-
PDF
- Split View
-
Views
-
Cite
Cite
Isabelle Nault, Frederic Sacher, Sebastien Knecht, Matthew Wright, Nicolas Lellouche, Seiichiro Matsuo, Kevin J. Makati, Meleze Hocini, Pierre Jaïs, Michel Haïssaguerre, Wide complex tachycardia in a healthy young man, EP Europace, Volume 10, Issue 11, November 2008, Pages 1340–1342, https://doi.org/10.1093/europace/eun270
Close - Share Icon Share
Abstract
We describe a case of a young man referred with a broad complex tachycardia for evaluation and ablation. Electrophysiological study was performed and revealed a left lateral accessory pathway with antegrade decremental conduction causing antidromic reciprocating re-entrant tachycardia. Ablation was successfully performed. Left lateral accessory pathways with decremental conduction are rarely encountered.
Case presentation
A 24-year-old man was referred to our hospital for ablation of a wide complex tachycardia suspected to be of ventricular origin. He had experienced several paroxysms of tachycardia, essentially in catecholaminergic settings. During these episodes, he reported dizziness. Surface ECG was recorded during the tachycardia and showed wide QRS complexes with right bundle branch morphology at a rate of 160 bpm ( Figure 1 ). The resting ECG was normal ( Figure 1 ). The echocardiogram and magnetic resonance imaging studies of the heart showed normal heart size and function.
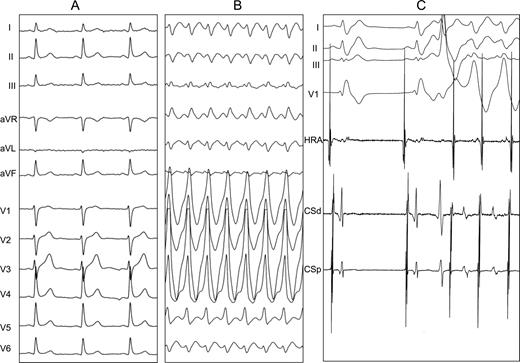
Surface ECG at rest and during tachycardia: ( A ) baseline ECG; ( B ) clinical wide complex tachycardia; ( C ) initiation of tachycardia by ventricular premature beat. HRA, high right atrium; CSd, distal coronary sinus; CSp, proximal coronary sinus.
Electrophysiological testing was carried out under conscious sedation using a quadripolar catheter (Xtrem, ELA Medical, Le-Plessis-Robinson, France), a bipolar diagnostic catheter (Bard, Lowell, USA), and a 4 mm ablation catheter (Celsius, Biosense Webster, Diamond Bar, USA) for ablation. The study was performed with right bundle branch block inadvertently induced during catheter manipulation with recovery after the procedure. Incremental atrial pacing consistently resulted in a wide QRS tachycardia similar in morphology to the clinical tachycardia. What inferences can be made from Figures 1 and 2 with regard to the tachycardia mechanism?

Programmed stimulation, S1 600 ms. His and coronary sinus (CS) recordings during distal CS pacing. ( A ) S2 320 ms, ( B ) S2 260 ms. Evidence of pre-excitation on surface ECG following the extrastimulus. There is no His bundle signal preceding the pre-excited beat, confirming the conduction over the accessory pathway. The conduction over the pathway is decremental, as can be seen in this figure, where the stimulation–ventricular activation intervals get longer with shorter coupling intervals. His d, His distal; His p, His proximal; CSd, distal coronary sinus; CSp, proximal coronary sinus.
Commentary
Figure 1 shows normal baseline sinus rhythm, the wide complex tachycardia with right bundle branch block morphology, and initiation of the tachycardia. The differential diagnosis of a wide complex tachycardia includes supraventricular tachyarrhythmia with aberrancy, ventricular tachycardia (VT), or antidromic atrioventricular reciprocating tachycardia. On the 12-lead ECG, atrial activity was suspected in inferior leads where a P wave could be distinguished with a one-to-one relation with the subsequent QRS and the P wave (and a superior axis). Several clues during the electrophysiological study suggested an atrial contribution the tachycardia. The tachycardia could be induced and terminated by atrial pacing and could also be terminated by spontaneous atrial ectopic beats. Importantly, the QRS morphology could be reproduced with atrial pacing, in favour of atypical aberrancy or atrioventricular pathway, although the QRS axis was hardly compatible with aberrancy. All these observations argued against a ventricular mechanism.
In Figure 2 , during atrial programmed stimulation, widening of the QRS appears following an extrastimulus (S2). His bundle activation present in the normally conducted beats consistently absent before wide QRS complex beats eliminating the hypothesis of aberrant conduction in the His Purkinje system and thus indicating conduction over an accessory pathway. Tachycardia was also initiated following premature ventricular beats, presumably caused by concealed retrograde penetration into the His Purkinje pathway favouring antegrade conduction over the accessory pathway ( Figure 1 C).
Interestingly, when atrial programmed stimulation was performed with shorter coupling interval, the atrioventricular interval prolonged suggesting that the accessory pathway had decremental Mahaim-like properties ( Figure 2 ). Such properties are rare for atrioventricular bypass tracts, in particular ones located left. Right ventricular apical pacing demonstrated a typical concentric atrial activation sequence with decremental conduction consistent with conduction through the atrioventricular (AV) node. The findings during the electrophysiological study were consistent with an atypical atrioventricular bypass tract.
The left atrium was accessed by transeptal puncture and retrograde aortic approach and the mitral annulus mapped. The vector of ventricular activation suggested an accessory pathway located along the lateral mitral annulus. The shortest AV time was noted at the 3 O'clock position on the mitral annulus, and an accessory pathway potential was recorded. Ablation was done while pacing the atria at a rapid rate to unmask pre-excitation. During ablation, the pre-excitation disappeared (best seen in leads II and III, the QRS remaining large because of the mechanically induced right bundle branch block) and at the same atrial pacing rate, AV conduction was 2:1 ( Figure 3 ). Figure 4 shows a short run of non-sustained ventricular tachycardia induced by a catheter in the left ventricle: ventriculo-atrial conduction is concentric and intermittent, suggesting no retrograde pathway is present. At the end of the procedure, no arrhythmia could be induced despite extrastimuli and burst pacing, no other accessory pathway could be found despite antegrade and retrograde pacing.
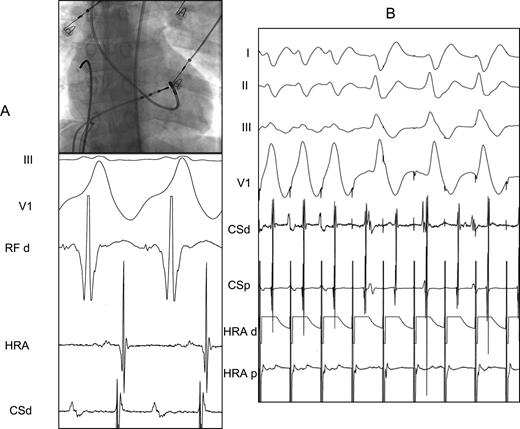
Termination. ( A ) Site of ablation on left lateral mitral annulus where accessory pathway potential is recorded. ( B ) Disapearance of pre-excitation during ablation while pacing the atrium. There is a change in QRS morphology and 2:1 conduction. HRA, high right atrium; HRA d, distal high right atrium; HRA p, proximal high right atrium; CSd, distal coronary sinus; CSp, proximal coronary sinus; RF d, ablation catheter distal.
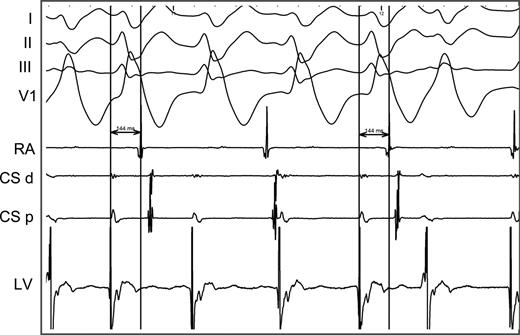
Non-sustained ventricular tachycardia mechanically induced by the map catheter into the left ventricle. Note that the intermittent concentric ventriculo-atrial conduction suggesting no additional retrograde pathway was present in this patient.
Accessory pathways with decremental properties are rare, and most often located on the tricuspid annulus or in the septal area. 1 , 2 They can co-exist with additional atrioventricular accessory pathways. By far nodofascicular or atriofascicular pathways insert in the right bundle branch, giving rise to tachycardias with left bundle branch block morphology. Some right atrioventricular bypass tracts with slow and decremental conduction have also been described. 1–3 Although rare, left-sided atrioventricular decremental pathways have previously been reported. 4 , 5 This case represents an unusual form of an already rare tachycardia utilizing an antegrade pathway with decremental conduction.



