-
PDF
- Split View
-
Views
-
Cite
Cite
Edward Lin, Cindy H Nguyen, Scott G Thomas, Completion and adherence rates to exercise interventions in intermittent claudication: Traditional exercise versus alternative exercise – a systematic review, European Journal of Preventive Cardiology, Volume 26, Issue 15, 1 October 2019, Pages 1625–1633, https://doi.org/10.1177/2047487319846997
Close - Share Icon Share
Abstract
Intermittent claudication, defined as fatigue or pain in the legs while walking, is a common symptom in peripheral arterial disease. Although exercise effectively improves function and manages symptoms, adherence rates are not ideal. The high levels of pain experienced in traditional exercise programmes may explain the suboptimal adherence. Alternative modalities of exercise can elicit similar benefits to traditional walking exercise. The purpose of this systematic review was to compare completion and adherence rates of exercise programmes in traditional exercise interventions versus alternative exercise interventions among patients with intermittent claudication.
Systematic review.
The electronic databases of Medline, SPORTDiscus and CINAHL were searched from the earliest records to March 2018. Search terms were based on ‘peripheral artery disease’ and ‘exercise’. Studies were included if they involved structured exercise and explicitly reported the number of participants that commenced and completed the programme.
The search identified 6814 records based on inclusion criteria. Eighty-four full-text records were reviewed in further detail. Out of the 84 studies, there was a total of 122 separate exercise groups, with 64 groups of ‘traditional walking exercise’ and 58 groups of ‘alternative exercise’. Completion and adherence rates for traditional exercise were 80.8% and 77.6%, respectively. Completion and adherence rates for alternative exercise were 86.6% and 85.5%, respectively.
The use of alternative modalities of exercise, which have been proved to be as effective as traditional exercise, may offer a solution to the poor participation and adherence rates to exercise in this population.
Introduction
Peripheral arterial disease (PAD) is a progressive disease involving occlusion in the arteries of the legs.1 It is caused by atherosclerosis and results in a reduction of blood flow and oxygen delivery to the lower limbs, and impairments in skeletal muscle function.2 From 2000 to 2010, the number of cases of PAD worldwide increased by 24% to 200 million.3 As expected for an atherosclerotic disease, the prevalence of PAD increases with age. The hallmark symptom of PAD is intermittent claudication (IC) which occurs in 30% of those with PAD.4 IC is characterised by fatigue, cramping or pain in the muscles of the lower limbs on prolonged physical exertion, and contributes significantly to the physical limitations present in this population and resultant poor quality of life.5,6 PAD is associated with various comorbidities including diabetes mellitus, dyslipidemia, hypertension, and other forms of cardiovascular disease.7
Treatment of PAD involves medication, revascularisation and/or exercise.8 The primary objectives of treatment are to reduce the high risk of cardiovascular disease events, improve symptoms, and to enhance quality of life through improving functional capacity. Exercise interventions are highly recommended for this patient population (class of recommendation: I, level of evidence: A) as a first-line treatment.8 Exercise is effective in improving functional capacity, as measured through maximum walking distance and pain-free walking distance, and enhancing quality of life.9
The earliest meta-analysis on exercise rehabilitation programmes for treating claudication was conducted in 1995.10 The authors found that exercise programmes were more effective if the programme involved walking instead of a combination of exercises, patients exercised to near-maximal pain, and the duration of the programme was greater than or equal to 26 weeks. Even through this review only included three randomised controlled trials (RCTs), exercise interventions and clinical guidelines have predominantly modelled their exercise recommendations based on this meta-analysis.
Recent reviews have indicated that walking to maximal pain may not be necessary to induce significant improvements in functional outcomes.11,12 Alternative modalities of exercise have been identified and evidence has shown that they are capable of eliciting similar benefits compared to traditional walking exercise. These modalities include pain-free treadmill exercise,13 lower limb aerobic exercise,14 polestriding (Nordic walking),15 arm ergometry,16 resistance training17 and circuit training.18
Despite the plethora of research indicating the effectiveness of exercise as a treatment method for IC, adherence rates are far from ideal. A systematic review on the uptake and adherence rates to supervised exercise programmes among patients with IC found that one of the main reasons for poor adherence was lack of motivation.19 Pain was suggested to be a contributing factor for low motivation. As the current recommendations involve walking to moderate to severe pain multiple times per session, patients may understandably be discouraged from exercising. In fact, some patients reported avoiding exercise altogether due to a lack of understanding regarding its benefits. One study found patients avoided exercise due to fear that it may worsen their condition.20 The majority of these patients believed that exercise causes claudication, worsens pain and is harmful to their legs. Thus the traditional walking exercise prescription may actually deter patients from performing exercise.
The purpose of this systematic review was to compare the completion and adherence rates to exercise programmes in traditional exercise interventions versus alternative exercise interventions for patients with IC-associated PAD.
Methods
The review was conducted in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.21
Search strategy
A systematic review of RCTs and non-RCTs was performed. An electronic database search was conducted using Medline, SPORTDiscus and CINAHL. The search was limited to titles and abstracts published in the English language. All databases were searched from the earliest record to March 2018. The search strategy included trials with supervised or unsupervised exercise interventions. Search terms were variants of ‘peripheral artery disease’ and ‘exercise’ and limited to titles and abstracts. Search terms were: ‘peripheral arter* disease’ OR ‘peripheral vascular disease’ OR ‘claudication’ OR ‘peripheral occlusive disease’ AND ‘exercise’ OR ‘train*’ OR ‘aerobic’ OR ‘resist*’ OR ‘program’ OR ‘walking’ OR ‘intervention’ OR ‘rehab*’ OR ‘supervised’ OR ‘physical activity’ OR ‘strength’ OR ‘fitness’ OR ‘walk*’ OR ‘raise’ OR ‘ergometry’ OR ‘treadmill’ OR ‘plantar flexion’ OR ‘sport’.
Study selection
Studies were included if they met the following criteria: (a) a study (RCT, controlled or pre-post design) that involved any form of structured exercise (supervised or unsupervised) for patients with intermittent claudication; (b) explicit statement of number of participants that commenced and completed the exercise intervention; and (c) exercise intervention in the study had a minimum duration of 4 weeks. Determination of study inclusion and data extraction was performed by EL and CHN (first and second author, respectively).
Data extraction and quality assessment
Quality assessment was performed using the physiotherapy evidence database scale (PEDro). Points were only rewarded if the categories were clearly satisfied.
Data extracted included: mode of exercise, supervision, programme characteristics (session duration, frequency, programme duration), pain rating (absolute and relative), exercise starters, exercise completers and adherence to exercise sessions. Completion was defined as a percentage of participants that completed the exercise interventions from those that started the intervention. Adherence was defined as the percentage of exercise sessions completed. A relative pain rating was calculated based on the various pain scales identified throughout the studies which were converted into a percentage. For example, in a 5-point 0–4 claudication pain scale (0 = no pain; 4 = maximal pain) a rating of 3 on the scale would convert into 80% on the relative pain scale.
Data analysis
Exercise completion and adherence rates were determined for both traditional walking exercise groups and alternative exercise groups. Traditional walking programmes involved short intervals of walking until moderate to severe levels of pain were induced, interspersed with rest periods to allow the pain to subside. Alternative exercises included modalities of exercise (arm ergometer, resistance training, circuit training, lower limb aerobic exercise and polestriding) and walking exercises which did not produce moderate or severe pain and therefore do not conform with the aforementioned traditional exercise protocol.
The levels of pain either achieved or prescribed in the exercise interventions were also used to stratify studies that reported this characteristic, into low pain (<50% on the relative pain scale) or high pain (≥50%) cohorts.
Odds ratios (ORs) were determined for the completion rates of traditional and alternative exercise groups and chi-squared tests were performed to determine if differences in completion rates between the two were significant. These tests were also performed for high and low pain cohorts. Independent samples t-tests were performed to determine if adherence rates were significantly different between groups, with statistical significance set at P < 0.05.
Results
The search resulted in a total of 8324 records, of which 1510 were duplicates (see Figure 1). The remaining 6814 records were screened based on title and abstract prior to full-text review. Eighty-four records were determined to satisfy the inclusion criteria and were analysed. Of the 84 records, 39 records contained data on adherence; 56 of the records were RCTs, 22 were pre-post studies and six were controlled studies.
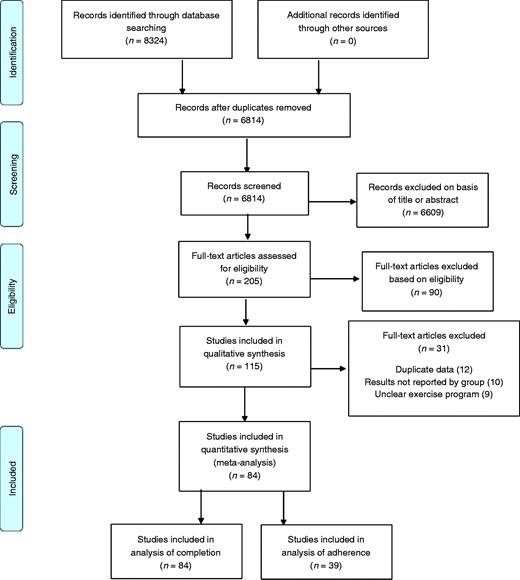
PRISMA flow diagram showing the process of identifying records eligible for review.
Quality assessment
The studies had an average PEDro score of 4.6 out of 10, with a range of 1–8. The scores were lowest in the categories of blinding (blind subjects, blind therapists and blind assessors), concealed allocation and intention to treat. A majority of studies satisfied the categories of randomisation, baseline comparison, between-group comparison, and point estimates and variability. ‘Eligibility’, although not included in the total PEDro score, was also satisfied in most of the studies. The ‘eligibility’ criterion is satisfied if the study describes a list of criteria used to determine eligibility for participation.
Subject and study characteristics
The 84 studies in the review included 4742 participants who were allocated into an exercise group and started the intervention. The average age of the participants was 66.7 years (excluding four studies that did not report average age). Overall, in studies that reported the number of men and women (n = 77), 70.5% of participants were men and 29.5% of participants were women. Out of the 84 studies, there was a total of 122 separate exercise groups. Within the 122 groups, 64 performed exercise that was defined as ‘traditional walking exercise’ and 58 performed exercise that was defined as ‘alternative exercise’. In the traditional walking exercise groups there were 2977 participants who started exercise. The average age for this cohort was 66.8 (range 57.9–76.3) years with 69.2% men and 30.8% women. In the alternative exercise groups, there were 1765 participants who started exercise. The average age for this cohort was 66.5 (range 53–78.8) years with 72.8% men and 27.2% women.
Exercise intervention characteristics
The different modalities of ‘alternative exercise’ included: circuit/combined exercise (n = 16), low pain/pain-free walking (n = 12), resistance training (n = 9), polestriding (n = 7), high-intensity (near-maximal speeds) walking (n = 4), upper limb ergometry (n = 4), lower limb ergometry (n = 3) and plantar flexion exercise (n = 3).
Out of the 122 exercise groups, 101 groups performed supervised exercise (traditional n = 47, alternative n = 54). Studies averaged 42.8 minutes (range 10–70) for session duration, a weekly frequency of 3.7 (1–21), and intervention duration of 18.4 weeks (6–56). Traditional programme durations (21.9 ± 12.8 weeks) were significantly longer (P = 0.001) compared to durations for alternative programmes (14.4 ± 7.0). Session durations and frequencies did not differ between programme types.
Completion rates and adherence rates
From the total 4742 participants who commenced exercise interventions, 3933 participants completed the entire exercise programme intervention. Stratified by traditional and alternative exercise structures, there were 2977 participants in traditional walking exercise interventions who commenced the interventions and 2405 participants who completed (completion rate 80.8% (range 54.2–100)). Among the studies that used alternative exercise modalities, 1765 participants commenced interventions and 1528 participants completed the interventions (completion rate 86.6% (range 60.0–100)). The odds of completion for traditional exercise were 4.20 and the odds of completion for alternative exercise were 6.45. Thus, participants were 1.53 times (OR) more likely to complete an alternative intervention compared to a traditional intervention. Performing a chi-squared test also demonstrated that the difference of completion rates between alternative exercise groups and traditional groups was statistically significant (χ2 18.8, P < 0.001) (Table 1).
| . | Completion rate (%) . | Adherence rate (%) . |
|---|---|---|
| Traditional exercise groups | 80.8 (range 54.2–100)* | 77.6 (range 57.1–100)† |
| Alternative exercise groups | 86.6 (range 60.0–100)* | 85.5 (range 66.7–100)† |
| High pain exercise groups | 81.0 (range 54.2–100)* | 77.0 (range 57.1–100)‡ |
| Low pain exercise groups | 86.6 (range 70.6–100)* | 93.4 (range 80.0–100)‡ |
| . | Completion rate (%) . | Adherence rate (%) . |
|---|---|---|
| Traditional exercise groups | 80.8 (range 54.2–100)* | 77.6 (range 57.1–100)† |
| Alternative exercise groups | 86.6 (range 60.0–100)* | 85.5 (range 66.7–100)† |
| High pain exercise groups | 81.0 (range 54.2–100)* | 77.0 (range 57.1–100)‡ |
| Low pain exercise groups | 86.6 (range 70.6–100)* | 93.4 (range 80.0–100)‡ |
*P < 0.001; †P = 0.02; ‡P = 0.004.
| . | Completion rate (%) . | Adherence rate (%) . |
|---|---|---|
| Traditional exercise groups | 80.8 (range 54.2–100)* | 77.6 (range 57.1–100)† |
| Alternative exercise groups | 86.6 (range 60.0–100)* | 85.5 (range 66.7–100)† |
| High pain exercise groups | 81.0 (range 54.2–100)* | 77.0 (range 57.1–100)‡ |
| Low pain exercise groups | 86.6 (range 70.6–100)* | 93.4 (range 80.0–100)‡ |
| . | Completion rate (%) . | Adherence rate (%) . |
|---|---|---|
| Traditional exercise groups | 80.8 (range 54.2–100)* | 77.6 (range 57.1–100)† |
| Alternative exercise groups | 86.6 (range 60.0–100)* | 85.5 (range 66.7–100)† |
| High pain exercise groups | 81.0 (range 54.2–100)* | 77.0 (range 57.1–100)‡ |
| Low pain exercise groups | 86.6 (range 70.6–100)* | 93.4 (range 80.0–100)‡ |
*P < 0.001; †P = 0.02; ‡P = 0.004.
Fifty-seven (traditional exercise groups 27; alternative exercise groups 30) of the 122 exercise groups also reported adherence rates to the exercise prescription. Average adherence rates for participants were significantly lower (P = 0.02) for traditional exercise groups (77.6%: 57.1–100%), compared to alternative exercise groups (85.5%: 66.7–100%).
Pain
Seventy-one (traditional exercise 46, alternative exercise 25) exercise groups included pain prescription/response associated with the exercise intervention as a characteristic of the exercise. Of the 19 groups belonging to the low pain cohort (<50% on relative pain scale), 100% (19/19) of the groups involved alternative exercise modalities. Of the 52 groups belonging to the high pain cohort (≥50% on relative pain scale), 88.5% (46/52) of the groups involved traditional walking exercise. Groups in the low pain cohort had an overall completion rate of 86.6% (range 70.6–100) and the odds of completing the programme in groups with low pain was 6.48. Groups in the high pain cohort had an overall completion rate of 81.0% (54.2–100) and the odds of completing the programme in groups with high pain was 4.27. Thus participants in the low pain cohort were 1.52 times (OR) more likely to complete the intervention compared to participants in the high pain cohort. The difference of completion rates between low pain exercise groups and high pain groups was statistically significant (χ2 9.05, P < 0.001). Adherence rates were reported for nine groups in the low pain cohort and were on average 93.4% (80.0–100), whereas adherence for the groups (n = 22) in the high pain cohort was lower with an average of 77.0% (57.1–100). Adherence rates, accounting for the number of participants per group, differed between traditional and alternative exercise groups (P = 0.004).
On analysing alternative exercise intervention groups classified in the high pain cohort (n = 6), the completion rate was 83.7% (60.0–88.3) and the adherence rate was 76.9% (only two groups reported adherence).
Reasons for non-completion
Of the studies (n = 51) that reported reasons for non-completion, ‘lack of motivation/interest’ was the most common reason (39.2%). Other common reasons included non-PAD/coronary artery disease (CAD)-related health issues (18.4%), family/work/transportation issues (13.9%) and CAD-related health issues (9.6%) (Table 2).
| Reasons . | No. of participants . | Percentage (%) . |
|---|---|---|
| Lack of motivation/interest | 277 | 39.2 |
| Non-PAD/CAD health issue | 130 | 18.4 |
| Family/work/transportation issues | 98 | 13.9 |
| CAD-related health issues | 68 | 9.6 |
| Other/unknown reasons | 62 | 8.8 |
| PAD progression/surgery | 45 | 6.4 |
| Death | 24 | 3.4 |
| Exercise programme-related reason | 2 | 0.3 |
| Total | 706 | 100 |
| Reasons . | No. of participants . | Percentage (%) . |
|---|---|---|
| Lack of motivation/interest | 277 | 39.2 |
| Non-PAD/CAD health issue | 130 | 18.4 |
| Family/work/transportation issues | 98 | 13.9 |
| CAD-related health issues | 68 | 9.6 |
| Other/unknown reasons | 62 | 8.8 |
| PAD progression/surgery | 45 | 6.4 |
| Death | 24 | 3.4 |
| Exercise programme-related reason | 2 | 0.3 |
| Total | 706 | 100 |
PAD: peripheral arterial disease; CAD: coronary artery disease.
| Reasons . | No. of participants . | Percentage (%) . |
|---|---|---|
| Lack of motivation/interest | 277 | 39.2 |
| Non-PAD/CAD health issue | 130 | 18.4 |
| Family/work/transportation issues | 98 | 13.9 |
| CAD-related health issues | 68 | 9.6 |
| Other/unknown reasons | 62 | 8.8 |
| PAD progression/surgery | 45 | 6.4 |
| Death | 24 | 3.4 |
| Exercise programme-related reason | 2 | 0.3 |
| Total | 706 | 100 |
| Reasons . | No. of participants . | Percentage (%) . |
|---|---|---|
| Lack of motivation/interest | 277 | 39.2 |
| Non-PAD/CAD health issue | 130 | 18.4 |
| Family/work/transportation issues | 98 | 13.9 |
| CAD-related health issues | 68 | 9.6 |
| Other/unknown reasons | 62 | 8.8 |
| PAD progression/surgery | 45 | 6.4 |
| Death | 24 | 3.4 |
| Exercise programme-related reason | 2 | 0.3 |
| Total | 706 | 100 |
PAD: peripheral arterial disease; CAD: coronary artery disease.
Discussion
Exercise is an effective form of treatment for patients with IC but only if patients are actively participating in physical activity programmes. Despite consistent evidence demonstrating the benefits of exercise for this patient population, participation rates in exercise programmes are far too low.19 To make matters worse, exercise adherence after the end of their intervention, in follow-up studies, is even lower.22 Thus the issue of exercise completion and adherence is important to address if patients with IC are to benefit from exercise. This review demonstrates that non-traditional exercise may be beneficial for patients with IC as adherence and programme completion rates are better compared to those for traditional exercise.
Patients with IC have been traditionally prescribed walking at a moderate pace until they reach near-maximal pain repeatedly, interspersed with periods of rest to allow the pain to subside. Walking exercise and achieving near-maximal levels of pain have long been believed to be two components necessary in exercise programmes for claudicants.23,24 The rationale behind these claims has been largely based on the first meta-analysis on exercise in claudicants over 20 years ago.10 More recent exploration in varying modalities of exercise for this population have shown alternative forms of exercise that stray from the traditional programme are also effective.11,12
Unsurprisingly, the type of exercise plays a role in completion and adherence rates to exercise in this population. Completion rates in programmes with alternative forms of exercise were 6% greater (80.8% vs. 86.6%) than programmes using traditional walking exercise. In addition, adherence to exercise was 8% greater (77.6% vs. 85.5%) in exercise interventions using alternative exercise compared to traditional exercise. These results suggest that traditional walking exercise is less likely to promote continued participation as the rates of completion and adherence are significantly lower. These results were maintained even when accounting for supervised and unsupervised exercise groups.
Pain played a significant role in the completion and adherence rates. Exercise groups performing low pain interventions had higher completion rates compared to groups performing high pain exercise. Although the concept of less pain equals greater participation may be intuitive, current practice still generally recommends patients to exercise to high levels of claudication pain.
No previous reviews have compared completion and adherence rates between traditional and alternative exercise in PAD. One previous review by Harwood (2016) explored the uptake and adherence rates to supervised exercise in this population.19 Uptake rates included the number of participants screened for interventions and the number subsequently allocated to exercise groups. Adherence rates represented the number of participants allocated into an exercise group and the number of participants that adequately completed the intervention. Out of the 4012 total participants from the studies that reported adherence, 3015 (75.1%) adequately completed the interventions, which is similar to the rates for traditional exercise we observed. The primary reasons for non-completion/adherence found in this review were similar to the previous review by Harwood (2016),25 and those reported for people with diabetes26 and comorbid musculoskeletal pain.27
Lower completion and adherence rates in traditional exercise programmes and high pain programmes can be viewed in light of the findings regarding barriers to physical activity among patients with IC. Using questionnaires28 and focus group interviews,29 researchers found the most prevalent personal barriers to exercise were ‘exercise-induced pain’ and ‘the need to rest because of leg pain’. The need to rest because of leg pain was also associated with lower levels of physical activity. Thus exercise programmes that involve exercising to severe levels of pain serve as a barrier to continued activity for this population. Lack of clear and accurate knowledge regarding claudication symptoms among patients may underlie the poor adherence to traditional/pain-inducing exercise. A study on pain-related beliefs in patients with IC concluded that the benefits of exercise for claudication were not fully understood by patients.20 Most patients believed exercise was the cause of claudication and that physical activity would not only make the pain worse but also harm their legs. The study concluded that healthcare providers were not adequately explaining the true value of exercise due to their own lack of understanding of ‘the subjective nature of pain’.
Certain limitations exist with this current review. The relationship between the available measures of adherence and completion is problematic. If 100% completion is reported for a study, but compliance to actual exercise sessions was not reported, it is possible that participants only completed the term of the intervention but did not attend all exercise sessions. Similarly, adherence rates can be unclear as it is possible that some studies reported 100% adherence to sessions attended but only half of the participants completed the entire intervention. In both cases, exercise participation can be falsely perceived due to lack of clear reporting. Improved reporting of adherence and completion rates, as well as reasons for drop out, would strengthen the validity of exercise studies and their findings.30 Higher standards need to be implemented to ensure systematic methods of reporting.
Another potential limitation is the inclusion of studies using unsupervised exercise. Various studies have indicated that supervised exercise is superior to unsupervised exercise with regard to improving treadmill performance31 and promoting physiological changes.32 However, unsupervised exercise is still effective in eliciting improvements in walking ability and daily activity levels,33 while having potential implications for improving adherence.34 Thus even if supervised exercise is more effective, as long as unsupervised exercise provides benefit, with the chance of greater adherence, it should be included as a viable option.
An additional limitation is the lack of female representation in these interventions. Even though the prevalence of the disease is similar between sexes,35 women are underrepresented in exercise intervention studies of patients with PAD (<30% of participants were women in the current review) and in cardiac rehabilitation programmes.36 Previous studies indicate this problem is due to a combination of practitioners not referring as many female patients and unique barriers to exercise that women experience.37 The lack of studies that directly compare alternative and traditional exercise programmes also prevents a stronger comparison between the two modalities. Studies vary in exercise programme characteristics (i.e. frequency, programme duration, session duration) making it harder to draw definitive conclusions.
This review has important clinical implications with regard to future research as well as clinical practice. First and foremost, patient education needs to dispel the myth that walking worsens their condition.38 There is a need to help patients better address symptom beliefs and outcome expectations. From a practitioner's standpoint, greater understanding of the subjective nature of pain in this population needs to be achieved. Not only does pain severity and perception differ among patients, but barriers to exercise also differ.39 Beyond patient and practitioner education, there may need to be changes made to the current fixation on a single form of exercise for IC patients. Guidelines have historically held steadfast to the idea that walking exercise should involve high levels of pain as the only method of exercise that can lead to significant improvements. Alternative methods of exercise are just as effective as traditional, and this review shows additional benefits through adherence. In addition, pain may not be a necessary component of an exercise programme. Low pain or pain-free interventions have produced meaningful improvements in patients with IC, and this review shows adherence to these interventions is greater than higher pain exercise programmes. Fortunately, the most recent guideline8 and scientific statement40 on PAD care has opened up to the idea of pain-free and alternative exercise modalities. However, there is still work to be done in order to ensure practitioners are implementing these changes.
A RCT that directly measures adherence and completion of traditional versus alternative exercise would be informative. It will also be useful to understand which components of the different programmes lead to greater adherence. Qualitative studies focused on the enjoyment and affect aspect of exercise in this population will be invaluable. More research exploring alternative modalities should be performed to validate further their efficacy and result in modifications to PAD management guidelines. Finally, future studies involving exercise interventions for patients with IC should consider clearly reporting adherence and completion rates.
Conclusion
This review found greater adherence to alternative exercise compared to traditional, painful exercise. Exercise as a beneficial method of therapy is no longer a subject of contention, rather the issue is now to figure out how to enable greater exercise participation. As further emphasis is being placed on patient perspectives, treatment of debilitating conditions such as IC must involve methods that are not only effective, but also provide patients with an opportunity to succeed.
Author contribution
EL and SGT conceived the study. EL conducted the literature search. Titles, abstracts and papers were screened, and data extraction was performed by EL and CHN. EL performed the statistical analysis and drafted the manuscript. SGT and CHN critically revised the manuscript. All authors approved the final manuscript and are accountable to all aspects of the work. All authors take responsibility for aspects regarding reliability and freedom from bias of presented data and subsequent interpretation.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
Presented in poster format at the 2018 Canadian Society for Exercise Physiology Conference in Niagara Fall, Ontario, Canada.




Comments