-
PDF
- Split View
-
Views
-
Cite
Cite
Jari A Laukkanen, Cardiac rehabilitation in the modern interventional cardiology era, European Journal of Preventive Cardiology, Volume 27, Issue 16, 1 November 2020, Pages 1713–1715, https://doi.org/10.1177/2047487320906304
Close - Share Icon Share
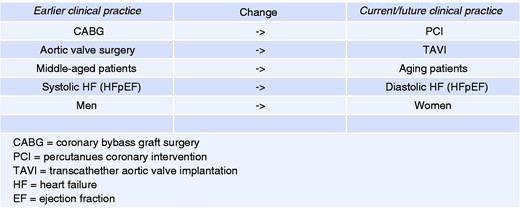
Changes in interventional cardiology, patient population and effects on cardiac rehabilitation.
Evidence-based CR should be a multidisciplinary intervention, including patient assessment, control of cardiovascular risk factors, vocational support, psychosocial management, physical activity counselling and the prescription of endurance, interval and strength exercise.4 The delivery of a comprehensive CR programme is essential to ensure favourable outcomes using cost-effective treatments. Multidisciplinary CR has remained underutilised among various aging patient groups mainly because of referral problems, poor enrollment and support, and various local reasons due to limited resources. Cardiac patients in CR programmes should be offered a comprehensive CR rehabilitation with a preferred duration of at least 6–12 weeks, consisting of one or more group-based therapies (education, exercise training, relaxation therapy with lifestyle modifications) supplemented by individual counselling when indicated. The importance of muscle strength training should not be underestimated in the elderly. Larger cohort registries on CR among elderly patients have also suggested reduced mortality or hospitalisation.4 The complexity of previous studies demonstrated a benefit of CR; it is doubtful whether these results may be reproducible in most elderly and frail patients, who represent an increasing burden of hospital care. Active participation in programmed CR among aged patients may be limited due to multiple diseases and various other reasons.
In the current issue of the European Journal of Preventive Cardiology, the large CR research team from European countries presented data on the management and treatment of patients referred from different cardiology clinics.5 European-level data stimulate more efforts to assess the effective use of CR to improve compliance with secondary prevention therapies. Although the elderly represent an increasing proportion of cardiac patients, they have usually been excluded from CR studies.6 To fulfill these research caps, the European Cardiac Rehabilitation in the Elderly project (EU-CaRE) study compared the longer-term effect of CR in aging 1633 CAD or heart valve replacement patients. The recent EU-CaRE study focused on the findings of ongoing CR programmes provided to elderly cardiac patients who were at least 65 years old at eight European study sites.5
Cardiorespiratory fitness (CRF) is a clinically useful indicator of the effectiveness of exercise-based CR during the follow-up. Oxygen consumption (VO2) declines over the years with aging, and it cannot be maintained without regular endurance exercise training. VO2peak is a strong predictor of prognosis in patients with or without diagnosed CAD.7 Irrespective of a significant genetic component of CRF, an exercise-based CR programme is a way to increase low VO2peak. The association between VO2peak and mortality has been proposed to persist across the lifespan, with a single measurement of CRF in midlife associated with the lifetime prognosis. There is a possibility that the higher mortality rates in patients with low levels of CRF are at least partly due to the severity of underlying chronic diseases associated with an increased risk of mortality (reverse causality). We have shown that a smaller decrease in CRF over the long follow-up time was associated with lower mortality rate.8 The observed association between the changes in VO2peak and mortality was independent of common risk factors assessed at baseline and 11 years later.
The assessment of CRF is one of the most important measures to assess the results of CR, in addition to conventional risk factor levels and symptoms. A meta-analysis of randomised controlled trials has concluded that there could be a mean improvement of 3–4 ml/kg/min in VO2peak after an exercise-based CR intervention.9 Greater exercise capacity in elderly patients allows them to be more active and perform activities at a higher level, including the activities of daily living. In the EU-CaRE study, the baseline VO2peak was measured in every CR centre before the start of the local CR programme. This key parameter was measured once before CR.5 Patients with symptomatic valvular heart disease, left main and/or three-vessel CAD and low ejection fraction have usually more symptoms and they are physically inactive.
Previous findings support current clinical practice guidelines that recommend the control of multiple risk factors to optimise secondary prevention in patients with CAD.10 Unfortunately, only a proportion of CAD patients will achieve all target levels in risk factor control and lifestyle recommendations. Although some risk factors may be more strongly associated with survival than others, all of them contribute to future survival. During CR, the proportion of CAD patients with three or more uncontrolled risk factors declined from 58.4% at baseline to 40.1% at 12 months.5 Despite significant improvements, however, many CAD patients still had three or more risk factors that were not at the target level after one year.5 There would still be an urgent demand to decrease common risk factors and improve prognosis. Better survival is not predicted only by the number of risk factors at goal but by the degree to which individual risk factors were controlled, as shown in the COURAGE follow-up study.10
In the EU-CaRE study, VO2peak with cardiovascular risk factor and body composition, diet, physical activity, psychological distress and medication were properly assessed before and after the 12-month CR period.5 Psychological distress scores improved and adherence to medication was good. VO2peak levels may partly be explained by the timing of participation. Patients undergoing coronary artery bypass grafting (CABG) or heart valve replacement had lower VO2peak at baseline, with a greater increase during the CR period and 12 months later (2.8 and 4.3 ml/kg/min, respectively) than patients with PCI and stable angina (1.6 and 1.4 ml/kg/min, respectively). The differences in CR timing such as the time delay from an index event to the start of CR may have an effect on VO2peak levels, which is contributed to by the phase of the recovery process. Among surgically treated patients, baseline VO2peak is usually low, which is likely attributable to the impact of disease severity before the operation. Due to extensive CAD or serious valvular disease, CABG or valvular surgery may have been preferred instead of PCI and/or transcatheter aortic valve implantation. Second, the recent study showed that the time from the index cardiac event to the start of CR may vary with the total duration of the CR programme (from 20 to 125 days). Third, there were variations in the number of weekly training sessions (from two to five) and the type of guidance of CR (inhospital vs. ambulatory).5 Harmonisation of the available CR programmes would be needed so that evidence-based therapies could be effectively implemented in current fast-paced clinical practice.
CR produces economic savings and better adherence to medical therapies in addition to lowered hospitalisation and improved quality of life. CR should be formulated according to national healthcare systems. This EU-level CR study is warmly welcomed in the modern interventional cardiology era among older patient groups. We commend the authors and are waiting for results from ongoing CR projects to implement these findings in real-life clinical practice. Further research is needed to identify more effective CR strategies to sustain healthy behaviours and the attainment of other risk factor goals to improve long-term survival.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.




Comments