead was not so distally positioned (see Figure 3 ). Of note that VA interval at the successful ablation site is almost virtual, indicating that the length of the left superior by-pass tract is probably short despite the assumed wide fibrous area separating atrial and ventricular myocardium at this site. Same abbreviations as in Figure 1 .
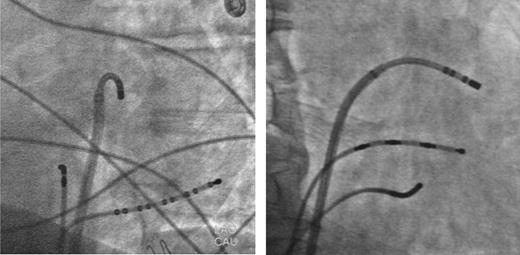
Left (left) and right (right) anterior fluoroscopic views of the successful RF ablation site at the superior aspect of the mitral annulus after transseptal catheterisation. Other catheters were positioned at the His bundle area and at the coronary sinus.
Discussion
Left anterior (or left superior according to the current denomination) and left anteroseptal AP are very uncommon because of the large area of fibrous continuity between aortic and mitral valves, usually precluding close contact and therefore by-pass connection between left atrial and ventricular myocardium. They may represent <0.5% of left AP amenable to ablation.
As mentioned earlier, simultaneous or nearly simultaneous retrograde atrial activation at the His bundle lead and at the distal CS is indicative of left superior AP. 1 Earliest atrial activation usually happens at the distal CS with left anterolateral AP (with a distal to proximal activation of the CS) and with delayed activation at the His bundle, Conversely, anteroseptal AP usually display retrograde atrial activation at the His bundle lead occurring before proximal CS (and with proximal to distal CS activation). Therefore, any close temporal relationship in retrograde activation between both distal CS and His bundle area should raise the possibility of an AP located at mid-distance between both intracardiac leads—i.e. at the superior aspect of the mitral annulus.
Retrograde P-waves during reciprocating tachycardia utilizing a left superior AP have been shown to be negative in the lateral leads and positive in the inferior leads, 1 such as in our case when the tachycardia included the superior AP. P-wave polarity could therefore not be used for differencing left antero-lateral from left superior AP. Moreover, P-wave morphology in V1–V2 does not help since positive (like in our case) or negative P-waves 1 could be observed.
Even if transaortic retrograde approach has been shown to be sometimes successful for ablation of left superior AP, 2 it presents some difficulties in reaching the target area or in positioning the RF catheter with enough stability between both valves. 1 That is why different approaches have been used, such as ablation inside the distal CS, transseptal catheterization, 1 or ablation from the aortic root 1 , 3–5 because of the close spatial relationship between the non-coronary cusp or left sinus of Valsalva and the fibrous continuity between the aortic and mitral annulus.
Conflict of interest: none declared.



