-
PDF
- Split View
-
Views
-
Cite
Cite
Xavier Trudel, Chantal Brisson, Mahée Gilbert-Ouimet, Caroline S Duchaine, Violaine Dalens, Denis Talbot, Alain Milot, Masked hypertension incidence and risk factors in a prospective cohort study, European Journal of Preventive Cardiology, Volume 26, Issue 3, 1 February 2019, Pages 231–237, https://doi.org/10.1177/2047487318802692
Close - Share Icon Share
Abstract
Masked hypertension may affect up to 30% of the general population and is associated with a high cardiovascular disease risk. No previous study has examined the incidence of masked hypertension and its risk factors. The study aim was to determine the incidence of masked hypertension and to examine its related risk factors.
This is a cohort study including 1836 initially normotensive participants followed up on average for 2.9 years. Blood pressure was measured using Spacelabs 90207. Manual blood pressure was defined as the mean of the first three readings taken at rest. Ambulatory blood pressure was defined as the mean of the next readings recorded every 15 minutes during daytime working hours. Masked hypertension incidence at follow-up was defined as manual blood pressure less than 140 and less than 90 mmHg and ambulatory blood pressure at least 135 or at least 85 mmHg. Generalised estimating equations were used.
The cumulative incidence of masked hypertension was 10.3% and was associated with male gender (relative risk (RR) 1.51, 95% confidence interval (CI) 1.18–1.94), older age (RR40–49 years 1.56, 95% CI 1.16–2.11, RR≥50 years 1.50, 95% CI 1.06–2.10), higher education (RRcollege 1.31, 95% CI 1.03–1.65), body mass index (RR≥27 1.43, 95% CI 1.11–1.85), smoking (RR 1.51, 95% CI 1.09–2.010) and alcohol intake (RR≥6/week 1.65, 95% CI 1.13–2.03).
The present study is the first to identify risk factors for the incidence of masked hypertension. Current guidelines for hypertension detection recommend ambulatory blood pressure in patients with an elevated blood pressure reading at the clinic. As it is impractical to measure ambulatory blood pressure in all normotensive patients, factors identified in the present study should be considered for the screening of at-risk individuals and for primary prevention of masked hypertension.
Introduction
The diagnosis of hypertension is traditionally based on office blood pressure (OBP) performed at the clinic. Ambulatory blood pressure (ABP) has refined the classification of hypertension into four categories: normotension, white coat hypertension, masked hypertension and sustained hypertension.1–3 Masked hypertension refers to the condition defined by normal OBP (less than 140 and less than 90 mmHg) combined with elevated daytime ABP (at least 135 or at least 85 mmHg).1, 4 Masked hypertension is a major challenge for the diagnosis and management of patients with hypertension.5 While masked hypertension has been associated with an increased cardiovascular risk comparable to that of sustained hypertension,6–8 results recently published from a cohort including 63,910 adults suggest that masked hypertension is even more strongly associated with all-cause and cardiovascular mortality than sustained hypertension.9
In the general population, the prevalence of masked hypertension has been observed to range from 8% to 30%.6 This prevalence varies according to the population characteristics and the methods used to measure OBP and ABP.3 Previous cross-sectional studies have reported a higher prevalence of masked hypertension with male gender, obesity, smoking and excessive alcohol intake5, 6, 10, 11 while the effect of age showed mixed results.10, 12 Whether or not these risk factors, based on prevalence data, are true contributors to masked hypertension incidence remains unknown. Primary prevention, aiming to reduce the burden of masked hypertension in the general population, should rely on true risk factors obtained from incidence data allowing for the early identification of at-risk patients before disease onset. No previous studies have provided estimations of the incidence of masked hypertension and examined its risk factors.
The objectives of the present study were to determine the incidence of masked hypertension and to examine the effect of sociodemographic and lifestyle-related risk factors on the incidence of masked hypertension, using a prospective cohort from Quebec City, Canada.
Methods
Population and study design
The design is a prospective dynamic cohort study. This cohort has been described elsewhere.13, 14 The study population was composed of all white collar workers from three large public insurance institutions in Canada. These organisations were chosen because they tend to have comparable activities as all three deliver insurance services to the general population. Their jobs encompassed the full range of white collar positions, including senior and middle managers, professionals and technicians and office workers. Participants completed a self-administered questionnaire including sociodemographics, cardiovascular disease (CVD) and blood pressure (BP) risk factors and several work characteristics. They were assessed three times during a 5-year period (years 0, 3 and 5). The participation rate was 80.9% at baseline and 85% at both follow-ups. The study sample was composed of all participants who: (a) were initially normotensive; (b) were working in one of the organisations at their baseline assessment; and (c) had their BP assessed at the subsequent measurement time. New workers at the first follow-up (year 3) as well as workers who changed work or retired after baseline were eligible and were included in the study. Participants with insufficient ambulatory BP measurements (less than 20) were excluded (N = 16), in accordance with criteria recently recommended by expert committees.15 The final study sample was composed of 1836 initially normotensive individuals.
BP measurements
BP was measured using the Spacelabs 90207 oscillometric monitor (Spacelabs Produits Médicaux Lté, St-Laurent, Quebec, Canada) validated by the independent investigators' protocol, recommended by the Association for the Advancement of Medical Instrumentation and British Hypertension Society.16, 17 In a research office at the participant's workplace, the device was fitted on the non-dominant arm if BP difference measured on both arms was less than 10 mmHg. Otherwise, it was fitted on the arm showing the higher BP level. After the participant had been sitting for 5 minutes, BP was measured three times in the presence of trained personnel using the office check mode of the Spacelabs monitor. Then, BP was measured every 15 minutes by the same monitor for the rest of the working day. All devices were fitted to participants at the same time of day (08:00 hours) and monitoring was conducted over regular daytime working hours (08:00 to 16:00) in all cases. Participants were white collar workers whose tasks were mainly achieved in a sitting position. To minimise motion artefact, clear instructions were given to participants in the case when the monitor performed a reading while they were in a standing position (stop walking with their arm resting at their side).
Manual blood pressure (MBP) was defined as the mean of the first three readings taken at rest in the presence of trained personnel. ABP was defined as the mean of the next readings taken every 15 minutes and recorded by the same monitor during regular work (daytime ABP).
Participants were classified into four categories according to the European Society of Hypertension guidelines:18 normotension, in which MBP was less than 140 and less than 90 mmHg and ABP was less than 135 and less than 85 mmHg; white coat hypertension, in which MBP was at least 140 or at least 90 mmHg and ABP was less than 135 and less than 85 mmHg; masked hypertension, in which MBP was less than 140 and less than 90 mmHg and ABP was at least 135 or at least 85 mmHg; and sustained hypertension, in which MBP was at least 140 or at least 90 mmHg and ABP was at least 135 or at least 85 mmHg. Participants treated for hypertension were classified as sustained hypertensive individuals. Participants were systematically informed about their hypertensive status and referred to their physician when their ABP values were compatible with the diagnosis of hypertension.
Sociodemographic and lifestyle-related risk factors
Sociodemographic factors included gender, age (<40, 40–49, ≥ 50 years) and education (less than college, college completed). Lifestyle-related risk factors included current cigarette smoking status, body mass index (BMI) and alcohol intake. Smoking status was defined as the daily consumption of at least one cigarette per day. Body weight and height were measured to calculate BMI (kg/m2) which was categorised using the following categories: less than 25, 25–29.9 and 30 kg/m2 or greater. Alcohol intake was measured using the following three categories, related to weekly intake frequency during the past 12 months: less than one drink per week, one to five drinks per week and six and more drinks per week. A family history of CVD was also considered. The definition of the latter group was based on the declaration by the participant of a cardiovascular event, such as angina, myocardial infarction, coronary revascularisation or stroke, experienced by their father, mother, brother or sister before the age of 60 years. The risk factors listed above were evaluated using validated protocols.19, 20
Analyses
We used cross-lagged models to examine whether cardiovascular risk factors assessed among initially normotensive participants were associated with the incidence of masked and sustained hypertension at the next measurement time. Generalised estimating equations with a Poisson distribution and an independent correlation matrix were used to examine the association between each risk factor and the incidence of hypertension.21 Generalised estimating equations are well suited for analyses of dynamic populations, as they accommodate new participants' in-migration and within-subject correlation due to repeated observations, leading to increased sample size and study power. Participants were included in one (N = 1067) or two (N = 769) longitudinal samples, the latter being for those who remained normotensive at the first follow-up. The total number of observations in the pooled sample was 2605. The incidence of masked hypertension was calculated using the number of observations as the denominator. Cumulative incidence ratios of masked and sustained hypertension were computed with 95% confidence intervals (CIs). Models were adjusted for all included risk factors and for sample affiliation, to take into account the length of follow-up. No interaction was found for gender. The main results are presented separately for men and women in the Appendix (Supplementary Table 1). SAS 9.4 software was used for all analyses.22 This study was approved by the ethical review board of the CHU de Québec.
Results
Table 1 presents the characteristics of the study sample at baseline. About two-thirds were women. The mean age was 43.1 years (standard deviation (SD) 8.1). About half were aged between 40 and 49 years. The mean BMI was 25.4 (SD 4.4). A high BMI (≥27 kg/m2) was present among 30% of the study sample, 10% were smokers and 22% consumed more than six alcohol drinks per week. Table 2 presents the hypertension classification at follow-up among these initially normotensive participants. The cumulative incidence of masked hypertension was 10.3% and was higher in men (13.8%) when compared to women (8.4%). Fewer participants transitioned to white coat (1.0%) or to sustained (4.1%) hypertension. Among sustained hypertensive individuals, 36.4% were treated for hypertension. Among those treated participants, 23% had uncontrolled ABP, i.e. ABP at least 135 or at least 85 mmHg.
| . | N (%) . |
|---|---|
| Gender | |
| Women | 1722 (66.1) |
| Men | 883 (33.9) |
| Age, years | |
| <40 | 763 (29.3) |
| 40–49 | 1247 (47.9) |
| ≥50 | 595 (22.8) |
| Body mass index (kg/m2) | |
| <25 | 1386 (53.2) |
| 25–26.9 | 443 (17.0) |
| ≥27 | 776 (29.8) |
| Education | |
| Less than college | 596 (22.9) |
| College | 863 (33.1) |
| University | 1146 (44.0) |
| Family history of CVD (yes) | 779 (29.9) |
| Alcohol intake | |
| <1/week | 873 (33.5) |
| 1–5/week | 1160 (44.5) |
| ≥6/week | 572 (22.0) |
| Smoking status (yes) | 272 (10.4) |
| Mean manual BP (mmHg, SD) | |
| Systolic | 118.6 (8.9) |
| Diastolic | 73.5 (6.5) |
| Mean ambulatory BP (mmHg, SD) | |
| Systolic | 119.6 (7.4) |
| Diastolic | 76.2 (5.3) |
| . | N (%) . |
|---|---|
| Gender | |
| Women | 1722 (66.1) |
| Men | 883 (33.9) |
| Age, years | |
| <40 | 763 (29.3) |
| 40–49 | 1247 (47.9) |
| ≥50 | 595 (22.8) |
| Body mass index (kg/m2) | |
| <25 | 1386 (53.2) |
| 25–26.9 | 443 (17.0) |
| ≥27 | 776 (29.8) |
| Education | |
| Less than college | 596 (22.9) |
| College | 863 (33.1) |
| University | 1146 (44.0) |
| Family history of CVD (yes) | 779 (29.9) |
| Alcohol intake | |
| <1/week | 873 (33.5) |
| 1–5/week | 1160 (44.5) |
| ≥6/week | 572 (22.0) |
| Smoking status (yes) | 272 (10.4) |
| Mean manual BP (mmHg, SD) | |
| Systolic | 118.6 (8.9) |
| Diastolic | 73.5 (6.5) |
| Mean ambulatory BP (mmHg, SD) | |
| Systolic | 119.6 (7.4) |
| Diastolic | 76.2 (5.3) |
BP: blood pressure; CVD: cardiovascular disease; SD: standard deviation.
| . | N (%) . |
|---|---|
| Gender | |
| Women | 1722 (66.1) |
| Men | 883 (33.9) |
| Age, years | |
| <40 | 763 (29.3) |
| 40–49 | 1247 (47.9) |
| ≥50 | 595 (22.8) |
| Body mass index (kg/m2) | |
| <25 | 1386 (53.2) |
| 25–26.9 | 443 (17.0) |
| ≥27 | 776 (29.8) |
| Education | |
| Less than college | 596 (22.9) |
| College | 863 (33.1) |
| University | 1146 (44.0) |
| Family history of CVD (yes) | 779 (29.9) |
| Alcohol intake | |
| <1/week | 873 (33.5) |
| 1–5/week | 1160 (44.5) |
| ≥6/week | 572 (22.0) |
| Smoking status (yes) | 272 (10.4) |
| Mean manual BP (mmHg, SD) | |
| Systolic | 118.6 (8.9) |
| Diastolic | 73.5 (6.5) |
| Mean ambulatory BP (mmHg, SD) | |
| Systolic | 119.6 (7.4) |
| Diastolic | 76.2 (5.3) |
| . | N (%) . |
|---|---|
| Gender | |
| Women | 1722 (66.1) |
| Men | 883 (33.9) |
| Age, years | |
| <40 | 763 (29.3) |
| 40–49 | 1247 (47.9) |
| ≥50 | 595 (22.8) |
| Body mass index (kg/m2) | |
| <25 | 1386 (53.2) |
| 25–26.9 | 443 (17.0) |
| ≥27 | 776 (29.8) |
| Education | |
| Less than college | 596 (22.9) |
| College | 863 (33.1) |
| University | 1146 (44.0) |
| Family history of CVD (yes) | 779 (29.9) |
| Alcohol intake | |
| <1/week | 873 (33.5) |
| 1–5/week | 1160 (44.5) |
| ≥6/week | 572 (22.0) |
| Smoking status (yes) | 272 (10.4) |
| Mean manual BP (mmHg, SD) | |
| Systolic | 118.6 (8.9) |
| Diastolic | 73.5 (6.5) |
| Mean ambulatory BP (mmHg, SD) | |
| Systolic | 119.6 (7.4) |
| Diastolic | 76.2 (5.3) |
BP: blood pressure; CVD: cardiovascular disease; SD: standard deviation.
Cumulative incidence of white coat, masked and sustained hypertension among initially normotensive in a prospective cohort study, Quebec City, Canada.
| . | White coat hypertension . | Masked hypertension . | Sustained hypertension . |
|---|---|---|---|
| . | % (N/total) . | % (N/total) . | % (N/total) . |
| Men | 1.5 (13/883) | 13.8 (122/883) | 5.3 (47/883) |
| Women | 0.8 (14/1722) | 8.4 (145/1722) | 3.5 (60/1722) |
| Overall | 1.0 (27/2605) | 10.3 (267/2605) | 4.1 (107/2605) |
| . | White coat hypertension . | Masked hypertension . | Sustained hypertension . |
|---|---|---|---|
| . | % (N/total) . | % (N/total) . | % (N/total) . |
| Men | 1.5 (13/883) | 13.8 (122/883) | 5.3 (47/883) |
| Women | 0.8 (14/1722) | 8.4 (145/1722) | 3.5 (60/1722) |
| Overall | 1.0 (27/2605) | 10.3 (267/2605) | 4.1 (107/2605) |
Cumulative incidence of white coat, masked and sustained hypertension among initially normotensive in a prospective cohort study, Quebec City, Canada.
| . | White coat hypertension . | Masked hypertension . | Sustained hypertension . |
|---|---|---|---|
| . | % (N/total) . | % (N/total) . | % (N/total) . |
| Men | 1.5 (13/883) | 13.8 (122/883) | 5.3 (47/883) |
| Women | 0.8 (14/1722) | 8.4 (145/1722) | 3.5 (60/1722) |
| Overall | 1.0 (27/2605) | 10.3 (267/2605) | 4.1 (107/2605) |
| . | White coat hypertension . | Masked hypertension . | Sustained hypertension . |
|---|---|---|---|
| . | % (N/total) . | % (N/total) . | % (N/total) . |
| Men | 1.5 (13/883) | 13.8 (122/883) | 5.3 (47/883) |
| Women | 0.8 (14/1722) | 8.4 (145/1722) | 3.5 (60/1722) |
| Overall | 1.0 (27/2605) | 10.3 (267/2605) | 4.1 (107/2605) |
Figure 1 presents the adjusted cumulative incidence ratios of masked hypertension. After adjustment for sample affiliation and mutual adjustment for all examined risk factors, male gender (relative risk (RR) 1.51, 95% CI 1.18–1.94), older age (RR40–49 years 1.56, 95% CI 1.16–2.11, RR≥50 years 1.50, 95% CI 1.06–2.10); higher education (RRcollege 1.31, 95% CI 1.03–1.65), BMI (RR≥27 1.43, 95% CI 1.11–1.85), smoking (RR 1.51, 95% CI 1.09–2.10) and alcohol intake (RR1–5/week 1.52, 95% CI 1.13–2.03, RR≥6/week 1.65, 95% CI 1.13–2.03) were associated with a higher incidence of masked hypertension. Participants with a family history of CVD had a higher incidence of masked hypertension but this association was not statistically significant.
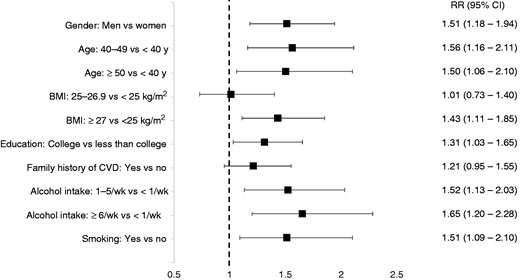
Cumulative incidence of masked hypertension by risk factors in a prospective cohort, Quebec City, Canada. RR: relative risk; BMI: body mass index (kg/m2); CVD: cardiovascular disease. Adjusted for length of follow-up and mutual adjustment for all listed risk factors.
Figure 2 presents the adjusted cumulative incidence ratios of sustained hypertension. Older age was strongly associated with the incidence of sustained hypertension (RR40–49 years 3.02, 95% CI 1.63–5.59, RR≥50 years 3.52, 95% CI 1.84–6.72). BMI (RR≥27 2.12, 95% CI 1.40–3.21) and smoking (RR 1.82, 95% CI 1.11–2.98) were also associated with the incidence of sustained hypertension. Men were at higher risk of developing sustained hypertension although this association was not statistically significant.
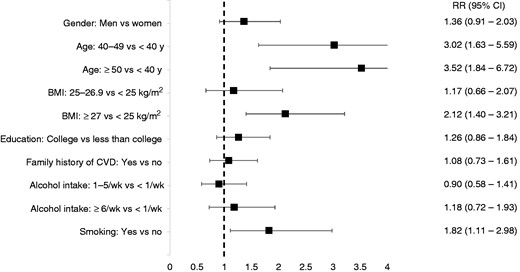
Cumulative incidence of sustained hypertension by risk factors in a prospective cohort, Quebec City, Canada. RR: relative risk; BMI: body mass index (kg/m2); CVD: cardiovascular disease. Adjusted for length of follow-up and mutual adjustment for all listed risk factors.
Discussion
In this prospective study conducted among middle aged normotensive workers, the cumulative incidence of masked hypertension was 10.3% over a mean follow-up of 2.9 years. The present study showed that male gender, older age, higher education, BMI, alcohol intake and smoking are associated with a higher incidence of masked hypertension. Previous studies have documented factors associated with the prevalence of masked hypertension, including one conducted by our research team among workers from the same organisations.11 These cross-sectional studies did not take into account the temporal ordering of the relationship and therefore had limited capacity to identify true contributors of masked hypertension development, which can only be measured with incidence data. The present study identified, for the first time, risk factors for the incidence of masked hypertension.
High screening BP was the only significant predictor of future masked hypertension in one previous study examining predictors of masked hypertension in 100 young men who either had normal (n = 28) or high (n = 72) screening BP.23 This previous study has limitations, including the restriction to men, the relatively small sample size and an overrepresentation of pre-hypertensive individuals. Most importantly, masked hypertension at follow-up was assessed for all participants, including those with no information on baseline ambulatory measurements, limiting the selection of a healthy cohort (free of masked hypertension) and consequently hindering the examination of ‘true’ incidence over time. Our study, conducted among a large prospective sample of men and women overcome these limitations and showed that gender, age, education and lifestyle-related risk factors are associated with the incidence of masked hypertension. Our results add crucial information to identify at-risk patients, who may benefit from ABP monitoring.
In our study, the incidence of masked hypertension was higher in men when compared to women. This result is consistent with previous prevalence studies.10 As hypertension develops later in women when compared to men, the middle aged composition of our cohort could explain this finding.24 Gender differences have been observed in the impact of masked hypertension on arterial structure and function with masked hypertensive women showing greater arterial wall stress and an increase in central pressure.25 Analysis of gender differences in the effect of masked hypertension on all-cause and CVD mortality showed a similar risk for men and women in a recently published cohort study.9 Therefore, early screening for masked hypertension should be considered in both genders. Our findings also pointed to increasing age as a major risk factor for the incidence of masked hypertension. Previous studies have not provided consistent results when examining the association of age with masked hypertension prevalence.10, 12 Some studies showed that the prevalence of masked hypertension was higher among older participants while others found the opposite.12 Methodological issues including the use of cross-sectional designs as well as differences in the assessment of MBP and ABP could explain these mixed findings. In our study, older age was clearly associated with the incidence of both masked and sustained hypertension, although the effects were of higher magnitude for sustained hypertension.
Our findings also showed a higher incidence of masked hypertension in participants with higher education. This finding is not consistent with the social gradient in CVD health, a well-documented and empirically supported phenomenon in which individuals with lower socioeconomic status are at increased CVD risk.26 In our study, the higher incidence of masked hypertension among participants with a higher education level could be explained by shared work characteristics. Supporting this hypothesis, one previous study showed that jobs characterised by high psychological demands and high job control were associated with masked hypertension prevalence in men.27 Factors not assessed in the office but eliciting BP elevation during daytime therefore could be important contributors. Future studies are needed to examine these underlying mechanisms.
In the present study, high BMI, smoking and alcohol intake were strongly associated with the incidence of masked hypertension, providing further support to consider lifestyle-related risk factors in efforts to prevent and detect masked hypertension.6 Previous evidence on BMI and masked hypertension had a potential for reverse causality due to the cross-sectional design.11, 28–30 Indeed, the presence of hypertension could have resulted in metabolic changes leading to weight gain.31 The present study showed, for the first time, a robust effect of high BMI on masked hypertension development. Our findings also suggest that among these lifestyle-related risk factors, alcohol intake could be of particular importance to identify normotensive individuals at risk of future out-of-office BP elevation. Indeed, high alcohol intake was positively associated with the incidence of masked hypertension but not with the incidence of sustained hypertension. The timing of BP measurements after alcohol drinking may influence the direction of BP change.32 Indeed, alcohol intake can lead to early BP reductions, followed by a later rise, about 10–15 hours after ingestion. MBP was assessed at the beginning of the work day and could have been reduced by this vasodepressor effect given that alcohol is usually drunk during the evening. On the other hand, the later rise in BP could have been captured by ABP assessed over the work day.
MBP and ABP were measured using the same device, in the same environmental setting (i.e. the workplace). The use of this particular method and its consequence on hypertension classification were discussed elsewhere.11 Briefly, the prevalence of masked hypertension (15%) remained in the range of previous studies.10 It should also be mentioned that there are important differences in methods used to measure OBP (clinical) in previous studies, related to the number of measurements and the equipment used (automatic oscillometric device vs. mercury sphygmomanometer), which could also influence masked hypertension prevalence estimates. The present study showed that the incidence of masked hypertension is common when measured using the same validated oscillometric device for both MBP and ABP.
This study has limitations. First, daytime ambulatory BP was used, limiting the examination of nocturnal hypertension. However, the majority of population-based studies on masked hypertension have used daytime ABP measurements.7 Therefore, the use of daytime BP favours comparability with previous studies and is in accordance with current guidelines for the definition of masked hypertension.33 A recently published cohort study showed that all ABP components (24-hour, daytime and night time) similarly increased the risk of death.9 A second limitation is related to the fact that our cohort was composed of white collar workers, so results may not generalise to other populations. Further research is needed to investigate the extent to which our findings are generalisable to other populations.
This study also has important strengths including being the first prospective cohort study examining the incidence of masked hypertension and its related risk factors among initially normotensive individuals. Other strengths include its high participation rate at each time and its sizeable sample size, for both genders. Finally, the present study examined the incidence of masked hypertension using a cross-lagged analysis of pooled samples, to maximise sample size and make an efficient use of this dynamic prospective cohort.
The present study showed that male gender, older age, higher education, BMI, smoking and alcohol intake are risk factors for the incidence of masked hypertension and remained robustly associated with the condition after mutual adjustment. As it is impractical to measure ABP in all patients with normal BP in the clinic, these risk factors should be considered for the screening of individuals at risk of developing masked hypertension and in primary prevention efforts.
Author contribution
XT supervised and synthesised the data analyses and led the writing. CB originated and supervised all aspects of the study. AM supervised the aspects of the study related to blood pressure measurement and interpretation. MGO and CSD led the literature review and supervised aspects related to occupational epidemiology. VD was involved in clinical issues. DT was involved in the data analyses. All the authors participated in reviewing and drafting the manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this research was supported by a grant from the Canadian Institutes of Health Research (CIHR) (57750).




Comments