-
PDF
- Split View
-
Views
-
Cite
Cite
James W. McCready, James C. Moon, Anthony W. Chow, Right to left shunt following radiofrequency catheter ablation of atrial fibrillation in a patient with complex congenital heart disease, EP Europace, Volume 12, Issue 2, February 2010, Pages 289–290, https://doi.org/10.1093/europace/eup353
Close - Share Icon Share
Abstract
We report a case of an iatrogenic atrial septal defect following left atrial ablation for persistent atrial fibrillation in a patient with a Fontan circulation. Transseptal puncture was performed with two sheaths across a single puncture and left atrial ablation undertaken. Post procedure the patient became cyanosed with right to left shunting. Transcatheter closure immediately improved symptoms and oxygen saturation.
Atrial arrhythmias occur in 29–41% of patients after a Fontan operation. 1 We report a case of an iatrogenic atrial septal defect (ASD) with significant right to left shunting in a patient with repaired congenital heart disease following a left atrial ablation procedure.
A 29-year-old female with repaired tricuspid atresia and Fontan circulation presented with atrial fibrillation (AF). She had undergone a Blalock shunt operation aged 7 months followed by an AP Fontan with ASD closure at age 8. She developed atrial flutter and fibrillation and initially underwent right atrial (RA) ablation. Following this procedure, she developed highly symptomatic persistent AF and underwent left atrial ablation.
Transoesophageal echo (TOE) demonstrated a dilated RA with a rudimentary right ventricle and preserved inter-atrial anatomy. A single transseptal puncture was performed with a Brockenbrough needle and deflectable sheath (Agilis™, St Jude Medical). A second sheath (Swartz SL0, St Jude Medical) was passed through the same hole using a standard single puncture 2 sheath technique. Two widely encircling circumferential rings were created around the PVs guided by electroanatomical mapping (CARTO, Biosense Webster) with all four PVs electrically isolated verified by a PV mapping catheter. Linear ablation was performed in the roof and from the left inferior PV to mitral valve isthmus and fractionated potentials were targeted in the posterior mitral valve ring. The patient remained in AF at the end of the procedure despite DC cardioversion.
Within days after the procedure the patient became breathless and centrally cyanosed. A repeat TOE showed a persistent ASD with a maximum diameter of 6 mm with bidirectional shunting and the patient underwent magnetic resonance imaging ( Figure 1 ). The patient was referred for closure of the iatrogenic ASD that was performed using a 25 mm Amplazer® patent foramen ovale (PFO) occluder (AGA Medical). Arterial oxygen saturations improved from 86 to 96%. After further DC cardioversion, she remained free from AF for over 3 months.
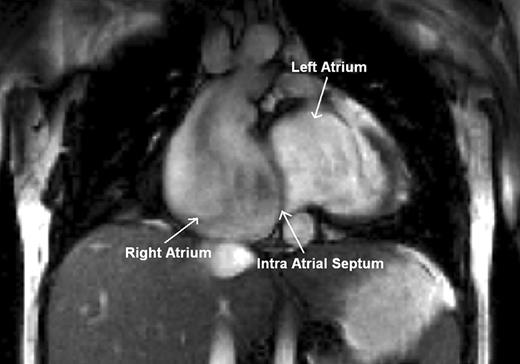
Cardiac magnetic resonance imaging following ablation. The right atrium is severely dilated with slow flow, the left atrium moderately dilated, and the right ventricle rudimentary. The atrial septal defect is not visible on the magnetic resonance imaging.
The persistence of iatrogenic ASDs following transseptal procedures has been reported. In one study, 42 patients underwent TOE 9 months following PVI, no ASDs were seen in patients with a two-sheath double-puncture method, but an ASD was seen in 30% ( n = 8) of those with a two-sheath single-puncture method ( P = 0.01). 2 Patent foramen ovales with significant right to left shunting and hypoxaemia have been described in normal hearts and transcatheter closure has been used to close the defect. 3
In patients with congenital heart disease, high RA pressures and iatrogenic ASD right to left shunting may occur. Our patient was at increased risk because of the long procedure time, elevated RA pressure with the Fontan circulation, and a single-puncture, two-sheath technique.
We recommend that a double-transseptal puncture or a single-sheath technique is used with early sheath withdrawal back into the RA for left atrial ablation procedures, in patients with raised right heart pressures or complex grown up congenital heart disease, to minimize the risk of reverse shunting through an iatrogenic ASD. We have reported successful transcatheter closure of this defect as treatment for this complication.
Conflict of interest: none declared.
Funding
This work was undertaken at UCLH/UCL who received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme.



