-
PDF
- Split View
-
Views
-
Cite
Cite
Sern Lim, Howard Marshall, Broad complex tachycardia and atrioventricular dissociation in a patient with heart transplant, EP Europace, Volume 11, Issue 2, February 2009, Pages 265–267, https://doi.org/10.1093/europace/eun358
Close - Share Icon Share
Case report
A 55-year-old man with a heart transplant performed 4 years ago for heart failure due to ischaemic heart disease was implanted with a dual-chamber pacemaker (Vitatron C50D pacemaker and Medtronic 4074 atrial and ventricular leads) for intermittent atrioventricular (AV) block. P- and R-wave amplitudes measured at implant were 1.5 and 9.5 mV, and pacing thresholds were 0.4 V at 0.5 ms and 0.6 V at 0.5 ms, respectively.
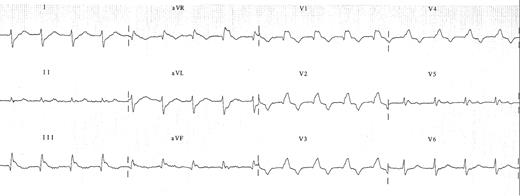
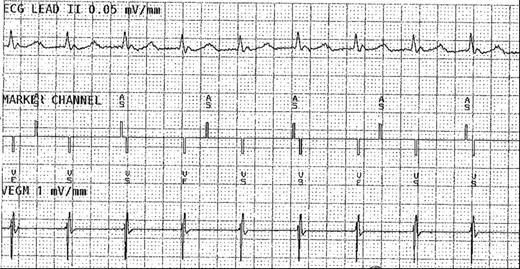
He presented 3 months after pacemaker implantation feeling unwell with increasing breathlessness. His 12-lead ECG showed a broad complex tachycardia of right bundle branch block morphology (about 110 bpm) with no clearly discernible P-wave ( Figure 1 ) and pacemaker interrogation revealed dissociation of atrial and ventricular sensed events ( Figure 2 ). A diagnosis of ventricular tachycardia was made. Repeated attempts at overdrive pacing through the pacemaker failed to terminate the tachycardia, and he was commenced on Amiodarone and Mexiletine.
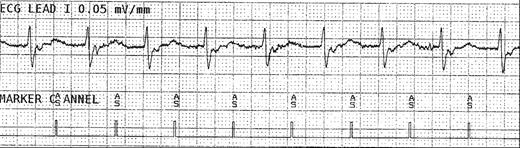
However, his tachycardia persisted despite anti-arrhythmic therapy. The possibility that the atrial lead may be positioned in the recipient remnant atrium was considered as (i) heart transplantation was performed by the biatrial technique in this case and (ii) the atrial rate is unusually low in a patient with a transplanted heart. Intravenous adenosine was administered that resulted in a physiological response. Hence, the atrial lead was repositioned into the donor atrium, which restored AV association and confirmed the diagnosis of sinus tachycardia ( Figure 3 ). The repeat chest X-ray confirmed the more medial position of the atrial lead in the donor atrium following lead repositioning.
In this case, cardiac biopsy did not reveal any evidence of acute rejection. Transthoracic echocardiography demonstrated severe left ventricular dysfunction associated with graft vasculopathy on angiography, which were the likely cause of his symptoms.
Discussion
The biatrial technique of orthoptic heart transplantation preserves the posterior portion of the recipient's atria, including the native sinus node, and the donor heart is transplanted with atrio-atrial anastomosis. The biatrial anastomosis results in distortion of the atrial anatomy and two sinus nodes in the heart transplant patient, which are often dissociated due to the suture line. The recipient remnant atria are not suitable targets for pacing due to high prevalence of arrhythmia and bradycardia. 1
This distortion in atrial anatomy must be considered at the time of atrial lead implantation in a heart transplant recipient. On fluoroscopy in the postero-anterior projection, the donor right atrium should lie more medially and anteriorly in the right anterior oblique projection. The association between atrial (either sensed or paced) and ventricular activity should be confirmed at the time of implantation. The position with the highest amplitude and lowest stimulation threshold should be sought as these parameters may deteriorate during rejection. The use of active fixation bipolar atrial leads is recommended to allow for mapping of the atria and avoid far-field sensing of ventricular and recipient atrial activity. 2
This case highlights the potential peculiarities associated with cardiac pacing following heart transplantation, particularly with biatrial anastomosis. Careful positioning of the atrial lead in the donor atrium will ensure appropriate dual-chamber pacemaker diagnostics and function.



