-
PDF
- Split View
-
Views
-
Cite
Cite
Ofer Kobo, Erin D Michos, Ariel Roguin, Rodrigo Bagur, Martha Gulati, Mamas A Mamas, Recommended and observed statin use among US adults with and without cancer, European Journal of Preventive Cardiology, Volume 31, Issue 10, August 2024, Pages 1251–1257, https://doi.org/10.1093/eurjpc/zwae057
Close - Share Icon Share
Abstract
Patients with cancer are at increased cardiovascular (CV) risk. We aimed to compare the recommended and observed statin use among individuals with and without cancer.
Using three 2-year cycles from the National Health and Nutrition Examination Survey (2013–18), we analysed data from 17 050 US adults. We compared the prevalence of Class 1 statin recommendations and use between individuals with and without cancer, overall, and among different demographic groups. Individuals with a history of cancer were older and had a higher burden of comorbidities. Stratified by age groups, they were more likely to have a secondary prevention indication compared with individuals without cancer but not a primary prevention indication for statin. Among individuals with an indication for statin therapy, the prevalence of statin use was higher in the cancer group compared with those without cancer (60.8% vs. 47.8%, P < 0.001), regardless of sex, type of indication (primary vs. secondary prevention), and education level. However, the higher prevalence of statin use in the cancer group was noted among younger individuals, ethnic minorities, and those with lower family income.
Our finding highlights the importance of optimization of CV health in patients with cancer, as individuals with cancer were more likely to have a Class 1 indication for statin treatment when compared with individuals without cancer. Important differences in statin use among cohorts based on sex, age, ethnicity, and socioeconomic status were identified, which may provide a framework through which CV risk factor control can be targeted in this population.
Higher statin use in cancer patients: Among those with Class 1 recommendation to take statins, 60.8% of cancer patients were using them, compared with 47.8% of non-cancer individuals, indicating a greater adherence to heart health recommendations in the cancer group.
Demographic variations in statin use: The study found notable differences in statin use among younger individuals, ethnic minorities, and those with lower income within the cancer patient group, suggesting disparities in how these subgroups manage their cardiovascular health.
Lay Summary
This study reveals that individuals with cancer more likely to have a secondary prevention indication compared with individuals without cancer but not a primary prevention indication for statin and that they had higher rates of compliance with statin treatment, compared with those without cancer.
See the editorial comment for this article ‘Statins among US adults and cancer: where the future liaises?’, by A. Bhalla et al., https://doi.org/10.1093/eurjpc/zwae137.
Background
Cardiovascular disease (CVD) and cancer are the most common causes of death globally.1,2 Patients with cancer face increased cardiovascular (CV) risk due to shared risk factors, cancer treatment-related cardiotoxicity, and pathophysiologic processes associated with the underlying malignancy itself. With increasing cancer survival rates, it is estimated that by 2030, there will be more than 22 million cancer survivors in the USA.3 In this population, the most common cause of death after cancer itself is atherosclerotic CV diseases (ASCVD)4 and CV mortality becomes dominant over the mortality from the primary cancer, as time passes since cancer diagnosis.5
Statins have a key role in the primary and secondary prevention of ASCVD through the reduction of LDL cholesterol (LDL-C). International guidelines recommend statin therapy for all adults with a history of ASCVD to reduce the risk of a recurrent ASCVD event.6,7 Statin therapy is also recommended as primary prevention for adults with increased ASCVD risk. Suboptimal adherence to guideline-recommended statin therapy potentially limits improvements in CV morbidity and mortality,8,9 specifically in high-risk populations.
Despite the increased CV risk of individuals with cancer,10,11 only a few previous studies examined the utilization of statins in individuals with cancer. While one study reported a higher likelihood of statin therapy among cancer survivors following admission with acute myocardial infarction when compared with non-cancer patients,12 other studies reported that statins were significantly underutilized in cancer survivors.13,14 However, these studies were conducted in relatively small cohorts and focused on secondary prevention of ASCVD in cancer patients.
Understanding statin use in patients with cancer and identifying gaps in guideline implantation is crucial for ASCVD prevention in this high-risk population. We therefore utilized data from the National Health and Nutrition Examination Survey (NHANES) to evaluate differences in guideline-recommended and actual statin usage among patients with and without cancer, for both primary and secondary ASCVD prevention.
Methods
The NHANES15 is a series of nationally representative studies designed to monitor the health of the US population. Participants are selected from the US non-institutionalized, civilian population, with the data being publicly available. Because the data are publicly available, patient consent for this analysis was not required and the study was exempt from institutional review board (IRB) approval.
This analysis used three 2-year NHANES cycles (2013–18) to estimate the prevalence of statin recommendations according to the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults,16 along with adherence rates for Class 1 indications of primary and secondary prevention. Although the ACC/AHA Cholesterol Guideline was updated in 2018,6 because our study population included data that preceded these guidelines, the 2013 ACC/AHA Guideline was applied. The total combined sample of NHANES 2013–18 comprised 17 961 adult participants. We excluded 911 individuals with unknown cancer status.
Demographic and social characteristics
Demographic characteristics and cancer status were queried during the home interview. Participants were stratified by self-reported history of cancer (‘Ever told you had cancer or malignancy’).
Household income was utilized as a measure of socioeconomic status (SES) and calculated as the ratio of monthly family income to poverty levels and categorized as low (≤1.30), low to middle (1.31–1.85), middle (1.86–3.50), and high income (>3.50).
Venous blood samples were drawn at the mobile examination centres using standardized protocols. During the 2013–18 data collection cycles, serum LDL-C levels were derived from fasting study participants who were examined in the morning session. LDL cholesterol was calculated from measured values of total cholesterol, triglycerides, and HDL cholesterol (HDL-C) according to the Friedewald calculation (mg/dL): (LDL-C) = (total cholesterol) − (HDL-C) − (triglycerides/5) and is valid for triglycerides ≤ 400 mg/dL. Statin use was identified during the interview or using the NHANES prescription medication data files.
We categorized participants into the three patient management groups according to the 2013 ACC/AHA guideline:16 (i) Class 1 indication for statin as secondary prevention for women and men with self-reported existing ASCVD, (ii) Class 1 indication for statin as primary prevention for adults with LDL-C levels ≥ 190 mg/dL and those 40–75 years of age with diabetes or with an estimated 10-year ASCVD risk ≥ 7.5%, and (iii) no Class 1 indication for statins. Individuals were categorized according to cancer status and age groups. We further examined adherence rates for primary and secondary prevention among individuals with and without cancer.
Statistical analysis
The NHANES oversamples persons 60 and older, African Americans, and Hispanics. To ensure nationally representative estimates, sampling weights were considered in all analyses to account for oversampling of subgroups and complex sample design. Continuous variables are presented as a mean and standard error, and categorical data are presented as percentages and frequencies. Categorical variables were compared using the Pearson χ2 test, whereas continuous variables were compared using Student’s t-test or the Mann–Whitney U test. All analyses were performed using STATA SE version 17.0 (StataCorp, College Station, TX, USA) and SPSS version 26 (IBM, Armonk, NY, USA).
Results
Our analysis included 17 050 participants, of which 1684 had a history of cancer, representing 702.11 million US adults, with 77.66 million (11.1%) having a cancer history. Individuals with a cancer history were older (mean age 65.9 vs. 48.3 years, P < 0.001), more likely to have higher family income [ratio of family income to poverty above 1.86 (60.5% vs. 53.5%, P < 0.001)], and education above high school level (61.5% vs. 54.8%, P < 0.001). LDL cholesterol levels of individuals with and without cancer did not differ (111.2 vs. 111.9, P = 0.07). Those with cancer were also more likely to have CV risk factors, including diabetes, hypertension, and hyperlipidaemia (22.3% vs. 13.4%, 58.0% vs. 34.8%, and 53.3% vs. 32.5%, respectively, all P < 0.001); however, they were less likely to be active smokers (16.2% vs. 19.5%, P < 0.001) (Table 1).
| . | No cancer . | Any cancer . | Overall cohort . | P value . |
|---|---|---|---|---|
| Number of participants | 15 366 (90.1%) | 1684 (9.9%) | 17 050 | |
| Weighted prevalence, % (weighted N, in millions) | 624.45 (88.9%) | 77.66 (11.1%) | 702.11 | |
| Age, years, mean (SD) | 48.3 (17.3) | 65.9 (13.6) | 50.0 (17.7) | <0.001 |
| Age, years | ||||
| 18–39 | 35.7% | 5.9% | 32.8% | <0.001 |
| 40–64 | 43.8% | 32.7% | 42.7% | |
| 65–79 | 15.4% | 39.6% | 17.8% | |
| 80 and over | 5.1% | 21.7% | 6.8% | |
| Sex | ||||
| Men | 48.3% | 46.4% | 48.1% | 0.13 |
| Women | 51.7% | 53.6% | 51.9% | |
| Self-reported race and ethnicity | ||||
| Mexican American | 15.4% | 7.7% | 14.6% | <0.001 |
| Other Hispanic | 10.9% | 7.4% | 10.5% | |
| Non-Hispanic White | 33.9% | 62.5% | 36.8% | |
| Non-Hispanic Black | 22.3% | 14.4% | 21.5% | |
| Other race | 17.5% | 8.1% | 16.6% | |
| Ratio of family income to poverty | ||||
| <1.31 | 32.8% | 26.1% | 32.1% | <0.001 |
| 1.31–1.85 | 13.7% | 13.3% | 13.7% | |
| 1.86–3.5 | 24.3% | 26.8% | 24.5% | |
| >3.5 | 29.2% | 33.7% | 29.7% | |
| Education level | ||||
| Less than high school | 22.4% | 17.0% | 21.9% | <0.001 |
| High school or equivalent | 22.8% | 21.5% | 2.7% | |
| More than high school | 54.8% | 61.5% | 55.4% | |
| Comorbidities | ||||
| Diabetes mellitus | 13.4% | 22.3% | 14.3% | <0.001 |
| Hypertension | 34.8% | 58.0% | 37.1% | <0.001 |
| Hyperlipidaemia | 32.5% | 53.3% | 34.6% | <0.001 |
| Active smoker | 19.5% | 16.2% | 19.2% | <0.001 |
| Mean LDL-C, mg/dL (SD) | 111.9 (35.3) | 111.2 (35.4) | 111.8 (35.4) | 0.07 |
| . | No cancer . | Any cancer . | Overall cohort . | P value . |
|---|---|---|---|---|
| Number of participants | 15 366 (90.1%) | 1684 (9.9%) | 17 050 | |
| Weighted prevalence, % (weighted N, in millions) | 624.45 (88.9%) | 77.66 (11.1%) | 702.11 | |
| Age, years, mean (SD) | 48.3 (17.3) | 65.9 (13.6) | 50.0 (17.7) | <0.001 |
| Age, years | ||||
| 18–39 | 35.7% | 5.9% | 32.8% | <0.001 |
| 40–64 | 43.8% | 32.7% | 42.7% | |
| 65–79 | 15.4% | 39.6% | 17.8% | |
| 80 and over | 5.1% | 21.7% | 6.8% | |
| Sex | ||||
| Men | 48.3% | 46.4% | 48.1% | 0.13 |
| Women | 51.7% | 53.6% | 51.9% | |
| Self-reported race and ethnicity | ||||
| Mexican American | 15.4% | 7.7% | 14.6% | <0.001 |
| Other Hispanic | 10.9% | 7.4% | 10.5% | |
| Non-Hispanic White | 33.9% | 62.5% | 36.8% | |
| Non-Hispanic Black | 22.3% | 14.4% | 21.5% | |
| Other race | 17.5% | 8.1% | 16.6% | |
| Ratio of family income to poverty | ||||
| <1.31 | 32.8% | 26.1% | 32.1% | <0.001 |
| 1.31–1.85 | 13.7% | 13.3% | 13.7% | |
| 1.86–3.5 | 24.3% | 26.8% | 24.5% | |
| >3.5 | 29.2% | 33.7% | 29.7% | |
| Education level | ||||
| Less than high school | 22.4% | 17.0% | 21.9% | <0.001 |
| High school or equivalent | 22.8% | 21.5% | 2.7% | |
| More than high school | 54.8% | 61.5% | 55.4% | |
| Comorbidities | ||||
| Diabetes mellitus | 13.4% | 22.3% | 14.3% | <0.001 |
| Hypertension | 34.8% | 58.0% | 37.1% | <0.001 |
| Hyperlipidaemia | 32.5% | 53.3% | 34.6% | <0.001 |
| Active smoker | 19.5% | 16.2% | 19.2% | <0.001 |
| Mean LDL-C, mg/dL (SD) | 111.9 (35.3) | 111.2 (35.4) | 111.8 (35.4) | 0.07 |
| . | No cancer . | Any cancer . | Overall cohort . | P value . |
|---|---|---|---|---|
| Number of participants | 15 366 (90.1%) | 1684 (9.9%) | 17 050 | |
| Weighted prevalence, % (weighted N, in millions) | 624.45 (88.9%) | 77.66 (11.1%) | 702.11 | |
| Age, years, mean (SD) | 48.3 (17.3) | 65.9 (13.6) | 50.0 (17.7) | <0.001 |
| Age, years | ||||
| 18–39 | 35.7% | 5.9% | 32.8% | <0.001 |
| 40–64 | 43.8% | 32.7% | 42.7% | |
| 65–79 | 15.4% | 39.6% | 17.8% | |
| 80 and over | 5.1% | 21.7% | 6.8% | |
| Sex | ||||
| Men | 48.3% | 46.4% | 48.1% | 0.13 |
| Women | 51.7% | 53.6% | 51.9% | |
| Self-reported race and ethnicity | ||||
| Mexican American | 15.4% | 7.7% | 14.6% | <0.001 |
| Other Hispanic | 10.9% | 7.4% | 10.5% | |
| Non-Hispanic White | 33.9% | 62.5% | 36.8% | |
| Non-Hispanic Black | 22.3% | 14.4% | 21.5% | |
| Other race | 17.5% | 8.1% | 16.6% | |
| Ratio of family income to poverty | ||||
| <1.31 | 32.8% | 26.1% | 32.1% | <0.001 |
| 1.31–1.85 | 13.7% | 13.3% | 13.7% | |
| 1.86–3.5 | 24.3% | 26.8% | 24.5% | |
| >3.5 | 29.2% | 33.7% | 29.7% | |
| Education level | ||||
| Less than high school | 22.4% | 17.0% | 21.9% | <0.001 |
| High school or equivalent | 22.8% | 21.5% | 2.7% | |
| More than high school | 54.8% | 61.5% | 55.4% | |
| Comorbidities | ||||
| Diabetes mellitus | 13.4% | 22.3% | 14.3% | <0.001 |
| Hypertension | 34.8% | 58.0% | 37.1% | <0.001 |
| Hyperlipidaemia | 32.5% | 53.3% | 34.6% | <0.001 |
| Active smoker | 19.5% | 16.2% | 19.2% | <0.001 |
| Mean LDL-C, mg/dL (SD) | 111.9 (35.3) | 111.2 (35.4) | 111.8 (35.4) | 0.07 |
| . | No cancer . | Any cancer . | Overall cohort . | P value . |
|---|---|---|---|---|
| Number of participants | 15 366 (90.1%) | 1684 (9.9%) | 17 050 | |
| Weighted prevalence, % (weighted N, in millions) | 624.45 (88.9%) | 77.66 (11.1%) | 702.11 | |
| Age, years, mean (SD) | 48.3 (17.3) | 65.9 (13.6) | 50.0 (17.7) | <0.001 |
| Age, years | ||||
| 18–39 | 35.7% | 5.9% | 32.8% | <0.001 |
| 40–64 | 43.8% | 32.7% | 42.7% | |
| 65–79 | 15.4% | 39.6% | 17.8% | |
| 80 and over | 5.1% | 21.7% | 6.8% | |
| Sex | ||||
| Men | 48.3% | 46.4% | 48.1% | 0.13 |
| Women | 51.7% | 53.6% | 51.9% | |
| Self-reported race and ethnicity | ||||
| Mexican American | 15.4% | 7.7% | 14.6% | <0.001 |
| Other Hispanic | 10.9% | 7.4% | 10.5% | |
| Non-Hispanic White | 33.9% | 62.5% | 36.8% | |
| Non-Hispanic Black | 22.3% | 14.4% | 21.5% | |
| Other race | 17.5% | 8.1% | 16.6% | |
| Ratio of family income to poverty | ||||
| <1.31 | 32.8% | 26.1% | 32.1% | <0.001 |
| 1.31–1.85 | 13.7% | 13.3% | 13.7% | |
| 1.86–3.5 | 24.3% | 26.8% | 24.5% | |
| >3.5 | 29.2% | 33.7% | 29.7% | |
| Education level | ||||
| Less than high school | 22.4% | 17.0% | 21.9% | <0.001 |
| High school or equivalent | 22.8% | 21.5% | 2.7% | |
| More than high school | 54.8% | 61.5% | 55.4% | |
| Comorbidities | ||||
| Diabetes mellitus | 13.4% | 22.3% | 14.3% | <0.001 |
| Hypertension | 34.8% | 58.0% | 37.1% | <0.001 |
| Hyperlipidaemia | 32.5% | 53.3% | 34.6% | <0.001 |
| Active smoker | 19.5% | 16.2% | 19.2% | <0.001 |
| Mean LDL-C, mg/dL (SD) | 111.9 (35.3) | 111.2 (35.4) | 111.8 (35.4) | 0.07 |
In general, individuals with a cancer history were more likely to have a greater prevalence of a Class 1 indication for statin treatment (28.4% vs. 15.8%) than those without cancer, largely driven by a higher likelihood of a secondary prevention indication (22.3% vs. 8.8%, P < 0.001). When stratified by age groups, individuals with cancer had a lower likelihood of having a primary prevention indication for statin across all age groups but a higher likelihood for secondary prevention among those aged 18–39, 40–64, and 80 years and above (Figure 1).
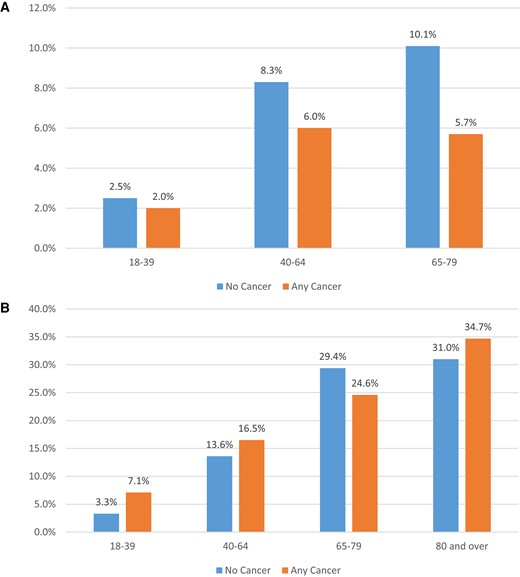
Per cent of individuals with statin recommendations, by age and cancer status. (A) Primary prevention and (B) secondary prevention.
Supplementary material online, Tables S1 and S2, present the baseline characteristics of individuals with a Class 1 indication for statin treatment with and without a cancer history. Among individuals with an indication for statin treatment as primary or secondary prevention, those with cancer were older and more likely to be non-Hispanic White and to have higher family income and level of education. They were also more likely to have diabetes mellitus, hypertension, and hyperlipidaemia and less likely to be active smokers. While LDL-C levels were similar among individuals with a secondary prevention indication with and without cancer (96.5 vs. 96.7 mg/dL, P = 0.18), individuals with a primary prevention indication with cancer had lower LDL-C compared with those without cancer (120.4 vs. 127.8 mg/dL, P < 0.001).
Individuals with cancer were found to be more likely to use statins in accordance with the ACC/AHA guidelines, compared with those without cancer. Statin use was observed in over 60% of cancer patients who were indicated for statin therapy, as compared with 47.8% in individuals without cancer (P < 0.001). This proportion was observed for both primary (39.0% vs. 35.2%) and secondary prevention indications (66.8% vs. 61.1%), as shown in Figure 2.
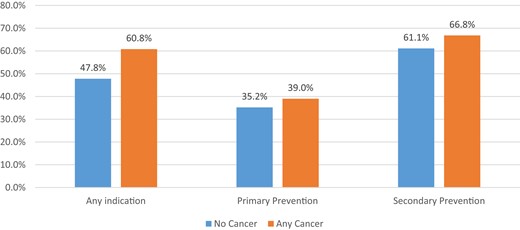
Per cent observed statin use among individuals with Class 1 by cancer status and type of statin indication.
When stratified by age, a higher prevalence of statin use was observed among individuals with cancer who were under the age of 65 years, compared with those without cancer. However, among individuals aged 80 or older with a Class 1 indication of statin use, the prevalence of statin use was lower among those with cancer, compared with those without cancer. Among individuals with and without cancer, the highest likelihood of statin use according to the ACC/AHA guidelines was observed among those aged above 65 (65–79 years old and 80 years or older) (Supplementary material online, Figure S1A).
Regarding sex, among individuals with an indication for statin therapy, men were more likely to use statins regardless of cancer status. Both men and women with cancer were more likely to use statins compared with individuals without cancer, but the difference was more prominent in men (75.8% vs. 57.4% and 45.4% vs. 39.6% for men and women, respectively, both P < 0.001) (Supplementary material online, Figure S1B). When stratified by self-reported race and ethnicity, the higher prevalence of statin use among individuals with cancer was consistent across racial groups but more prominent among non-White individuals. Among individuals with cancer, the highest prevalence of statin use was in the ‘other race’ group (83.7%), while among individuals without cancer, the highest statin use was observed among non-Hispanic White individuals (56.9% compared with 60.0% among non-Hispanic White individuals with cancer) (Supplementary material online, Figure S1C).
When stratified by family income, we observed a higher prevalence of statin use among individuals with cancer with a ratio of family income to poverty below 3.5. However, among those with a higher ratio of family income to poverty, the prevalence of statin use was similar among individuals with and without cancer (Supplementary material online, Figure S1D). Finally, when stratified by education level, the increased prevalence of statin use among individuals with cancer was consistent across all education level groups, with the highest prevalence observed among individuals with cancer history with less than high school education (Supplementary material online, Figure S1E).
Discussion
Our analysis of indications and utilization of statin therapy in adults with and without a history of cancer demonstrates several important findings. Individuals with cancer are more likely to have a Class 1 indication for statin treatment as secondary prevention and less likely to have an indication as primary prevention when compared with individuals without cancer. Additionally, statin use was observed in over 60% of cancer patients who were indicated for statin therapy, as compared with only 47.8% in individuals without cancer. However, there were important differences in statin use among cohorts based on sex, age, ethnicity, and SES, which may provide a framework through which CV risk factor control can be targeted in this population.
When stratified by age, individuals with cancer were less likely to have a primary prevention indication to statin despite the higher prevalence of many ASCVD risk factors, an observation that may suggest better risk factor management in patients with cancer. A higher awareness of health may also be manifested by the lower rates of active smoking among individuals with history of cancer compared with individuals without a history of cancer.
In line with previous reports,11,17 we found that individuals with cancer were older and were more likely to have risk factors as diabetes mellitus, hyperlipidaemia, and hypertension, as well as established ASCVD. Our finding of a higher likelihood of an indication for secondary prevention statin prescription among individuals with cancer, particularly in the elderly cancer population, aligns with the increased CV morbidity and mortality faced by cancer survivors,5,18 emphasizing the need for comprehensive cardio-oncology services.
The importance of cholesterol-lowering therapy in patients with cancer was recently demonstrated in a study among over 13 000 female patients with breast cancer, in which overall mortality was significantly lower among statin users.19 In addition to the role of statins in the primary and secondary prevention of ASCVD, statins attenuate left ventricular ejection fraction (LVEF) decline following doxorubicin treatment.20 Furthermore, abnormal cholesterol metabolism has been linked to the development and progression of tumours, and changes in cholesterol metabolism triggered by internal or external stimuli can promote tumour growth. During metastasis, tumour cells require large amounts of cholesterol to support their growth and colonization of new organs.21 While identifying the specific targets in cholesterol metabolism that regulate cancer progression is still a challenge, statins may be beneficial in the treatment of prostate22 and liver cancer.23 The European Society of Cardiology (ESC) guidelines on cardio-oncology recommend statins should be considered for primary prevention in adult patients with cancer at high and very high CV toxicity risk.24
Previous studies focused on statin utilization in cancer survivors compared with individuals without cancer have presented conflicting results. A study that included 1119 cancer survivors and 7886 propensity score-matched non-cancer acute myocardial infarction patients reported that cancer survivors were more likely to receive statins.12 In contrast, among individuals included in the acute myocardial infarction in Switzerland (AMIS Plus) registry, patients with a history of cancer were less likely to receive guideline-recommended treatment, including statins.14 Similar finding were reported in an analysis of the National Heart Attack Myocardial Infarction National Audit Project (MINAP) registry in the UK.25 Another single-centre study assessed cardioprotective medication prescription pre-admission to the cardiology unit and reported underutilization of statins among patients with a history of cancer, compared with those without a history of cancer.13 A single-centre retrospective study focusing on CV risk factor management of breast cancer survivors reported that 57% of those with statin indication received statins.26 Our study, which included the largest cohort of individuals with cancer with primary and secondary prevention indications, observed a higher prevalence of statin use among individuals with cancer and any Class 1 indication for statin therapy compared with those without cancer.
We observed a higher prevalence of statin use in male and older age groups, similar to previous reports.9 Interestingly, among individuals aged 64 years old and younger, the prevalence of statin use was higher in the cancer group, while among those aged 65 years old and older, a higher prevalence of statin use was observed in those without cancer. This may suggest less awareness of CV health among older cancer patients.
Previous studies reported differences in statin use across demographic groups. In previous studies, ethnic minorities, especially Black or Hispanic individuals, were less likely to receive statin therapy for primary and secondary prevention27–29; we observed a higher prevalence of statin use among non-Hispanic White individuals compared with non-Hispanic Black and Hispanic individuals. Higher statin use was observed in cancer groups across all ethnic and racial groups, with prominent differences in the non-White groups. As routine healthcare access was associated with increased statin use in both primary and secondary prevention,9,27 our findings may suggest that the improved access to healthcare in cancer patients may attenuate racial and ethnic disparities in access to healthcare. Our hypothesis that the higher prevalence of statin use among individuals with a cancer history is related to access to healthcare can also be supported by the observation that no differences were noted between cancer and non-cancer patients with high family income. However, the differences in statin use prevalence were noted across all education level spectra.
Improving cancer patients’ education and awareness of the increased CV risk was suggested by the ESC cardio-oncology guidelines as an important step in mitigation of this risk.24 Patients should be informed that a regular long-term CV follow-up is required. Both e-tools and non-electronic leaflets may assist in this complex task.30,31
Our analysis has limitations, including those inherent to data set analyses. Important variables regarding cancer type, treatment, and the interval between cancer diagnosis and data collection are not available. Self-reported and prescription medication data available did not include intensity or reason for use; misclassification of some individuals to a lower-risk category may have occurred for several reasons including the fact that NHANES has information for only three out of the four major ASCVD categories (symptomatic peripheral arterial disease is not available). Furthermore, among individuals not taking statin despite a Class 1 indication, we cannot differentiate between those who were not prescribed a statin by their physician and those who were statin intolerant, prescribed another class of anti-lipid therapies, or despite a medical indication declined a statin. Another important limitation of NHANES is that it does not provide further details about those included in the ‘other races’ category such as American Indian and Alaska Native (AIAN), Native Hawaiian and Other Pacific Islanders (NHOPI), and/or Asian Americans. Finally, as this is an observational, cross-sectional study. residual confounding may explain in part the associations seen.
In summary, we found that adults with a cancer history were more likely to use a statin when indicated. This finding is encouraging, suggesting that healthcare professionals are effectively managing CV risk in this population. This observation along with a lower likelihood of an indication for statin prescription for primary prevention and a lower prevalence of active smoking among individuals with cancer, as well as lower LDL-C level among individuals with a primary prevention indication, may all be related to greater access to healthcare providers and increased awareness of health following a diagnosis of cancer. However, this increased prevalence of statin therapy was noted in patients under the age of 65, emphasizing the importance of extending these practices to the elderly cancer population. Furthermore, statin use among those individuals with cancer and a primary prevention indication, as well as among females, younger individuals, and those belonging to ethnic minority groups, was relatively low. This emphasizes the importance of targeted interventions, to ensure that the benefits of statin therapy extend to all cancer survivors. Efforts to bridge the gap between guideline recommendations and actual clinical practice are crucial for improving CV outcomes in cancer patients and survivors.
Supplementary material
Supplementary material is available at European Journal of Preventive Cardiology.
Author contribution
O.K.: writing—original draft, formal analysis, and methodology. E.D.M., A.R., R.B., and M.G.: writing—reviewing and editing. M.A.M.: writing—reviewing and editing, project administration, conceptualization, and methodology.
Funding
None declared.
Data availability
The data underlying this article are available in the NAHNES website, at https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
References
Author notes
Conflict of interest: none declared.




Comments