-
PDF
- Split View
-
Views
-
Cite
Cite
Sean Pymer, Simon Nichols, Jonathon Prosser, Stefan Birkett, Sean Carroll, Lee Ingle, Does exercise prescription based on estimated heart rate training zones exceed the ventilatory anaerobic threshold in patients with coronary heart disease undergoing usual-care cardiovascular rehabilitation? A United Kingdom perspective, European Journal of Preventive Cardiology, Volume 27, Issue 6, 1 April 2020, Pages 579–589, https://doi.org/10.1177/2047487319852711
Close - Share Icon Share
Abstract
In the United Kingdom (UK), exercise intensity is prescribed from a fixed percentage range (% heart rate reserve (%HRR)) in cardiac rehabilitation programmes. We aimed to determine the accuracy of this approach by comparing it with an objective, threshold-based approach incorporating the accurate determination of ventilatory anaerobic threshold (VAT). We also aimed to investigate the role of baseline cardiorespiratory fitness status and exercise testing mode dependency (cycle vs. treadmill ergometer) on these relationships.
A maximal cardiopulmonary exercise test was conducted on a cycle ergometer or a treadmill before and following usual-care circuit training from two separate cardiac rehabilitation programmes from a single region in the UK. The heart rate corresponding to VAT was compared with current heart rate-based exercise prescription guidelines.
We included 112 referred patients (61 years (59–63); body mass index 29 kg·m–2 (29–30); 88% male). There was a significant but relatively weak correlation (r = 0.32; p = 0.001) between measured and predicted %HRR, and values were significantly different from each other (p = 0.005). Within this cohort, we found that 55% of patients had their VAT identified outside of the 40–70% predicted HRR exercise training zone. In the majority of participants (45%), the VAT occurred at an exercise intensity <40% HRR. Moreover, 57% of patients with low levels of cardiorespiratory fitness achieved VAT at <40% HRR, whereas 30% of patients with higher fitness achieved their VAT at >70% HRR. VAT was significantly higher on the treadmill than the cycle ergometer (p < 0.001).
In the UK, current guidelines for prescribing exercise intensity are based on a fixed percentage range. Our findings indicate that this approach may be inaccurate in a large proportion of patients undertaking cardiac rehabilitation.
Introduction
Cardiovascular rehabilitation is a multi-disciplinary secondary prevention programme that has been shown to contribute to reduced hospital admissions, and improvements in patient quality of life, following a cardiac event.1–4 Historically, a 1% improvement in peak oxygen uptake (VO2peak) resulting from exercise-based cardiovascular rehabilitation was thought to confer a 2% reduction in premature mortality.5 Similarly, every 3.5 mL·kg–1·min–1 increment in VO2peak has been associated with a 12–13% survival benefit6,7 in men referred for exercise testing. Therefore, it is essential that the prescribed dose of exercise is sufficient to stimulate improvements in VO2peak following cardiovascular rehabilitation. Recent systematic reviews and meta-analyses have shown that increased exercise intensity is an important factor in achieving superior outcomes in patients with cardiovascular disease.8,9
The prescribed dose of exercise can be influenced by manipulating exercise frequency, duration, type/mode, and/or intensity (exercise dose).10 In the United Kingdom (UK), current long-term exercise training guidelines for patients undertaking cardiovascular rehabilitation recommend exercise training intensities between 40% and 70% heart rate reserve (HRR), oxygen uptake reserve, or a Borg rating of perceived exertion (RPE) between 11 and 14.11,12 Both continuous and interval training at an objective physiological threshold has been shown to have a beneficial impact by improving VO2peak.13 Training at or above the ventilatory anaerobic threshold (VAT), often referred to as the first ventilatory threshold, indicates the point above which further increments in work rate are increasingly supplemented through anaerobic metabolism.13,14–16 Despite being associated with mild metabolic perturbations,13,16 regular exercise bouts conducted at work rates equivalent to VAT are well tolerated17 and induce physiological adaptation, leading to improved cardiorespiratory fitness (CRF) and other cardiovascular risk factors.18,19 However, whilst work rates corresponding to VAT may represent a minimum intensity needed to improve CRF, metabolic gas equipment and calibrated ergometers are often not available in a cardiovascular rehabilitation setting in the UK. Prescribing exercise as a percentage of measured HRR, or most typically estimated HRR, is often a more practical and realistic alternative in UK cardiac rehabilitation settings.10
The 40% HRR threshold is cited as the lowest effective exercise intensity for improving CRF in patients undertaking cardiovascular rehabilitation.10,12 The individual VAT is widely accepted to occur between 45% and 65% HRR in healthy and in cardiac patients,8 with lower values reported in patients with a chronic cardiovascular disease.10 However, the distribution of VAT values, and its relation to exercise capacity, is unclear in patients undertaking cardiovascular rehabilitation. How commonly VAT occurs within discrete exercise intensity ranges is also under-reported in patients with coronary artery disease. Tan et al.20 showed that the mean VAT was equal to 82% of maximal heart rate (HR), in 19 cardiac patients referred for a cardiopulmonary exercise test (CPET) prior to cardiovascular rehabilitation.20 However, the mode of exercise testing may also influence when an individual’s VAT occurs.
In the UK, the mode of exercise testing varies between cardiovascular rehabilitation programmes. This means that a patient’s exercise prescription could be based on a number of different submaximal exercise tests, including the 6-min walk test, incremental shuttle walk test, step test, or cycle ergometry. The differing metabolic responses to cycling compared with walking may affect a patient’s O2peak and the occurrence of VAT. This, in turn, may significantly affect the accuracy of exercise intensity prescription. These issues have not been addressed sufficiently within UK guidelines for exercise prescription in cardiovascular rehabilitation programmes. This information may help practitioners to optimise a patient's initial exercise prescription and maximise the improvements associated with exercise training programmes. This is especially important when the frequency and duration of cardiovascular rehabilitation sessions are finite. We aimed to determine the accuracy of the standard UK approach for prescribing exercise in patients undertaking cardiovascular rehabilitation by comparing it with objective measures of exercise prescription, namely O2peak and VAT. Secondary aims were to determine how exercise modality (exercise testing with cycle versus treadmill ergometer) and baseline levels of CRF affected the concordance of VAT and HRR measures.
Methods
Data were collated from the baseline assessment of two separate cohorts who undertook a maximal effort CPET to volitional exhaustion prior to commencing a cardiovascular rehabilitation programme. The methods for these studies have previously been reported.21,22 Ethical approval was provided by the Yorkshire and Humber – Sheffield National (12/YH/0072) and Humber Bridge NHS (12/YH/0278) Research Ethics Committees. Briefly, patients were recruited following a referral to cardiovascular rehabilitation for angina, myocardial infarction, coronary artery bypass graft or percutaneous coronary intervention (PCI). Patients attended a baseline study assessment, where written informed consent was obtained. CPET was conducted on a cycle ergometer following a 25 W incremental protocol, or on a treadmill following the modified Bruce protocol,23 adopting previously outlined test termination and maximal effort criteria.15,24 Breath-by-breath metabolic gas exchange data were collected using an Innocor (Innovision, Glamsbjerg, Denmark) or Oxycon-Pro metabolic cart (Jaeger, Hoechburg, Germany), respectively, which were calibrated according to manufacturers’ instructions and current recommendations.25 Peak values were averaged over the final 30 s of the CPET. VO2peak was reported in absolute values (L·min–1) and standardised to each patient’s body mass (mL·kg–1·min–1). Individualised VAT was independently determined by two investigators (using the average of the middle five of every seven breaths plotted in the V-slope method, and verified using the ventilatory equivalents.14,26 Where investigators reported different VAT values, a third reviewer was consulted and the threshold value agreed by consensus. The VAT was reported in L·min–1 and mL·kg–1·min–1 and expressed as a percentage of directly-determined and predicted VO2peak.27 The HR at VAT was then established and reported as a ratio of maximum heart rate (HRmax) and HRR determined from CPET, and as a ratio of predicted HRmax and HRR with relevant adjustment for the effects of β-blockade on maximal heart rates as follows10:
((205.8 – (0.685 × age)) – resting heart rate (–30 beats per min if taking beta-blockers)
To characterise where a patient’s VAT occurred in relation to established training zones, the VAT values were categorically assigned to exercise intensity groups of <40%, 40–49%, 50–59%, 60–69%, 70%, and >70% of measured and predicted HRR. Adjustment for β-blockades were made where appropriate.12 We assessed how many patients had a VAT that occurred within the exercise training intensity ranges recommended by UK cardiovascular rehabilitation guidelines, namely 40–70% HRR, or an RPE between 11 and 14.11,12 Patients were sub-categorised according to individual CRF levels as low (<5 metabolic equivalents (METs) for women, <6 METs for men), moderate (5 < 7 METs for women, 6 < 8 METs for men), and high CRF (≥7 METs for women, ≥8 METs for men), based on exercise capacity (MET) thresholds derived from the international literature and previously applied to cardiac patients in the UK.28 These sub-groups were then categorised based on the HRR zone that the individualised VAT occurred within. We also conducted sub-analyses on patients who undertook their CPET on either a treadmill or a cycle ergometer.
Data analysis
Statistical analysis was conducted using SPSS version 24 (IBM, New York, USA). When data were not normally distributed, normalisation of the distribution was attempted using log10 transformation. Logarithmically transformed data were analysed in their transformed state and reported as an arithmetic mean to allow for meaningful interpretation. Normally distributed and transformed data were analysed using a univariate general linear model with significance set at arbitrary level (p < 0.05) and are presented as mean (95% confidence interval (CI)), and partial-eta squared (ηp2) effect sizes, with 0.01, 0.06 and 0.14 denoting small, moderate and large effects, respectively.29 For non-normally distributed data, a Mann–Whitney U test was conducted with median and range reported. Categorical data was analysed using a Chi-squared test of independence and reported as percentage and frequency. When ≥1 cell had an expected value <5, the Fisher’s exact test was used.
Results
Patient characteristics
One-hundred and twelve (N = 112) cardiac patients were included for analysis (61.3 years (59.4–63.1); 29.3 kg·m–2 (28.5–30.1); 88% male). Forty-two patients (n = 42; 37.5%) undertook their CPET on a cycle ergometer. Patients on a cycle ergometer achieved 79.1% of their predicted HRmax (74.6–83.6%), an RPE of 18 (17–18) and a peak respiratory exchange ratio (RER) of 1.02 (1.00–1.05). Seventy (n = 70) patients undertook CPET on a treadmill. Patients conducting CPET on a treadmill achieved 82.3% (79.7–84.9%) of predicted HRmax, an RPE of 17.8 (17.3–18.3) and a peak RER of 1.09 (1.06–1.11). Of the patients undergoing cycle and treadmill testing, 77% and 86%, respectively, were prescribed beta-blockers. The majority of patients had a diagnosis of myocardial infarction with primary (32.5%) or elective (28.9%) PCI. There was a greater prevalence of active smokers (p = 0.017) in those that conducted a CPET on a cycle ergometer. There were significant between-group differences for age (p = 0.012; = 0.054), and resting HR (mean difference 5.8 beats/min (95% CI 1.0–10.5 beats/min) p = 0.032; Table 1) between the test modality groups. Forty-two out of 112 patients were classified within the lower cardiorespiratory fitness group, 50 in the moderate-fitness group and 20 in the high-fitness group (Table 2).
| Variable . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Sex, male/female | 100/14 (87.70% male) | 40/4 (90.0% male) | 60/10 (85.7% male) | 0.411 | |
| Age, years | 61.25 (95% CI: 59.35 to 63.14) | 63.13 (95% CI: 60.75 to 65.51) | 58.25 (95% CI: 55.21 to 61.29) | 0.012* | 0.054 |
| BMI, kg/m2 Tr | 29.30 (95% CI: 28.54 to 30.07) | 30.1 (95% CI: 28.8 to 31.44) | 28.80 (95% CI: 29.74 to 27.90) | 0.101 | 0.024 |
| Resting SBP, mmHg Tr | 131.55 (95% CI: 127.94 to 135.27) | 139.57 (95% CI 134.39 to 144.95) | 126.74(95% CI: 122.18 to 131.46) | 0.001** | 0.099 |
| Resting DBP, mmHg | 83 (60 to 149) | 85.50 (62 to 104) | 82 (60 to 149) | 0.09 | |
| LVEF, % | 55.77 (95% CI: 54.34 to 57.20) | 57.05 (95% CI: 54.35 to 59.75) | 54.99 (95% CI: 53.35 to 56.62) | 0.167 | 0.017 |
| Resting HR, beats/min | 60 (42 to 95) | 64 (44 to 95) | 56 (42 to 91) | 0.008** |
| Variable . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Sex, male/female | 100/14 (87.70% male) | 40/4 (90.0% male) | 60/10 (85.7% male) | 0.411 | |
| Age, years | 61.25 (95% CI: 59.35 to 63.14) | 63.13 (95% CI: 60.75 to 65.51) | 58.25 (95% CI: 55.21 to 61.29) | 0.012* | 0.054 |
| BMI, kg/m2 Tr | 29.30 (95% CI: 28.54 to 30.07) | 30.1 (95% CI: 28.8 to 31.44) | 28.80 (95% CI: 29.74 to 27.90) | 0.101 | 0.024 |
| Resting SBP, mmHg Tr | 131.55 (95% CI: 127.94 to 135.27) | 139.57 (95% CI 134.39 to 144.95) | 126.74(95% CI: 122.18 to 131.46) | 0.001** | 0.099 |
| Resting DBP, mmHg | 83 (60 to 149) | 85.50 (62 to 104) | 82 (60 to 149) | 0.09 | |
| LVEF, % | 55.77 (95% CI: 54.34 to 57.20) | 57.05 (95% CI: 54.35 to 59.75) | 54.99 (95% CI: 53.35 to 56.62) | 0.167 | 0.017 |
| Resting HR, beats/min | 60 (42 to 95) | 64 (44 to 95) | 56 (42 to 91) | 0.008** |
Data are presented as mean (95% CI) unless otherwise noted. Tr = transformed using log10 transformation and reported as arithmetic mean for meaningful interpretation. BMI = kilogram per metre squared; SBP = millimetres of mercury. Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values and analysed using a non-parametric test.
BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; LVEF: left ventricular ejection fraction; HR: heart rate
p < 0.05
p < 0.01
p < 0.001
| Variable . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Sex, male/female | 100/14 (87.70% male) | 40/4 (90.0% male) | 60/10 (85.7% male) | 0.411 | |
| Age, years | 61.25 (95% CI: 59.35 to 63.14) | 63.13 (95% CI: 60.75 to 65.51) | 58.25 (95% CI: 55.21 to 61.29) | 0.012* | 0.054 |
| BMI, kg/m2 Tr | 29.30 (95% CI: 28.54 to 30.07) | 30.1 (95% CI: 28.8 to 31.44) | 28.80 (95% CI: 29.74 to 27.90) | 0.101 | 0.024 |
| Resting SBP, mmHg Tr | 131.55 (95% CI: 127.94 to 135.27) | 139.57 (95% CI 134.39 to 144.95) | 126.74(95% CI: 122.18 to 131.46) | 0.001** | 0.099 |
| Resting DBP, mmHg | 83 (60 to 149) | 85.50 (62 to 104) | 82 (60 to 149) | 0.09 | |
| LVEF, % | 55.77 (95% CI: 54.34 to 57.20) | 57.05 (95% CI: 54.35 to 59.75) | 54.99 (95% CI: 53.35 to 56.62) | 0.167 | 0.017 |
| Resting HR, beats/min | 60 (42 to 95) | 64 (44 to 95) | 56 (42 to 91) | 0.008** |
| Variable . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Sex, male/female | 100/14 (87.70% male) | 40/4 (90.0% male) | 60/10 (85.7% male) | 0.411 | |
| Age, years | 61.25 (95% CI: 59.35 to 63.14) | 63.13 (95% CI: 60.75 to 65.51) | 58.25 (95% CI: 55.21 to 61.29) | 0.012* | 0.054 |
| BMI, kg/m2 Tr | 29.30 (95% CI: 28.54 to 30.07) | 30.1 (95% CI: 28.8 to 31.44) | 28.80 (95% CI: 29.74 to 27.90) | 0.101 | 0.024 |
| Resting SBP, mmHg Tr | 131.55 (95% CI: 127.94 to 135.27) | 139.57 (95% CI 134.39 to 144.95) | 126.74(95% CI: 122.18 to 131.46) | 0.001** | 0.099 |
| Resting DBP, mmHg | 83 (60 to 149) | 85.50 (62 to 104) | 82 (60 to 149) | 0.09 | |
| LVEF, % | 55.77 (95% CI: 54.34 to 57.20) | 57.05 (95% CI: 54.35 to 59.75) | 54.99 (95% CI: 53.35 to 56.62) | 0.167 | 0.017 |
| Resting HR, beats/min | 60 (42 to 95) | 64 (44 to 95) | 56 (42 to 91) | 0.008** |
Data are presented as mean (95% CI) unless otherwise noted. Tr = transformed using log10 transformation and reported as arithmetic mean for meaningful interpretation. BMI = kilogram per metre squared; SBP = millimetres of mercury. Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values and analysed using a non-parametric test.
BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; LVEF: left ventricular ejection fraction; HR: heart rate
p < 0.05
p < 0.01
p < 0.001
The occurrence of ventilatory anaerobic threshold in relation to predicted HRR training zones, stratified by exercise modality and baseline CRF levels.
| . | Number of patients (%) . | ||
|---|---|---|---|
| Predicted HRR threshold . | Pooled cycle and treadmill . | Cycle . | Treadmill . |
| <40% predicted HRR | 51 (45.4) | 32 (76.2) | 19 (27.1) |
| 40–49% predicted HRR | 24 (21.4) | 5 (11.9) | 19 (27.1) |
| 50–59% predicted HRR | 15 (13.4) | 4 (9.5) | 11 (15.7) |
| 60–69% predicted HRR | 11 (9.8) | 0 | 11 (15.7) |
| >70% predicted HRR | 11 (9.8) | 1 (2.4) | 10 (14.3) |
| Total within 40–70% HRR | 44.6% | 21.4% | 58.5% |
| Baseline CRF category | |||
| Low fitness | Moderate fitness | High fitness | |
| <40% predicted HRR | 24 (57.1) | 23 (46) | 4 (20) |
| 40–49% predicted HRR | 11 (26.2) | 11 (22) | 2 (10) |
| 50–59% predicted HRR | 2 (4.8) | 8 (16) | 5 (25) |
| 60–69% predicted HRR | 2 (4.8) | 6 (12) | 3 (15) |
| >70% predicted HRR | 3 (7.1) | 2 (4) | 6 (30) |
| Total within 40–70% HRR | 35.8% | 50% | 50% |
| . | Number of patients (%) . | ||
|---|---|---|---|
| Predicted HRR threshold . | Pooled cycle and treadmill . | Cycle . | Treadmill . |
| <40% predicted HRR | 51 (45.4) | 32 (76.2) | 19 (27.1) |
| 40–49% predicted HRR | 24 (21.4) | 5 (11.9) | 19 (27.1) |
| 50–59% predicted HRR | 15 (13.4) | 4 (9.5) | 11 (15.7) |
| 60–69% predicted HRR | 11 (9.8) | 0 | 11 (15.7) |
| >70% predicted HRR | 11 (9.8) | 1 (2.4) | 10 (14.3) |
| Total within 40–70% HRR | 44.6% | 21.4% | 58.5% |
| Baseline CRF category | |||
| Low fitness | Moderate fitness | High fitness | |
| <40% predicted HRR | 24 (57.1) | 23 (46) | 4 (20) |
| 40–49% predicted HRR | 11 (26.2) | 11 (22) | 2 (10) |
| 50–59% predicted HRR | 2 (4.8) | 8 (16) | 5 (25) |
| 60–69% predicted HRR | 2 (4.8) | 6 (12) | 3 (15) |
| >70% predicted HRR | 3 (7.1) | 2 (4) | 6 (30) |
| Total within 40–70% HRR | 35.8% | 50% | 50% |
Predicted heart rate reserve using current guidelines, accounting for β-blockade. Baseline fitness category based on Taylor et al.28; low fitness <5 METs for women and <6 METs for men; moderate fitness 5 < 7 METs for women and 6 < 8 METs for men; high fitness ≥7 METs for women and ≥8 METs for men, where 1 MET = 3.5 mL·kg–1·min–1.
HRR, heart rate reserve. MET, metabolic equivalent
HRR: heart rate reserve; CRF: cardiorespiratory fitness; MET: metabolic equivalent
The occurrence of ventilatory anaerobic threshold in relation to predicted HRR training zones, stratified by exercise modality and baseline CRF levels.
| . | Number of patients (%) . | ||
|---|---|---|---|
| Predicted HRR threshold . | Pooled cycle and treadmill . | Cycle . | Treadmill . |
| <40% predicted HRR | 51 (45.4) | 32 (76.2) | 19 (27.1) |
| 40–49% predicted HRR | 24 (21.4) | 5 (11.9) | 19 (27.1) |
| 50–59% predicted HRR | 15 (13.4) | 4 (9.5) | 11 (15.7) |
| 60–69% predicted HRR | 11 (9.8) | 0 | 11 (15.7) |
| >70% predicted HRR | 11 (9.8) | 1 (2.4) | 10 (14.3) |
| Total within 40–70% HRR | 44.6% | 21.4% | 58.5% |
| Baseline CRF category | |||
| Low fitness | Moderate fitness | High fitness | |
| <40% predicted HRR | 24 (57.1) | 23 (46) | 4 (20) |
| 40–49% predicted HRR | 11 (26.2) | 11 (22) | 2 (10) |
| 50–59% predicted HRR | 2 (4.8) | 8 (16) | 5 (25) |
| 60–69% predicted HRR | 2 (4.8) | 6 (12) | 3 (15) |
| >70% predicted HRR | 3 (7.1) | 2 (4) | 6 (30) |
| Total within 40–70% HRR | 35.8% | 50% | 50% |
| . | Number of patients (%) . | ||
|---|---|---|---|
| Predicted HRR threshold . | Pooled cycle and treadmill . | Cycle . | Treadmill . |
| <40% predicted HRR | 51 (45.4) | 32 (76.2) | 19 (27.1) |
| 40–49% predicted HRR | 24 (21.4) | 5 (11.9) | 19 (27.1) |
| 50–59% predicted HRR | 15 (13.4) | 4 (9.5) | 11 (15.7) |
| 60–69% predicted HRR | 11 (9.8) | 0 | 11 (15.7) |
| >70% predicted HRR | 11 (9.8) | 1 (2.4) | 10 (14.3) |
| Total within 40–70% HRR | 44.6% | 21.4% | 58.5% |
| Baseline CRF category | |||
| Low fitness | Moderate fitness | High fitness | |
| <40% predicted HRR | 24 (57.1) | 23 (46) | 4 (20) |
| 40–49% predicted HRR | 11 (26.2) | 11 (22) | 2 (10) |
| 50–59% predicted HRR | 2 (4.8) | 8 (16) | 5 (25) |
| 60–69% predicted HRR | 2 (4.8) | 6 (12) | 3 (15) |
| >70% predicted HRR | 3 (7.1) | 2 (4) | 6 (30) |
| Total within 40–70% HRR | 35.8% | 50% | 50% |
Predicted heart rate reserve using current guidelines, accounting for β-blockade. Baseline fitness category based on Taylor et al.28; low fitness <5 METs for women and <6 METs for men; moderate fitness 5 < 7 METs for women and 6 < 8 METs for men; high fitness ≥7 METs for women and ≥8 METs for men, where 1 MET = 3.5 mL·kg–1·min–1.
HRR, heart rate reserve. MET, metabolic equivalent
HRR: heart rate reserve; CRF: cardiorespiratory fitness; MET: metabolic equivalent
VAT, HRR zones and CRF categories
Measured HRR (72 ± 15 beats/min) derived from maximal CPET demonstrated only a modest correlation with predicted HRR (77.99 ± 20.42 beats/min) (using current UK cardiovascular rehabilitation guidelines (r = 0.32; p = 0.001). However, the directly determined and predicted HRR/peak HR variables were significantly different from each other (mean difference = 6.74 beats/min (95% CI 2.99–10.49 beats/min) p = 0.001). The VAT occurred within 40–70% of directly determined HRR range in 61.6% of patients. In the remaining 38.4% of patients, 33.9% achieved their VAT at <40% HRR, and in 4.5% of patients their VAT did not occur until >70% HRR. For predicted HRR, VAT occurred within 40–70% HRR in 44.6% of patients. Of the remaining 55.4% of patients, 45.4% achieved VAT at <40% HRR, and 9.8% at >70% HRR (Table 2).
The VAT occurred between 40% and 70% of predicted HRR in 21.4% of patients undertaking cycling exercise. The majority (76.2%) of patients exceeded the VAT at <40% HRR. For patients undertaking CPET on a treadmill, 58.5% of patients had a VAT that occurred between 40% and 70% of predicted HRR, and 27.1% had a VAT that occurred at <40% HRR. Interestingly, the VAT occurred between 40% and 70% of predicted HRR in 35.8% of patients that were categorised as having a low CRF. VAT was exceeded at <40% of their HRR in 57.1% of patients. For higher-fitness patients, VAT occurred between 40% and 70% of predicted HRR in 50% of patients, at <40% HRR in 20%, and > 70% HRR for the remaining 30% of patients (Table 2).
Figure 1 shows the inter-quartile range for VAT as a percentage of predicted HRR, based on CRF category, and exercise testing modality. The VAT occurred at a higher percentage of VO2peak in patients with a higher CRF. This observation was also evident when CPET was conducted on a treadmill for all CRF categories, but most apparently in the moderate- and high-fitness groups.
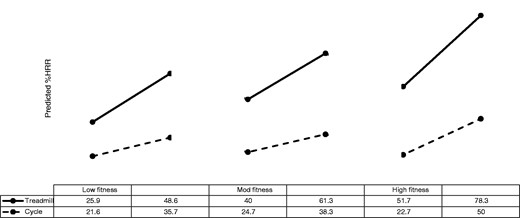
Inter-quartile range of ventilatory anaerobic threshold identification based on predicted HRR (% range) in cardiac patients separated by exercise modality and cardiorespiratory fitness (CRF) category. Predicted HRR using current guidelines, accounting for β-blockade. Baseline CRF category based on Taylor et al.28; low fitness <5 METs for women and <6 METs for men; moderate (mod) fitness 5 < 7 METs for women and 6 < 8 METs for men; high fitness ≥7 METs for women and ≥8 METs for men, where 1 MET = 3.5 mL·kg–1·min−1.
HRR: heart rate reserve; MET: metabolic equivalent
Directly measured compared with predicted CRF variables
Mean VO2peak was not significantly different between exercise modality groups in absolute units (p = 0.644; = 0.002) or relative to body mass (p = 0.359; = 0.008) (Table 3). However, absolute p = 0.027) and relative (p = 0.001) VAT was significantly different across the different CRF groups. VAT occurred at a higher percentage of predicted (p = 0.003; = 0.08) and measured VO2peak (p < 0.001; = 0.151), and HRR (p < 0.001; = 0.132) in patients exercising on the treadmill. Measured HRR (p=0.012; = 0.056) and HR at VAT (p = 0.016; = 0.052) were significantly higher in the treadmill group. There was a significant between-group difference for predicted HRmax adjusted for β-blockade (p = 0.003; Table 4). However, there was no difference in predicted HRR (p = 0.863 = <0.001) or VO2peak between groups (p = 0.815, < 0.001). Figures 2a and 2b highlight individual case studies which demonstrate how the predicted HRR method can either over- or under- estimate individualised exercise prescription versus directly determined HRR and VAT.
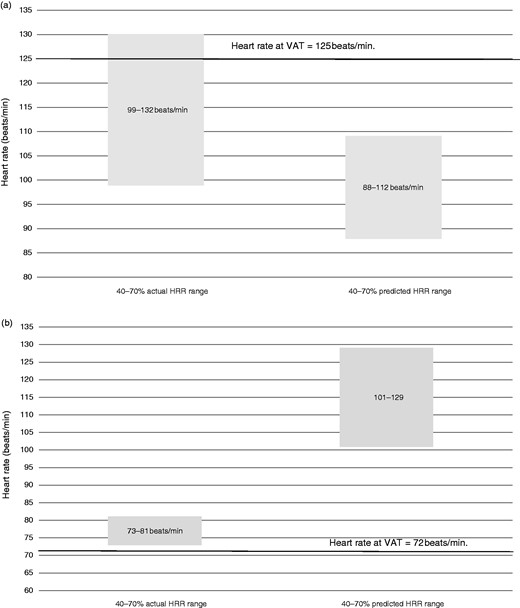
(a) A case study highlighting how the 40–70% HRR prediction equation may under-estimate individualised exercise prescription. A 58-year-old male taking β-blockers with a body mass index (BMI) of 24.8, peak oxygen uptake (VO2peak) of 35.28 mL·kg−1·min–1 in the high fitness category. Cardiopulmonary exercise test (CPET) was conducted on a treadmill. Solid line corresponds to heart rate at ventilatory anaerobic threshold, which is 125 beats/min. (b) A case study highlighting how the 40–70% HRR prediction equation may over-estimate individualised exercise prescription. A 71-year-old male not taking β-blockers with a BMI of 25.8, VO2peak of 13.82 mL·kg–1·min–1 in the low fitness category. CPET was conducted on a cycle. Solid line corresponds to heart rate at ventilatory anaerobic threshold, which is 72 beats/min.
HRR: heart rate reserve; VAT: ventilatory anaerobic threshold
Cardiorespiratory data based on maximal cardiopulmonary exercise test in patients using cycle and treadmill exercise modalities.
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| VO2peak, L·min–1 | 2.00 (95% CI: 1.88 to 2.11) | 2.03 (95% CI: 1.82 to 2.25) | 1.98 (95% CI: 1.83 to 2.12) | 0.644 | 0.002 |
| VO2peak, mL·kg–1·min–1 Tr | 22.12 (95% CI: 19.8 to 24.7) | 21.43 (95% CI: 18.0 to 25.5) | 22.55 (95% CI: 19.7 to 25.8) | 0.359 | 0.008 |
| HRmax, beats/mina | 137 (88 to 181) | 131 (88 to 181) | 139 (88 to 169) | 0.32 | |
| HRR, beats/min | 71.5 (95% CI: 67.7 to 75.4) | 65.1 (95% CI: 58.9 to 71.3) | 75.43 (95% CI: 70.69 to 80.17) | 0.009* | 0.061 |
| VAT, mL·kg–1·min–1a | 13.1 (8.2 to 29.7) | 13.3 (8.2 to 26.0) | 16.6 (8.6 to 30.0) | 0.001*** | |
| VAT, L·min–1a | 1.3 (0.7 to 2.5) | 1.15 (0.7 to 2.0) | 1.35 (0.7 to 2.5) | 0.027* | |
| HR at VAT, beats/min | 94 (95% CI: 91 to 97) | 90 (95% CI: 85 to 94) | 97 (95% CI: 93 to 101) | 0.016* | 0.05 |
| VAT, % of VO2peak | 67.5 (95% CI: 65 to 70) | 61.3 (95% CI: 58 to 65) | 71.1 (95% CI: 68 to 74) | <0.001*** | 0.151 |
| VAT, % of predicted VO2peak Tr | 56.8 (95% CI: 52 to 63) | 51.8 (95% CI: 45 to 60) | 60.1 (95% CI: 53 to 68) | 0.003** | 0.08 |
| VAT, % of HRR | 45.90 (95% CI: 43 to 49) | 39.45 (95% CI: 35.6 to 43.3) | 49.77 (95% CI: 46.5 to 53.0) | <0.001*** | 0.129 |
| VAT, % of HRmax | 71.58 (95% CI: 70.1 to 73.1) | 69.81 (95% CI: 66.9 to 72.7) | 72.64 (95% CI: 70.9 to 74.4) | 0.072 | 0.029 |
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| VO2peak, L·min–1 | 2.00 (95% CI: 1.88 to 2.11) | 2.03 (95% CI: 1.82 to 2.25) | 1.98 (95% CI: 1.83 to 2.12) | 0.644 | 0.002 |
| VO2peak, mL·kg–1·min–1 Tr | 22.12 (95% CI: 19.8 to 24.7) | 21.43 (95% CI: 18.0 to 25.5) | 22.55 (95% CI: 19.7 to 25.8) | 0.359 | 0.008 |
| HRmax, beats/mina | 137 (88 to 181) | 131 (88 to 181) | 139 (88 to 169) | 0.32 | |
| HRR, beats/min | 71.5 (95% CI: 67.7 to 75.4) | 65.1 (95% CI: 58.9 to 71.3) | 75.43 (95% CI: 70.69 to 80.17) | 0.009* | 0.061 |
| VAT, mL·kg–1·min–1a | 13.1 (8.2 to 29.7) | 13.3 (8.2 to 26.0) | 16.6 (8.6 to 30.0) | 0.001*** | |
| VAT, L·min–1a | 1.3 (0.7 to 2.5) | 1.15 (0.7 to 2.0) | 1.35 (0.7 to 2.5) | 0.027* | |
| HR at VAT, beats/min | 94 (95% CI: 91 to 97) | 90 (95% CI: 85 to 94) | 97 (95% CI: 93 to 101) | 0.016* | 0.05 |
| VAT, % of VO2peak | 67.5 (95% CI: 65 to 70) | 61.3 (95% CI: 58 to 65) | 71.1 (95% CI: 68 to 74) | <0.001*** | 0.151 |
| VAT, % of predicted VO2peak Tr | 56.8 (95% CI: 52 to 63) | 51.8 (95% CI: 45 to 60) | 60.1 (95% CI: 53 to 68) | 0.003** | 0.08 |
| VAT, % of HRR | 45.90 (95% CI: 43 to 49) | 39.45 (95% CI: 35.6 to 43.3) | 49.77 (95% CI: 46.5 to 53.0) | <0.001*** | 0.129 |
| VAT, % of HRmax | 71.58 (95% CI: 70.1 to 73.1) | 69.81 (95% CI: 66.9 to 72.7) | 72.64 (95% CI: 70.9 to 74.4) | 0.072 | 0.029 |
Tr = transformed using log10 transformation and reported as arithmetic mean for meaningful interpretation. Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values analysed using a non-parametric test.
p < 0.05
p < 0.01
p < 0.001
VO2peak: peak oxygen consumption; HRmax: maximum heart rate; HRR: heart rate reserve; VAT: ventilatory anaerobic threshold HR: heart rate
Cardiorespiratory data based on maximal cardiopulmonary exercise test in patients using cycle and treadmill exercise modalities.
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| VO2peak, L·min–1 | 2.00 (95% CI: 1.88 to 2.11) | 2.03 (95% CI: 1.82 to 2.25) | 1.98 (95% CI: 1.83 to 2.12) | 0.644 | 0.002 |
| VO2peak, mL·kg–1·min–1 Tr | 22.12 (95% CI: 19.8 to 24.7) | 21.43 (95% CI: 18.0 to 25.5) | 22.55 (95% CI: 19.7 to 25.8) | 0.359 | 0.008 |
| HRmax, beats/mina | 137 (88 to 181) | 131 (88 to 181) | 139 (88 to 169) | 0.32 | |
| HRR, beats/min | 71.5 (95% CI: 67.7 to 75.4) | 65.1 (95% CI: 58.9 to 71.3) | 75.43 (95% CI: 70.69 to 80.17) | 0.009* | 0.061 |
| VAT, mL·kg–1·min–1a | 13.1 (8.2 to 29.7) | 13.3 (8.2 to 26.0) | 16.6 (8.6 to 30.0) | 0.001*** | |
| VAT, L·min–1a | 1.3 (0.7 to 2.5) | 1.15 (0.7 to 2.0) | 1.35 (0.7 to 2.5) | 0.027* | |
| HR at VAT, beats/min | 94 (95% CI: 91 to 97) | 90 (95% CI: 85 to 94) | 97 (95% CI: 93 to 101) | 0.016* | 0.05 |
| VAT, % of VO2peak | 67.5 (95% CI: 65 to 70) | 61.3 (95% CI: 58 to 65) | 71.1 (95% CI: 68 to 74) | <0.001*** | 0.151 |
| VAT, % of predicted VO2peak Tr | 56.8 (95% CI: 52 to 63) | 51.8 (95% CI: 45 to 60) | 60.1 (95% CI: 53 to 68) | 0.003** | 0.08 |
| VAT, % of HRR | 45.90 (95% CI: 43 to 49) | 39.45 (95% CI: 35.6 to 43.3) | 49.77 (95% CI: 46.5 to 53.0) | <0.001*** | 0.129 |
| VAT, % of HRmax | 71.58 (95% CI: 70.1 to 73.1) | 69.81 (95% CI: 66.9 to 72.7) | 72.64 (95% CI: 70.9 to 74.4) | 0.072 | 0.029 |
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| VO2peak, L·min–1 | 2.00 (95% CI: 1.88 to 2.11) | 2.03 (95% CI: 1.82 to 2.25) | 1.98 (95% CI: 1.83 to 2.12) | 0.644 | 0.002 |
| VO2peak, mL·kg–1·min–1 Tr | 22.12 (95% CI: 19.8 to 24.7) | 21.43 (95% CI: 18.0 to 25.5) | 22.55 (95% CI: 19.7 to 25.8) | 0.359 | 0.008 |
| HRmax, beats/mina | 137 (88 to 181) | 131 (88 to 181) | 139 (88 to 169) | 0.32 | |
| HRR, beats/min | 71.5 (95% CI: 67.7 to 75.4) | 65.1 (95% CI: 58.9 to 71.3) | 75.43 (95% CI: 70.69 to 80.17) | 0.009* | 0.061 |
| VAT, mL·kg–1·min–1a | 13.1 (8.2 to 29.7) | 13.3 (8.2 to 26.0) | 16.6 (8.6 to 30.0) | 0.001*** | |
| VAT, L·min–1a | 1.3 (0.7 to 2.5) | 1.15 (0.7 to 2.0) | 1.35 (0.7 to 2.5) | 0.027* | |
| HR at VAT, beats/min | 94 (95% CI: 91 to 97) | 90 (95% CI: 85 to 94) | 97 (95% CI: 93 to 101) | 0.016* | 0.05 |
| VAT, % of VO2peak | 67.5 (95% CI: 65 to 70) | 61.3 (95% CI: 58 to 65) | 71.1 (95% CI: 68 to 74) | <0.001*** | 0.151 |
| VAT, % of predicted VO2peak Tr | 56.8 (95% CI: 52 to 63) | 51.8 (95% CI: 45 to 60) | 60.1 (95% CI: 53 to 68) | 0.003** | 0.08 |
| VAT, % of HRR | 45.90 (95% CI: 43 to 49) | 39.45 (95% CI: 35.6 to 43.3) | 49.77 (95% CI: 46.5 to 53.0) | <0.001*** | 0.129 |
| VAT, % of HRmax | 71.58 (95% CI: 70.1 to 73.1) | 69.81 (95% CI: 66.9 to 72.7) | 72.64 (95% CI: 70.9 to 74.4) | 0.072 | 0.029 |
Tr = transformed using log10 transformation and reported as arithmetic mean for meaningful interpretation. Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values analysed using a non-parametric test.
p < 0.05
p < 0.01
p < 0.001
VO2peak: peak oxygen consumption; HRmax: maximum heart rate; HRR: heart rate reserve; VAT: ventilatory anaerobic threshold HR: heart rate
Relation between predicted and measured variables stratified by mode of exercise.
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Predicted HRmax, adjusted for β-blockade; beats/mina | 136 (118 to 174) | 138 (126 to 174) | 134 (118 to 167) | 0.009** | |
| VAT, % of predicted HRmax adjusted for β-blockade | 67.97 (65.86 to 70.07) | 62.74 (59.68 to 65.80) | 71.10 (68.50 to 73.71) | <0.001** | 0.131 |
| Predicted HRR, adjusted for β-blockade; beats/min | 77.85 (95% CI: 75.04 to 80.66) | 77.93 (95% CI: 73.19 to 82.68) | 77.8 (95% CI: 74.24 to 81.36) | 0.965 | <0.001 |
| VAT, % of predicted HRR adjusted for β-blockadea | 40.35 (9.57 to 87.93) | 30.49 (9.57 to 69.23) | 47.06 (12 to 87.93) | <0.001*** | |
| Predicted VO2peak, mL·min–1 | 2272.14 (95% CI: 2184.11 to 2360.17) | 2258.79 (95% CI: 2114.05 to 2403.53) | 2280.35 (95% CI: 2166.68 to 2394.01) | 0.815 | <0.001 |
| VO2peak, % of predicted VO2peak | 87.85 (95% CI: 84.11 to 91.58) | 89.99 (95% CI: 82.64 to 97.35) | 86.56 (95% CI: 82.40 to 90.72) | 0.380 | 0.007 |
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Predicted HRmax, adjusted for β-blockade; beats/mina | 136 (118 to 174) | 138 (126 to 174) | 134 (118 to 167) | 0.009** | |
| VAT, % of predicted HRmax adjusted for β-blockade | 67.97 (65.86 to 70.07) | 62.74 (59.68 to 65.80) | 71.10 (68.50 to 73.71) | <0.001** | 0.131 |
| Predicted HRR, adjusted for β-blockade; beats/min | 77.85 (95% CI: 75.04 to 80.66) | 77.93 (95% CI: 73.19 to 82.68) | 77.8 (95% CI: 74.24 to 81.36) | 0.965 | <0.001 |
| VAT, % of predicted HRR adjusted for β-blockadea | 40.35 (9.57 to 87.93) | 30.49 (9.57 to 69.23) | 47.06 (12 to 87.93) | <0.001*** | |
| Predicted VO2peak, mL·min–1 | 2272.14 (95% CI: 2184.11 to 2360.17) | 2258.79 (95% CI: 2114.05 to 2403.53) | 2280.35 (95% CI: 2166.68 to 2394.01) | 0.815 | <0.001 |
| VO2peak, % of predicted VO2peak | 87.85 (95% CI: 84.11 to 91.58) | 89.99 (95% CI: 82.64 to 97.35) | 86.56 (95% CI: 82.40 to 90.72) | 0.380 | 0.007 |
Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values and analysed using a non-parametric test.
p < 0.05
p < 0.01
p < 0.001
HRmax: maximal heart rate; VAT: ventilatory anaerobic threshold; HRR: heart rate reserve; VO2Peak, peak oxygen consumption
Relation between predicted and measured variables stratified by mode of exercise.
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Predicted HRmax, adjusted for β-blockade; beats/mina | 136 (118 to 174) | 138 (126 to 174) | 134 (118 to 167) | 0.009** | |
| VAT, % of predicted HRmax adjusted for β-blockade | 67.97 (65.86 to 70.07) | 62.74 (59.68 to 65.80) | 71.10 (68.50 to 73.71) | <0.001** | 0.131 |
| Predicted HRR, adjusted for β-blockade; beats/min | 77.85 (95% CI: 75.04 to 80.66) | 77.93 (95% CI: 73.19 to 82.68) | 77.8 (95% CI: 74.24 to 81.36) | 0.965 | <0.001 |
| VAT, % of predicted HRR adjusted for β-blockadea | 40.35 (9.57 to 87.93) | 30.49 (9.57 to 69.23) | 47.06 (12 to 87.93) | <0.001*** | |
| Predicted VO2peak, mL·min–1 | 2272.14 (95% CI: 2184.11 to 2360.17) | 2258.79 (95% CI: 2114.05 to 2403.53) | 2280.35 (95% CI: 2166.68 to 2394.01) | 0.815 | <0.001 |
| VO2peak, % of predicted VO2peak | 87.85 (95% CI: 84.11 to 91.58) | 89.99 (95% CI: 82.64 to 97.35) | 86.56 (95% CI: 82.40 to 90.72) | 0.380 | 0.007 |
| . | Pooled cycle and treadmill . | Cycle . | Treadmill . | p-value . | Partial eta-squared . |
|---|---|---|---|---|---|
| Predicted HRmax, adjusted for β-blockade; beats/mina | 136 (118 to 174) | 138 (126 to 174) | 134 (118 to 167) | 0.009** | |
| VAT, % of predicted HRmax adjusted for β-blockade | 67.97 (65.86 to 70.07) | 62.74 (59.68 to 65.80) | 71.10 (68.50 to 73.71) | <0.001** | 0.131 |
| Predicted HRR, adjusted for β-blockade; beats/min | 77.85 (95% CI: 75.04 to 80.66) | 77.93 (95% CI: 73.19 to 82.68) | 77.8 (95% CI: 74.24 to 81.36) | 0.965 | <0.001 |
| VAT, % of predicted HRR adjusted for β-blockadea | 40.35 (9.57 to 87.93) | 30.49 (9.57 to 69.23) | 47.06 (12 to 87.93) | <0.001*** | |
| Predicted VO2peak, mL·min–1 | 2272.14 (95% CI: 2184.11 to 2360.17) | 2258.79 (95% CI: 2114.05 to 2403.53) | 2280.35 (95% CI: 2166.68 to 2394.01) | 0.815 | <0.001 |
| VO2peak, % of predicted VO2peak | 87.85 (95% CI: 84.11 to 91.58) | 89.99 (95% CI: 82.64 to 97.35) | 86.56 (95% CI: 82.40 to 90.72) | 0.380 | 0.007 |
Boldface values simply mean that they are significant at the P<0.05 level.
Variables are reported as median (minimum and maximum) values and analysed using a non-parametric test.
p < 0.05
p < 0.01
p < 0.001
HRmax: maximal heart rate; VAT: ventilatory anaerobic threshold; HRR: heart rate reserve; VO2Peak, peak oxygen consumption
Discussion
This study aimed to determine the accuracy of the standard UK approach for prescribing exercise in patients undertaking cardiovascular rehabilitation. This method of determining target heart rates for exercise training in cardiac patients relies largely on predictive methods for determining maximal HR (including patients taking β-blockade). We sought to compare it with a more objective measure of exercise prescription, namely the VAT derived from respiratory gas exchange during a maximal CPET. Our findings indicate that current UK cardiovascular rehabilitation exercise prescription guidelines appear susceptible to substantial inaccuracy with more than half of our cohort achieving a VAT outside the recommended target range of 40–70% HRR. We found that 45% of patients had VAT identified at <40% HRR, and in 9% of patients, VAT was identified at >70% HRR, suggesting that the required exercise intensity spectrum is wider than the recommended 40–70 HRR%.
When considering baseline cardiorespiratory fitness, the proportion of patients whose VAT occurred outside the guidelines increased, 57% of low-fitness patients achieving VAT at <40% HRR, and 30% of high-fitness patients achieving VAT at >70% HRR, confirming that VAT occurs later with increasing CRF in cardiac patients.30 For those who achieved VAT at <40% HRR, their exercise prescription may overly exceed VAT and prove too challenging, whilst for those that achieve VAT >70% HRR, their prescription is unlikely to induce a training stimulus and prove too easy. We speculate that this may contribute to the 23% attrition rate recently reported in UK cardiovascular rehabilitation,31 as some patients overly exceed their training stimulus (i.e. low-fitness patients), which may be uncomfortable, whilst some do not reach it, thus providing minimal benefit (i.e. high-fitness patients), both of which may cause patients to discontinue cardiovascular rehabilitation.
Therefore, a one size fits all approach, relying on predictive methods for maximal HR and estimated HRR to prescribe exercise, appears ineffective. Exercise prescription within cardiac rehabilitation settings needs to be more accurate, patient specific and fine-tuned, ideally based on ventilatory markers, actual HRR and baseline fitness category determined via CPET.32 One option could be to shift from ‘range-based’ to ‘threshold-based’ cardiovascular rehabilitation exercise prescription, with moderate–high intensity exercise, corresponding to work rates between VAT and critical power, being recommended.16 Based on the current data, CPET would aid prescription to ensure that all patients achieved VAT during cardiovascular rehabilitation, whilst also ensuring that it is not overly exceeded. This is important given that certain cardiac patients, namely those who may be more deconditioned, often perform activities of daily living at levels of VO2 that exceed VAT.33 Therefore, exercising in steady-state conditions above VAT is vital for these patients, but may not be possible if it is exceeded. In the late 1970s, limitations in the relative per cent method (i.e. %HRR) for prescribing exercise intensity were identified, with a study by Katch et al. showing this method failed to consider individual metabolic differences,34 yet it is still a recommended approach today.8,10 More recent investigations have proposed a more individualised exercise prescription based on ventilatory thresholds to personalise individualised training load based on metabolic responses.35,36 Recently, Weatherwax et al. reported that in sedentary adults, 12 weeks of aerobic exercise training based on an individualised exercise prescription using VAT had a greater effect on the incidence of training response compared with a standardised approach using HRR. While the exact mechanisms are still not entirely understood, it is believed that exercise intensity prescribed with the use of ventilatory thresholds takes into consideration individual metabolic characteristics which are overlooked when using relative per cent methods.37
The current data also indicate that VAT is mode-dependent for the overall cohort and across all three CRF categories. Similar to previous suggestions,16 VAT occurred at around 50% HRR on the treadmill but is 12–15% lower on the cycle. A similar relation has also been observed in patients with chronic heart failure.38 This mode dependency is also evident in terms of predicted HRR zones, which are adopted in most UK cardiovascular rehabilitation centres, with >75% of patients on a cycle ergometer achieving VAT at <40% HRR, compared with just 27% of patients exercising on a treadmill. Previous research has identified a VAT mode dependency in cardiac patients based on VO2.39 The current results differ somewhat as they show a mode dependency for patients who are yet to begin as opposed to those who have finished cardiovascular rehabilitation. Furthermore, in the current study this mode dependency is expressed using HRR, which is adopted in most cardiovascular rehabilitation centres, rather than VO2.
UK cardiovascular rehabilitation is provided by the state-funded National Health Service, unlike cardiovascular rehabilitation operating in other international and EU countries,15 and the integration of CPET equipment is not currently incorporated into most UK centres and may prove to be prohibitive.40 Another possible solution could be to increase the upper intensity limit of exercise prescription in line with international guidelines at 80% HRR, especially for patients in a higher fitness category.10,41 Of the 10 patients whose VAT occurred at >70% HRR, six achieved VAT at <80% HRR. This suggests that increasing the upper range of exercise prescription guidelines could be helpful to a small cohort of patients, and provide greater scope for training progression in those that could tolerate it; aligning UK guidelines closer to those seen internationally.42 This does not, however, address the issue for those who achieved VAT at < 40%. A further alternative to personalise exercise prescription across the whole spectrum would be to identify the HR range corresponding to an RPE of 11–13, given that VAT has been shown to occur around this point.43,44 Submaximal testing is routinely performed in UK cardiovascular rehabilitation and identification and utilisation of the HR between these points during testing could ensure that more patients are exercising at or around the VAT. One caveat to such an option is that RPE is a subjective tool, meaning that appropriate anchoring of key values would be required for each patient, and this would need to be applied consistently within and between each cardiovascular rehabilitation centre in the UK.
To be able to confidently prescribe an individualised exercise programme in a safe and effective manner can be challenging in a cardiac population. The healthcare professional must be able to account for medication usage, presence of non-cardiovascular co-morbidities and, for example, adverse events during exercise testing. Hansen and colleagues45 showed significant inter-clinician variance in prescribing exercise for patients with different cardiovascular diseases (CVDs), highlighting the challenges posed. Further training and education is key; however, digital resources are available to assist practitioner decision-making processes. For example, the European Association of Preventive Cardiology recently developed the Exercise Prescription in Everyday Practice and Rehabilitative Training (EXPERT) tool.46 The EXPERT tool is an interactive, digital training and decision support system that assists healthcare professionals in prescribing clinically effective and medically safe exercise training programmes for CVD patients. The adoption of tools such as EXPERT should be more widely encouraged and facilitated to support decision making processes around exercise prescription in cardiac populations. The impact of their utility within clinical practice could then be audited to determine changes in efficacy.
Limitations
The key limitation is that the two groups are made up of separate patients who varied on some baseline characteristics. Ideally, all patients would have completed a CPET using both modalities to reduce any individual effect.
Conclusion
To our knowledge, this is the first study of its kind to explore VAT in terms of prescribed HRR zones for cardiac patients to identify the accuracy of current UK cardiovascular rehabilitation exercise prescription guidelines. For a large proportion of patients, the guidelines are inaccurate with many patients achieving VAT at <40% HRR, meaning their exercise prescription may be overly challenging. Conversely, 30% of high-fitness patients achieved VAT at >70% HRR, meaning their prescription may be too conservative to provide a stimulus. This under/over-prescription may lead patients to unnecessarily discontinue their cardiovascular rehabilitation (see Figure 2(a) and (b)). Therefore, for UK cardiovascular rehabilitation, a one size fits all approach is ineffective and a shift from predictive equations and submaximal exercise tests to gold-standard CPET on entry to cardiovascular rehabilitation would be required to improve exercise prescription. However, this may not be viable for a number of reasons, meaning that adoption of less conservative guidelines could provide a solution to ensuring that a larger proportion of patients achieve a training stimulus. Furthermore, although VO2peak did not demonstrate a mode dependency, VAT did. This suggests that it may be necessary to conduct a CPET using both modalities, or tailor exercise prescription based on the modality used. Future research could confirm this mode dependency for HRR at VAT in cardiac patients by testing the same group of patients twice, once during each modality.
Author contribution
Both SP and SN have contributed equally to this manuscript, therefore we would like them both to be acknowledged as joint first authors. SN, SC and LI contributed to the design of the work. SN conducted data collection. SN, SB, SP and JP conducted data analysis and drafted the manuscript. SB, JP, SC, LI critically reviewed the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Sean Pymer is funded by a University of Hull PhD scholarship.




Comments